
PHYSICIAN’S GU IDE TO
Assessing and Counseling
Older Drivers
2nd edition
The information in this guide is provided to assist physicians in evaluating
the ability of their older patients to operate motor vehicles safely as part of
their everyday, personal activities. Evaluating the ability of patients to operate
commercial vehicles or to function as professional drivers involves more
stringent criteria and is beyond the scope of this publication.
This guide is not intended as a standard of medical care, nor should it be used
as a substitute for physicians’ clinical judgement. Rather, this guide reects the
scientic literature and views of experts as of December 2009, and is provided
for informational and educational purposes only. None of this guide’s materials
should be construed as legal advice nor used to resolve legal problems. If legal
advice is required, physicians are urged to consult an attorney who is licensed to
practice in their state.
Material from this guide may be reproduced. However, the authors of this
guide strongly discourage changes to the content, as it has undergone rigorous,
comprehensive review by medical specialists and other experts in the eld of
older driver safety.
The American Medical Association is accredited by the Accreditation Council
for Continuing Medical Education to provide continuing medical education
(CME) for physicians.
The American Medical Association designates this educational activity for a
maximum of 6.25 AMA PRA Category 1 Credits™. Physicians should only claim
credit commensurate with the extent of their participation in the activity.
Additional copies of the guide can be downloaded or ordered online at the
AMA’s Older Driver’s Project Web site: www.ama-assn.org/go/olderdrivers.
For further information about the guide,
please contact:
Joanne G. Schwartzberg, MD
Director, Aging and Community Health
American Medical Association
515 N. State Street
Chicago, IL 60654
Physician’s Guide
to Assessing and
Counseling Older Drivers
An AMA Continuing Education Program
First Edition Original Release Date–7/30/2003
Second Edition–2/3/2010
Expiration Date–2/3/2012
Accreditation Statement
The American Medical Association is accredited
by the Accreditation Council for Continuing
Medical Education to provide continuing medical
education for physicians.
Designation Statement
The American Medical Association designates
this educational activity for a maximum of 6.25
AMA PRA Category 1 Credits
TM
. Physicians
should only claim credit commensurate with the
extent of their participation in the activity.
Disclosure Statement
The content of this activity does not relate to
any product of a commercial interest as dened
by the ACCME; therefore, there are no relevant
nancial relationships to disclose.
Educational Activity Objectives
• Increase physician awareness of the safety risks
of older drivers as a public health issue
• Identify patients who may be at risk for unsafe
driving
• Use various clinical screens to assess patients’
level of function for driving tness
• Employ referral and treatment options for
patients who are no longer t to drive
• Practice counseling techniques for patients who
are no longer t to drive
• Demonstrate familiarity with State reporting
laws and legal/ethical issues surrounding
patients who may not be safe on the road
Instructions for claiming AMA PRA
Category 1 Credits™
To facilitate the learning process, we encourage
the following method for physician participation:
Read the material in the Physician’s Guide to
Assessing and Counseling Older Drivers, complete
the CME Questionnaire & Evaluation, and then
mail both of them to the address provided. To
earn the maximum 6.25 AMA PRA Category 1
Credits™ , 70 percent is required to pass and
receive the credit.
IV Acknowledgements
Acknowledgements
This Physician’s Guide to Assessing and
Counseling Older Drivers is the product
of a cooperative agreement between
the American Medical Association and
the National Highway Trafc Safety
Administration.
First edition: Primary Authors
Claire C. Wang, MD
American Medical Association
Catherine J. Kosinski, MSW
American Medical Association
Joanne G. Schwartzberg, MD
American Medical Association
Anne Shanklin, MA
American Medical Association
Second edition:
Principal Faculty Authors
Editor: David B. Carr, MD
Associate Professor of Medicine and
Neurology Washington University at
St. Louis Clinical Director
Planning Committee:
David B. Carr, MD;
Associate Professor of Medicine and
Neurology Washington University at
St. Louis Clinical Director
Joanne G. Schwartzberg, MD
Director, Aging and Community Health,
American Medical Association
Lela Manning, MPH, MBA
Project Coordinator, American Medical
Association
Jessica Sempek, MS
Program Administrator, American Medical
Asscoiation
Citation
Carr DB; Schwartzberg JG; Manning
L; Sempek J; Physician’s Guide to
Assessing and Counseling Older
Drivers, 2nd edition, Washington,
D.C. NHTSA. 2010.
This guide beneted signicantly
from the expertise of the following
individuals who served as reviewers
in this project.
Second edition: Content Consultants
Lori C. Cohen
AARP
Senior Project Manager, Driver Safety
Jami Croston, OTD
Washington University at St. Louis
T. Bella Dinh-Zarr, PhD, MPH
Road Safety Director, FIA Foundation
North American Director, MAKE
ROADS SAFE–The Campaign for Global
Road Safety
John W. Eberhard, PhD
Consultant, Aging and Senior
Transportation Issues
Camille Fitzpatrick, MSN, NP
University of California Irvine
Clinical Professor Family Medicine
Mitchell A. Garber, MD,
MPH, MSME
National Transportation Safety Board
Medical Ofcer
Anne Hegberg, MS, OTR/L
Marionjoy Rehabilitation Hospital
Certied Driver Rehabilitation Specialist
Patti Y. Horsley, MPH
Center for Injury Prevention
Policy and Practice
SDSU EPIC Branch
California Department of Public Health
Linda Hunt, OTR/L, PhD
Pacic University
School of Occupational Therapy
Associate Professor
Jack Joyce
Maryland Motor Vehicle Administration
Driver Safety Research Ofce
Senior Research Associate
Karin Kleinhans OTR/L
Sierra Nevada Memorial Hospital
Center for Injury Prevention Policy &
Practice
Occupational Therapy Association of
California
Kathryn MacLean, MSW
St. Louis University
Mangadhara R. Madineedi, MD, MSA
Harvard Medical School
Instructor in Medicine
VA Boston Healthcare System
Director, Geriatrics & Extended Care
Service Line
Richard Marottoli, MD, MPH
American Geriatrics Society
John C. Morris
Professor of Neurology
Washington University School of Medicine
Germaine L. Odenheimer, MD
VAMC
Donald W. Reynolds Department of
Geriatric Medicine
Associate Professor
Alice Pomidor, MD, MPH
Florida State University College of
Medicine
Associate Professor, Department of
Geriatrics
Kanika Mehta Rankin
Loyola University Chicago School of Law
(2nd year) Juris Doctorate Candidate,
2011
Yael Raz, MD
American Academy of Otolaryngology
William H. Roccaforte, MD
American Association for Geriatric
Psychiatry
Nebraska Medical Center
Department of Psychiatry
Gayle San Marco, OTR/L, CDRS
Northridge Hospital Medical Center
Project Consultation, Center for Injury
Prevention Policy & Practice
Freddie Segal-Gidan, PA-C, PhD
American Geriatrics Society
William Shea, OTR/L
Fairlawn Rehabilitation Hospital
VAcknowledgements
Patricia E. Sokol, RN, JD
Senior Poilcy Analyst, Patient Safety
American Medical Association
Esther Wagner, MA
National Highway Trafc Safety
Administration
First edition: Advisory Panel
Sharon Allison-Ottey, MD
National Medical Association
Joseph D. Bloom, MD
American Psychiatric Association
Audrey Rhodes Boyd, MD
American Academy of Family Physicians
David B. Carr, MD
Washington University School of Medicine
Bonnie M. Dobbs, PhD
University of Alberta
Association for the Advancement of
Automotive Medicine
John Eberhard, PhD
National Highway Trafc Safety
Administration
Laurie Flaherty, RN, MS
National Highway Trafc Safety
Administration
Arthur M. Gershkoff, MD
American Academy of Physical
Medicine and Rehabilitation
Brian Greenberg, MEd
American Association of Retired Persons
Lynne M. Kirk, MD, FACP
American College of Physicians –
American Society of Internal Medicine
Marian C. Limacher, MD, FACC,
FSGC
American College of Cardiology
Society of Geriatric Cardiology
Richard Marottoli, MD, MPH
American Geriatrics Society
Lylas G. Mogk, MD
American Academy of Ophthalmology
John C. Morris, MD
American Academy of Neurology
Alzheimer’s Association
James O’Hanlon, PhD
Tri-Counties Regional Center
Cynthia Owsley, PhD, MSPH
University of Alabama at Birmingham
Robert Raleigh, MD
Maryland Department of Transportation
William Roccaforte, MD
American Association for Geriatric
Psychiatry
Jose R. Santana Jr., MD, MPH
National Hispanic Medical Association
Melvyn L. Sterling, MD, FACP
Council on Scientic Affairs
American Medical Association
Jane Stutts, PhD
University of North Carolina Highway
Safety Research Center
First edition: Review Committee
Geri Adler, MSW, PhD
Minneapolis Geriatric Research Education
Clinical Center
Reva Adler, MD
American Geriatrics Society
Elizabeth Alicandri
Federal Highway Administration
Paul J. Andreason, MD
Food and Drug Administration
Mike Bailey
Oklahoma Department of Public Safety
Robin Barr, PhD
National Institute on Aging
Arlene Bierman, MD, MS
Agency for Healthcare Research
and Quality
Carol Bodenheimer, MD
American Academy of Physical Medicine
and Rehabilitation
Jennifer Bottomley, PhD, MS, PT
American Physical Therapy Association
Thomas A. Cavalieri, DO
American Osteopathic Association
Lori Cohen
American Association of Motor Vehicle
Administrators
Joseph Coughlin, PhD
Gerontological Society of America
T. Bella Dinh-Zarr, PhD, MPH
AAA
Barbara Du Bois, PhD
National Resources Center on Aging
and Injury
Leonard Evans, PhD
Science Serving Society
Connie Evaschwick, ScD., FACHE
American Public Health Association
Jeff Finn, MA
American Occupational Therapy
Association
Jaime Fitten, MD
UCLA School of Medicine
Marshall Flax, MA
Association for the Education and
Rehabilitation of the Blind and
Visually Impaired
Linda Ford, MD
Nebraska Medical Association
Barbara Freund, PhD
Eastern Virginia Medical School
Mitchell Garber, MD, MPH, MSME
National Transportation Safety Board
Andrea Gilbert, COTA/L
Rehabilitation Institute of Chicago
Claudia Grimm, MSW
Oregon Department of Transportation
Kent Higgins, PhD
Lighthouse International
VI Acknowledgements
Linda Hunt, PhD, OTR/L
Maryville University
Mary Janke, PhD
California Department of Motor Vehicles
Gary Kay, PhD
Washington Neuropsychological Institute
Shara Lynn Kelsey
Research and Development
California Department of Motor Vehicles
Susan Kirinich
National Highway Trafc Safety
Administration
Donald Kline, PhD
University of Calgary
Philip LePore, MS
New York State Ofce for the Aging
Sandra Lesikar, PhD
US Army Center for Health Promotion
and Preventive Medicine
William Mann, OTR, PhD
University of Florida
Dennis McCarthy, MEd, OTR/L
University of Florida
Gerald McGwin, PhD
University of Alabama
Michael Mello, MD, FACEP
American College of Emergency Physicians
Barbara Messinger-Rapport, MD, PhD
Cleveland Clinic Foundation
Alison Moore, MD, MPH
American Public Health Association
David Geffen School of Medicine,
University of California
Anne Long Morris, EdD, OTR/L
American Society on Aging
Germaine Odenheimer, MD
Center for Assessment and Rehabilitation
of Elderly Drivers
Eli Peli, M.Sc., OD
Schepens Eye Research Institute
Alice Pomidor, MD, MPH
Society of Teachers of Family Medicine
George Rebok, MA, PhD
Johns Hopkins School of Hygiene and
Public Health
Selma Sauls
Florida Department of Highway Safety and
Motor Vehicles
Susan Samson
Pinellas/Pasco Area Agency on Aging
Steven Schachter, MD
Epilepsy Foundation
Frank Schieber, PhD
University of South Dakota
Freddi Segal-Gidan, PA, PhD
American Geriatrics Society
Melvin Shipp, OD, MPH, DrPh
University of Alabama at Birmingham
Richard Sims, MD
American Geriatrics Society
Kristen Snyder, MD
Oregon Health & Science University
School of Medicine
Susan Standfast, MD, MPH
American College of Preventative Medicine
Holly Stanley, MD
American Geriatrics Society
Loren Staplin, PhD
Transanalytics and Texas Transportation
Institute
Wendy Stav, PhD, OTR, CDRS
American Occupational Therapy
Association
Cleveland State University
Donna Stressel, OTR, CDRS
Association of Driver Rehabilitation
Specialists
Cathi A. Thomas, RN, MS
Boston University Medical Center
American Parkinson Disease Association
John Tongue, MD
American Academy of Orthopedic Surgery
Patricia Waller, PhD
University of Michigan
Lisa Yagoda, MSW, ACSW
National Association of Social Workers
Patti Yanochko, MPH
San Diego State University
Richard Zorowitz, MD
National Stroke Association

VIITable of Contents
Table of Contents
Preface .................................................................................................................................. IX
Chapter 1 .................................................................................................................................1
Safety and the Older Driver With Functional or Medical Impairments: An Overview
Chapter 2 ...............................................................................................................................11
Is the Patient at Increased Risk for Unsafe Driving?
Red Flags for Further Assessment
Chapter 3 ...............................................................................................................................19
Assessing Functional Ability
Chapter 4 ...............................................................................................................................33
Physician Interventions
Chapter 5 ...............................................................................................................................41
The Driver Rehabilitation Specialist
Chapter 6 ...............................................................................................................................49
Counseling the Patient Who is no Longer Safe to Drive
Chapter 7 ...............................................................................................................................59
Ethical and Legal Responsibilities of the Physician
Chapter 8 ...............................................................................................................................69
State Licensing and Reporting Laws
Chapter 9 .............................................................................................................................145
Medical Conditions and Medications That May Affect Driving
Chapter 10 ...........................................................................................................................187
Moving Beyond This Guide: Future Plans to Meet the Transportation Needs of Older Adults
Appendix A ..........................................................................................................................197
CPT
®
Codes

VIII Table of Contents
Table of Contents (continued)
Appendix B ..........................................................................................................................201
Patient and Caregiver Educational Materials
Am I a Safe Driver? ....................................................................................................................... 203
Successful Aging Tips .................................................................................................................. 205
Tips for Safe Driving ...................................................................................................................... 207
How to Assist the Older Driver ...................................................................................................... 209
Getting By Without Driving ............................................................................................................ 213
Where Can I Find More Information? ............................................................................................. 215
Appendix C ..........................................................................................................................221
Continuing Medical Education Questionnaire and Evaluation
Physicians Guide to Assessing and Counseling Older Drivers ....................................................... 221
Continuing Medical Education Evaluation Form ............................................................................. 224
Index ....................................................................................................................................229

IXPreface
Preface
The science of public health and the practice of medicine are often deemed two
separate entities. After all, the practice of medicine centers on the treatment of
disease in the individual, while the science of public health is devoted to preven-
tion of disease in the population. However, physicians can actualize public health
priorities through the delivery of medical care to their individual patients.
One of these priorities is the prevention of injury. More than 400 Americans
die each day as a result of injuries sustained from motor vehicle crashes, rearms,
poisonings, suffocation, falls, res, and drowning. The risk of injury is so great
that most people sustain a signicant injury at some time during their lives.
The Physician’s Guide to Assessing and Counseling Older Drivers was created by
the American Medical Association (AMA), with support from the National
Highway Trafc and Safety Administration (NHTSA), to help physicians
address preventable injuries—in particular, those incurred in motor vehicle
crashes. Currently, motor vehicle injuries are the leading cause of injury-related
deaths among 65- to 74-year-olds and are the second leading cause (after falls)
among 75- to 84-year-olds. While trafc safety programs have reduced the fatal-
ity rate for drivers under age 65, the fatality rate for older drivers has consistently
remained high. Clearly, additional efforts are needed.
Physicians are in a leading position to address and correct this health disparity.
By providing effective health care, physicians can help their patients maintain
a high level of tness, enabling them to preserve safe driving skills later in life
and protecting them against serious injuries in the event of a crash. By adopting
preventive practices—including the assessment and counseling strategies outlined
in this guide—physicians can better identify drivers at risk for crashes, help
enhance their driving safety, and ease the transition to driving retirement if
and when it becomes necessary.
Through the practice of medicine, physicians have the opportunity to promote
the safety of their patients and of the public. The AMA and NHTSA urge you
to use the tools in this Physician’s Guide to Assessing and Counseling Older Drivers
to forge a link between public health and medicine.
The project was supported by cooperative agreement number DTNH22-08-H-00185
from the National Highway Trafc Safety Administration (NHTSA) of the Department
of Transportation. While this guide was reviewed by NHTSA, the contents of this guide
are those of the authors and do not represent the opinions, policies or ofcial positions
of NHTSA.

CHAPTER 1
Safety and the Older Driver
With Functional or Medical
Impairments: An Overview
1
Chapter 1—Safety and the Older Driver With Functional or Medical Impairments: An Overview
Patients like Mrs. Simon and Mr. Evans
are becoming more common in physi-
cians’ practices. Buoyed by the large
ranks of “baby boomers” and increased
life expectancy, the U.S. older adult
population is growing nearly twice as
fast as the total population.
1,2
Within
this cohort of older adults, an increasing
proportion will be licensed to drive, and
it is expected that these license-holders
will drive more miles than older drivers
do today.
3
As the number of older drivers with
medical conditions expands, patients
and their families will increasingly
turn to physicians for guidance on safe
driving. Physicians will have the chal-
lenge of balancing their patients’ safety
against their transportation needs and
the safety of society.
This guide is intended to help you
answer the questions, “At what level of
severity do medical conditions impair
safe driving?” “What can I do to help
my patient drive more safely?”
*
, and if
necessary to help you counsel patients
1. National Center for Statistics & Analysis.
Trafc Safety Facts 2000: Older Population.
DOT HS 809 328. Washington, DC: National
Highway Trafc Safety Administration.
2. Population Projections of the United States by
Age, Sex, Race, Hispanic, Origin, and Nativity:
1999 to 2100. Population Projections Program,
Population Division, Census Bureau Internet
release date: January 13, 2000. Revised date:
February 14, 2000. Suitland, MD: U.S.
Census Bureau.
3. Eberhard, J. Safe Mobility for Senior Citizens.
International Association for Trafc and Safety
Services Research. 20(1):29–37.
Mrs. Simon, a 67-year-old woman
with type 2 diabetes mellitus and
hypertension, mentions during a
routine check-up that she almost
hit a car while making a left-hand
turn when driving two weeks ago.
Although she was uninjured, she
has been anxious about driving since
that episode. Her daughter has
called your ofce expressing concern
about her mother’s driving abilities.
Mrs. Simons admits to feeling less
condent when driving and wants
to know if you think she should stop
driving. What is your opinion?
Mr. Evans, a 72-year-old man
with coronary artery disease and
congestive heart failure, arrives for
an ofce visit after fainting yesterday
and reports complaints of “light-
headedness” for the past two weeks.
When feeling his pulse, you notice
that his heartbeat is irregular. You
perform a careful history and physi-
cal examination, and order some
laboratory tests to help determine the
cause of his atrial brillation. When
you ask Mr. Evans to schedule a
follow-up appointment for the next
week, he tells you he cannot come
at that time because he is about to
embark on a two-day road trip to
visit his daughter and newborn
grandson. Would you address the
driving issue and if so, how?
What would you communicate to
the patient?
CHAPTER 1
Safety and the Older
Driver With Functional
or Medical Impairments
An Overview
about driving cessation and alternate
means of transportation. Mobility
counseling and discussing alternative
modes of transportation need to take a
more prominent role in the physician’s
ofce. To these ends, we have reviewed
the scientic literature and collaborated
with clinicians and experts in this eld
to produce the following physician tools:
• An ofce-based assessment of
medical tness to drive. This
assessment is outlined in the
algorithm, Physician’s Plan for
Older Drivers’ Safety (PPODS),
presented later in this chapter.
• A functional assessment battery,
the Assessment of Driving Related
Skills (ADReS). This can be found
in Chapter 3.
• A reference table of medical
conditions and medications that
may affect driving, with specic
recommendations for each, can
be found in Chapter 9.
In addition to these tools, we also
present the following resources:
• Information to help you navigate
the legal and ethical issues regarding
patient driving safety. Information
* Please be aware that the information in this
guide is provided to assist physicians in evaluat-
ing the ability of their older patients to operate
motor vehicles safely as part of their everyday,
personal activities. Evaluating the ability of
patients to operate commercial vehicles or to
function as professional drivers involves more
stringent criteria and is beyond the scope of this
guide.

2 Chapter 1—Safety and the Older Driver With Functional or Medical Impairments: An Overview
on patient reporting, with a state-by-
state list of licensing criteria, license
renewal criteria, reporting laws,
and Department of Motor Vehicles
(DMV) contact information, can be
found in Chapters 7 and 8.
• Recommended Current Procedural
Terminology (CPT
®
) codes for
assessment and counseling procedures.
These can be found in Appendix A.
• Handouts for your patients and their
family members. These handouts,
located in Appendix B, include a self-
screening tool for driving safety, safe
driving tips, driving alternatives, and
a resource sheet for concerned family
members. These handouts can be
removed from the guide and photo-
copied for distribution to patients
and their family members.
We understand that physicians may
lack expertise in communicating with
patients about driving, discussing the
need for driving cessation (delivering
bad news), and being aware of viable
alternative transportation options to
offer. Physicians also may be concerned
about dealing with the patient’s anger,
or even losing contact with the patient.
Driving is a sensitive subject, and the
loss of driving privileges can be stressful.
While these are reasonable concerns,
there are ways to minimize the impact
on the doctor-patient relationship when
discussing driving. We provide sample
approaches in subsequent chapters in
the areas of driving assessment, rehabili-
tation, restriction, and cessation.
We want this information to be
readily accessible to you and your
ofce staff. You can locate this guide
on the Internet at the AMA Web site
(www.ama-assn.org/go/olderdrivers).
Additional printed copies may also
be ordered through the Web site.
Before you read the rest of the guide,
you may wish to familiarize yourself
with key facts about older drivers.
Older drivers: Key facts
Fact #1: The number of older adult
drivers is growing rapidly and they
are driving longer distances.
Life expectancy is at an all-time high
4
and the older population is rap-
idly increasing. By the year 2030, the
population of adults older than 65 will
more than double to approximately 70
million, making up 20 percent of the
total U.S. population.
5
In many States,
including Florida and California, the
population of those over age 65 may
reach 20 percent in this decade The
fastest growing segment of the popula-
tion is the 80-and-older group, which
is anticipated to increase from about 3
million this year to 8 to 10 million over
the next 30 years. We can anticipate
many older drivers on the roadways
over the next few decades, and your
patients will likely be among them.
Census projections estimate that by
the year 2020 there will be 53 million
persons over age 65 and approximately
40 million (75%) of those will be
licensed drivers.
6
The increase in the
number of older drivers is due to many
factors. In addition to the general aging
of the population that is occurring in
all developed countries, many more
female drivers are driving into advanced
age. This will likely increase with aging
cohorts such as the baby boomers.
In addition, the United States has
become a highly mobile society, and
older adults are using automobiles for
volunteer activities and gainful employ-
ment, social and recreational needs,
and cross country travel. Recent studies
suggest that older adults are driving
4. Centers for Disease Control and Prevention.
2008. National Center for Health Statistics.
Accessed on December 14, 2008 at;
www.cdc.gov/nchs/PRESSROOM/
07newsreleases/lifeexpectancy.htm
5. U.S. Census Bureau, Healthy Aging, 2008.
Accessed on December 14, 2008 at; www.cdc.
gov/NCCdphp/publications/aag/aging.htm
6. U.S. Census Bureau. Projection of total resident
population by 5-year age groups and sex with
special age categories; middle series, 2016–2020.
Washington, DC: Population Projections
Program, Population Division, U.S. Census
Bureau; 2000.
more frequently, while transportation
surveys reveal an increasing number of
miles driven per year for each successive
aging cohort.
Fact #2: Driving cessation is inevi-
table for many and can be associated
with negative outcomes.
Driving can be crucial for performing
necessary chores and maintaining social
connectedness, with the latter having
strong correlates with mental and physi-
cal health.
7
Many older adults continue
to work past retirement age or engage in
volunteer work or other organized ac-
tivities. In most cases, driving is the pre-
ferred means of transportation. In some
rural or suburban areas, driving may be
the sole means of transportation. Just as
the driver’s license is a symbol of inde-
pendence for adolescents, the ability to
continue driving may mean continued
mobility and independence for older
drivers, with great effects on their qual-
ity of life and self-esteem.
8
In a survey of 2,422 adults 50 and older,
86 percent of survey participants report-
ed that driving was their usual mode of
transportation. Within this group, driv-
ing was the usual method of transporta-
tion for 85 percent of participants 75 to
79, 78 percent of participants 80 to 84,
and 60 percent of participant’s 85 and
older.
9
This data also indicates that the
probability of losing the ability to drive
increases with advanced age. It is esti-
mated that the average male will have
6 years without the functional ability to
drive a car and the average female will
have 10 years.
10
However, our society
has not prepared the public for driving
7. Berkman, L. F., Glass, T., Brissette, I., & See-
man, T. E. From social integration to health:
Durkheim in the new millennium. Soc Sci Med.
51:843–857.
8. Stutts, J. C. Do older drivers with visual and
cognitive impairments drive less? J Am Geriatr
Soc. 46(7):854–861.
9. Ritter, A. S., Straight, A., & Evans, E.
Understanding Senior Transportation: Report
and Analysis of a Survey of Consumers Age
50+. American Association for Retired Persons,
Policy and Strategy Group, Public Policy
Institute, p. 10–11.
10. Foley, D. J., Heimovitz, H. K., Guralnik, J., &
Brock, D. B. Driving life expectancy of persons
aged 70 years and older in the United States.
Am J Public Health. 92:1284–1289
3Chapter 1—Safety and the Older Driver With Functional or Medical Impairments: An Overview
cessation, and patients and physicians
are often ill-prepared when that time
comes.
Studies of driving cessation have noted
increased social isolation, decreased
out-of-home activities,
11
and an in-
crease in depressive symptoms.
12
These
outcomes have been well documented
and represent some of the negative con-
sequences of driving cessation. It is im-
portant for health care providers to use
the available resources and professionals
who can assist with transportation to
allow their patients to maintain inde-
pendence. These issues will be discussed
further in subsequent chapters.
Fact #3: Many older drivers
successfully self-regulate their
driving behavior.
As drivers age, they may begin to
feel limited by slower reaction times,
chronic health problems, and effects
from medications. Although transporta-
tion surveys over the years document
that the current cohort of older driv-
ers is driving farther, in later life many
reduce their mileage or stop driving
altogether because they feel unsafe or
lose condence. In 1990, males over 70
drove on average 8,298 miles, compared
with 16,784 miles for men 20 to 24; for
women, the gures were 3,976 miles
and 11,807 miles, respectively.
13
Older
drivers are more likely to wear seat belts
and are less likely to drive at night,
speed, tailgate, consume alcohol prior
to driving, and engage in other risky
behaviors.
14
Older drivers not only drive substan-
tially less, but also tend to modify
11. Marottoli, R. A., de Leon, C. F. M., & Glass,
T. A., et al. Consequences of driving cessation:
decreased out-of-home activity levels. J Gerontol
Series B Psychol Sci Soc Sci. 55:S334–340.
12. Ragland, D. R., Satariano, W. A,. & MacLeod,
K. E. Driving cessation and increased depressive
symptoms J Gerontol Series A Bio Sci Med Sci.
60:399–403.
13. Evans, L. How safe were today’s older drivers
when they were younger? Am J Epidemiol.
1993;137(7);769–775.
14. Lyman, J. M., McGwin, G., &Sims, R.V. Factors
related to driving difculty and habits in older
drivers. Accid Anal Prev. 33:413–421.
when and how they drive. When they
recognize loss of ability to see well after
dark, many stop driving at night. There
are data that suggest older women are
more likely to self-regulate than men.
15
Others who understand the complex
demands of left turns at uncontrolled
intersections and their own diminished
capacity forgo left-hand turns, and
make a series of right turns instead. Self-
regulating in response to impairments
is simply a continuation of the strategy
we all employ daily in navigating this
dangerous environment—driving. Each
of us, throughout life, is expected to
use our best judgment and not operate
a car when we are impaired, whether
by fatigue, emotional distress, physical
illness, or alcohol. Thus, self-awareness,
knowledge of useful strategies, and
encouragement to use them may be
sufcient among cognitively intact
older adults; however, this remains an
important area for further study.
Older drivers may reduce their mile-
age by eliminating long highway trips.
However, local roads often have more
hazards in the form of signs, signals,
trafc congestion, and confusing inter-
sections. Decreasing mileage, then, may
not always proportionately decrease
safety risks.
16
In fact, the “low mileage”
drivers (e.g., less than 3,000 miles per
year) may actually be the group that is
most “at-risk.”
17
Despite all these self-regulating mea-
sures, motor vehicle crash rates per mile
driven begin to increase at age 65.
18
On
a case-by-case level, the risk of a crash
depends on whether each individual
driver’s decreased mileage and behavior
15. Kostyniuk, L. P., & Molnar, L. J. Self-regulatory
driving practices among older adults: health, age
and sex effects. Accid Anal Prev. 40: 1576–1580.
16. Janke, M. K. Accidents, mileage, and the exag-
geration of risk. Accid Anal Prev. 1991;23:183–
188.
17. Langford, J., Methorst, R., & Hakamies-
Blomqvist, L. Older drivers do not have a high
crash risk—a replication of low mileage bias.’
Accid Anal Prev. 38(3):574–578.
18. Li, G., Braver, E. R., & Chen, L. H. Exploring
the High Driver Death Rates per Vehicle-Mile
of Travel in Older Drivers: Fragility versus
Excessive Crash Involvement. Presented at the
Insurance Institute for Highway Safety; August
2001.
modications are sufcient to counter-
balance any decline in driving ability.
In some cases, decline—in the form of
peripheral vision loss, for example—
may occur so insidiously that the driver
is not aware of it until he/she experi-
ences a crash. In fact, a recent study
indicated that some older adults do not
restrict their driving despite having
signicant visual decits.
19
Reliance on
driving as the sole available means of
transportation can result in an unfortu-
nate choice between poor options. In
the case of dementia, drivers may lack
the insight to realize they are unsafe
to drive.
In a series of focus groups conducted
with older adults who had stopped
driving within the past ve years, about
40 percent of the participants knew
someone over age 65 who had problems
with his/her driving but was still behind
the wheel.
20
Clearly, some older drivers
require outside assessment and interven-
tions when it comes to driving safety.
Fact #4: The crash rate for older
drivers is in part related to physical
and/or mental changes associated
with aging and/or disease.
21
Compared with younger drivers whose
car crashes are often due to inexperi-
ence or risky behaviors,
22
older driver
crashes tend to be related to inattention
or slowed speed of visual processing.
23
Older driver crashes are often multiple-
vehicle events that occur at intersections
and involve left-hand turns. The crash is
usually caused by the older driver’s failure
to heed signs and grant the right-of-way.
At intersections with trafc signals, left-
19. Okonkwo, O. C., Crowe, M., Wadley, V. G.,
& Ball, K. Visual attention and self-regulation
of driving among older adults. Int Psychogeriatr.
20:162–173.
20. Persson, D. The elderly driver: deciding when to
stop. Gerontologist. 1993;33(1):88–91.
21. Preusser, D. F., Williams, A. F., Ferguson, S. A.,
Ullmer R. G., & Weinstein, H.B. Fatal crash
risk for older drivers at intersections. Accid Anal
Prev. 30(2):151–159.
22. Williams, A. F., & Ferguson, S. A. Rationale
for graduated licensing and the risks it should
address. Inj Prev. 8:ii9–ii16.
23. Eberhard, J. W. Safe Mobility for Senior
Citizens. International Association for Trafc
and Safety Sciences Research. 20(1):29–37.

4 Chapter 1—Safety and the Older Driver With Functional or Medical Impairments: An Overview
hand turns are a particular problem for
the older driver. At stop-sign-controlled
intersections, older drivers may not know
when to turn.
24
These driving behaviors indicate that
visual, cognitive, and/or motor factors
may affect the ability to drive in older
adults. Research has not yet determined
what percentage of older adult crashes
are due to driving errors that are also
common among middle-aged drivers,
what proportion are due to age-related
changes in cognition (such as delayed
reaction time), or how many could be
attributed to age-related medical illness-
es. However, it is believed that further
improvements in trafc safety will likely
result from improving driving perfor-
mance or modifying driving behavior.
25
The identication and management
of diseases has a potential to maintain
or improve driving abilities and
road safety.
Fact #5: Physicians can inuence
their patients’ decisions to modify
or stop driving. They can also help
their patients maintain safe
driving skills.
Although older drivers believe that
they should be the ones to make the
nal decision about driving, they also
agree that their physicians should advise
them. In a series of focus groups con-
ducted with older adults who had given
up driving, all agreed that the physi-
cians should talk to older adults about
driving, if a need exists. As one panelist
put it, “When the doctor says you can’t
drive anymore, that’s denite. But when
you decide for yourself, there might be
questions.” While family advice had
limited inuence on the participants,
most agreed that if their physicians
advised them to stop and their family
concurred, they would certainly retire
from driving.
26
This is consistent with a
24. Preusser, D. F., Williams, A. F., Ferguson, S. A.,
Ullmer, R. G., & Weinstein, H. B. Fatal crash
risk for older drivers at intersections. Accid Anal
Prev. 30(2):151–159.
25. Lee, J. D. Fifty years of driving safety research.
Hum Factors. 50: 521–528.
26. Persson, D. The elderly driver: deciding when to
stop. Gerontologist. 1993;33(1):88–91.
recent focus group study with caregivers
of demented drivers, who stated that
physicians should be involved in this
important decision-making process.
27
Physicians assist their older patients
to maintain safe mobility in two ways.
They provide effective treatment and
preventive health care, and they play a
role in determining the ability of older
adults to drive safely. Also, improved
cardiovascular and bone health has
the potential to reduce serious injuries
and improve the rate of recovery in the
event of a crash.
In many cases, physicians can keep
their patients on the road longer by
identifying and managing diseases, such
as cataracts and arthritis, or by discon-
tinuing sedating medications. Many
physicians are aware of the literature on
fall prevention, and that clinicians can
reduce future risks of falls and fractures
by addressing certain extrinsic (envi-
ronmental) and intrinsic factors.
28
Driv-
ing abilities share many attributes that
are necessary for successful ambulation,
such as adequate visual, cognitive, and
motor function. In fact, a history of falls
has been associated with an increased
risk of motor vehicle crash.
29
Brief physician intervention on topics
such as smoking and seat belt use has
been shown to be effective. There is
an assumption that doctors can and do
make a difference by evaluating older
individuals for medical tness to drive.
Furthermore, there is a crucial need to
have this hypothesis studied systemati-
cally. To date, little organized effort in
the medical community has been made
to help older adults improve or main-
tain their driving skills. Research and
clinical reviews on the assessment
27. Perkinson, M., Berg-Weger, M., Carr, D.,
Meuser, T., Palmer, J., Buckles, V., Powlishta,
K., Foley, D., & Morris, J. Driving and dementia
of the Alzheimer type: beliefs and cessation
strategies among stakeholders. Gerontologist.
45(5):676–685.
28. Tinetti, M. E. Preventing falls in elderly persons.
N Engl J Med. 348(1):42–49.
29. Margolis, K. L., Kerani, R. P., McGovern, P.,
et al. Risk factors for motor vehicle crashes in
older women. J Gerontol Series A Bio Sci Med Sci.
57:M186–M191.
of older drivers have focused on screen-
ing methods to identify unsafe drivers
and restrict older drivers. Physicians are
in a position to identify patients at risk
for unsafe driving or self-imposed driv-
ing cessation due to functional impair-
ments, and address and help manage
these issues to keep their patients driv-
ing safely for as long as possible.
Physicians must abide by State report-
ing laws. While the nal determination
of an individual’s ability to drive lies
with the driver licensing authority,
physicians can assist with this deter-
mination. Driver licensing regulations
and reporting laws vary greatly by State.
Some State laws are vague and open to
interpretation; therefore, it is impor-
tant for physicians to be aware of their
responsibilities for reporting unsafe
patients to the local driver licensing
authority. Information on State laws is
provided in Chapter 8.
Thus, physicians can play a more active
role in preventing motor vehicle crashes
by assessing their patients for medical
tness to drive, recommending safe
driving practices, referring patients to
driver rehabilitation specialists, advising
or recommending driving restrictions,
and referring patients to State authori-
ties when appropriate.

5Chapter 1—Safety and the Older Driver With Functional or Medical Impairments: An Overview
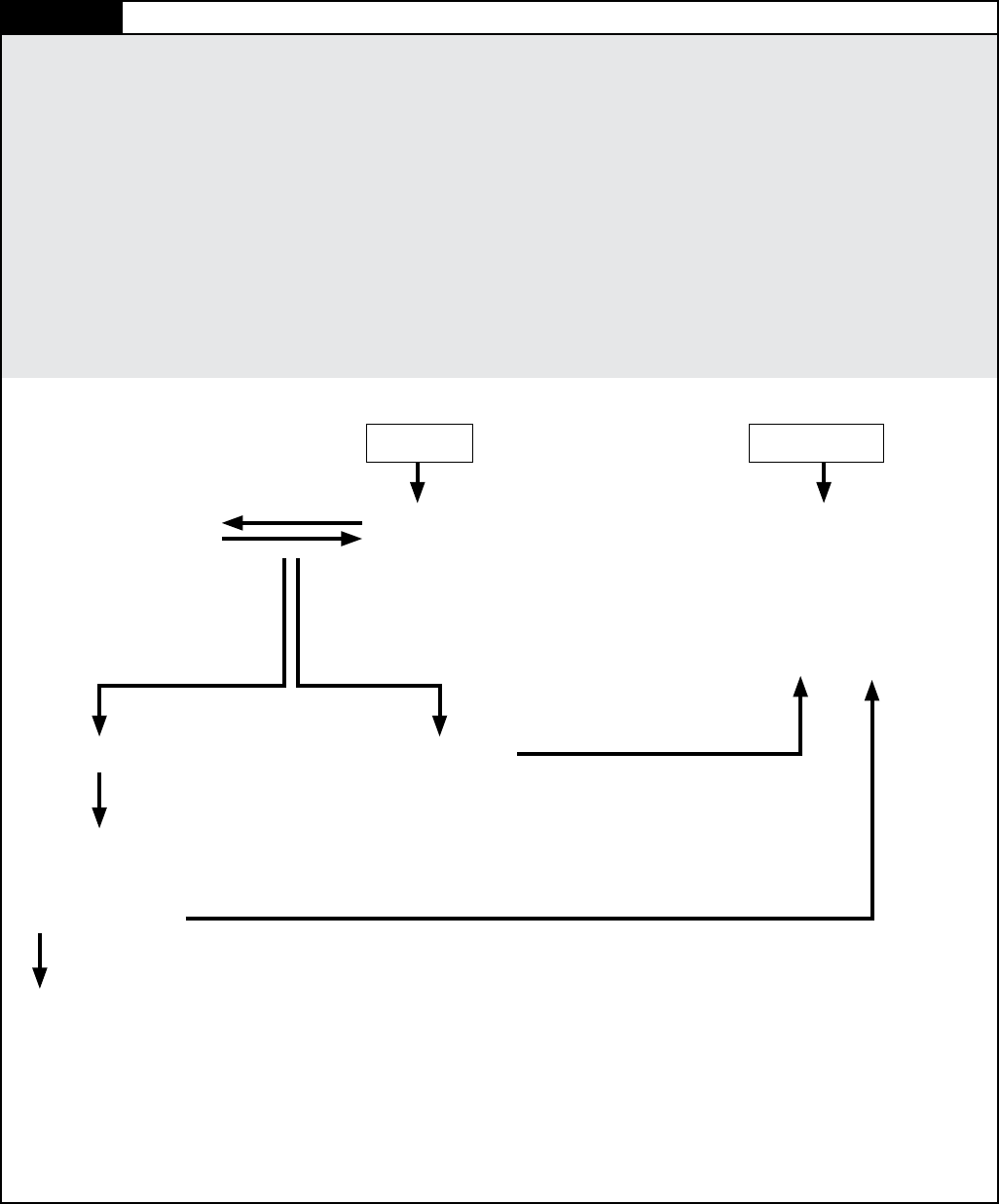
To achieve these ends, primary care
physicians can follow the algorithm,
Physician’s Plan for Older Drivers’ Safety
(PPODS) (see Figure 1.1), which
recommends that physicians:
• Screen for red ags such as medical
illnesses and medications that may
impair driving safety;
• Ask about new-onset impaired
driving behaviors (see Am I a Safe
Driver and How to Help the Older
Driver in the appendices);
• Assess driving-related functional
skills in those patients who are at
increased risk for unsafe driving; for
the functional assessment battery,
Assessment of Driver Related Skills
(ADReS), see Chapter 3;
• Treat any underlying causes of
functional decline;
• Refer patients who require a driving
evaluation and/or adaptive training to
a driver rehabilitation specialist;
• Counsel patients on safe driving
behavior, driving restrictions, driving
cessation, and/or alternate transporta-
tion options as needed; and
• Follow-up with patients who should
adjust their driving to determine if
they have made changes, and evalu-
ate those who stop driving for signs of
depression and social isolation.
While primary care physicians may
be in the best position to perform the
PPODS, other clinicians have a re-
sponsibility to discuss driving with their
patients as well. Ophthalmologists,
neurologists, psychiatrists, physiatrists,
orthopedic surgeons, emergency depart-
ment and trauma center physicians,
and other specialists all treat condi-
tions, prescribe medications, or perform
procedures that may have an impact on
driving skills. When counseling their
patients, physicians may wish to
consult the reference list of medical
conditions in Chapter 9.
In the following chapters, we will guide
you through the PPODS and provide
the tools you need to perform it. Before
we begin, you may wish to review the
AMA’s policy on impaired drivers (see
Figure 1.2).This policy can be applied
to older drivers with medical conditions
that impair their driving skills and
threaten their personal driving safety.
Fact #6: Trafc safety for older
drivers is a growing public
health issue.
Older drivers are the safest drivers as
an age group when using the absolute
number of crashes per 100 licensed
drivers per year.
30
However, the crash
rate per miles driven reveals an increase
at about age 65 to 70 in comparison to
middle-aged drivers.
31
In 2000, 37,409
Americans died in motor vehicle
crashes.
32
Of this number, 6,643 were 65
and older.
33
Accidental injuries are the
seventh leading cause of death among
older people and motor vehicle crashes
are not an uncommon cause.
34
As the
number of older drivers continues to
grow, drivers 65 and older are expected
to account for 16 percent of all crashes
and 25 percent of all fatal crashes.
35
Motor vehicle injuries are the leading
cause of injury-related deaths among
65- to 74-year-olds and are the second
leading cause (after falls) among 75- to
84-year-olds.
36
Compared to other driv-
30. CDC. (1997). Behavioral Risk Factor Surveil-
lance System Survey Data. Atlanta: Centers for
Disease Control and Prevention
31. Ball, K., Owsley, C., Stalvey, B., Roenker, D.
L., & Sloane, M. E. Driving avoidance and
functional impairment in older drivers. Accid
Anal Prev. 30:313–322.
32. NHTSA. FARS. Web-Based Encyclopedia.
www-fars.nhtsa.dot.gov.
33. Insurance Institute for Highway Safety. (2001).
Fatality Facts: Elderly (as of October 2001).
(Fatality Facts contains an analysis of data from
U.S. Department of Transportation Fatality
Analysis Reporting System.) Arlington, VA:
Insurance Institute for Highway Safety.
34. Staats, D. O. Preventing injury in older adults.
Geriatrics. 63:12–17.
35. Eberhard, J. Older drivers up close: they aren’t
dangerous. Insurance Institute for Highway Safety
Status Report (Special Issue: Older Drivers).
36(8):1–2.
36. CDC. (1999). 10 Leading Causes of Injury
Deaths, United States, 1999, All Races, Both
Sexes. Ofce of Statistics and Programming,
National Center for Injury Prevention and Con-
trol, Centers for Disease Control and Preven-
tion. Data source: National Center for Health
Statistics Vital Statistics System. Atlanta:
Centers for Disease Control and Prevention.
ers, older drivers have a higher fatality
rate per mile driven than any other age
group except drivers under 25.
37
On the
basis of estimated annual travel, the
fatality rate for drivers 85 and older is
9 times higher than the rate for drivers
25 to 69.
38
By age 80, male and female
drivers are 4 and 3.1 times more likely,
respectively, than 20-year-olds to die
as a result of a motor vehicle crash.
39
There is a disproportionately higher rate
of poor outcomes in older drivers, due
in part to chest and head injuries.
40
Old-
er adult pedestrians are also more likely
to be fatally injured at crosswalks.
41
There may be several reasons for this
excess in fatalities. First, some older
drivers are considerably more fragile.
For example, the increased incidence
of osteoporosis, which can lead to
fractures, and/or atherosclerosis of the
aorta which can predispose individuals
to rupture with chest trauma from an
airbag or steering wheel. Fragility begins
to increase at age 60 to 64 and
increases steadily with advancing age.
42
A recent study noted that chronic
conditions are determinants of mortality
and even minor injury.
43
As noted above,
older drivers are also overrepresented in
37. NHTSA. Driver fatality rates, 1975-1999.
Washington, DC: National Highway Trafc
Safety Administration.
38. NHTSA. National Center for Statistics &
Analysis. Trafc Safety Facts 2000: Older
Population. DOT HS 809 328. Washington,
DC: National Highway Trafc Safety
Administration.
39. Evans, L. Risks older drivers face themselves
and threats they pose to other road users.
Int J Epidemiol. 29:315–322.
40. Bauza, G., Lamorte, W. W., Burke, P., &
Hirsch, E. F. High mortality in elderly drivers is
associated with distinct injury patterns: analysis
of 187,869 drivers. J Trauma Inj Infect Crit Care.
64:304–310.
41. FHWA. (2007). Pedestrian Safety Guide and
Countermeasres. PEDSAFE. 2007. Washington,
DC: Federal Highway Administration. www.
walkinginfo.org/pedsafe/crashstats.cfm. Accessed
November 21, 2007.
42. Li, G., Braver, E., & Chen, L-H. Fragility versus
excessive crash involvement as determinants of
high death rates per vehicle mile of travel for
older drivers. Accid Anal Prev. 35, 227–235.
43. Camiloni, L., Farchi, S., Giorgi Rossi, P., Chini,
F., et al. Mortality in elderly injured patients:
the role of comorbidities. Int J Inj Control Safety
Prom. 15:25–31.
(Continues on page 7)
6 Chapter 1—Safety and the Older Driver With Functional or Medical Impairments: An Overview
Figure 1.1 Physician’s Plan for Older Drivers’ Safety (PPODS)
Is the patient at increased risk for unsafe driving?
Perform initial screen—
• Observe the patient
• Be alert to red ags
¤ Medical conditions
¤ Medications and polypharmacy
¤ Review of systems
¤ Patient’s or family member’s concern/
impaired driving behaviors
At risk
Formally assess function
• Assess Driving Related Skills (ADReS)
¤ Vision
¤ Cognition
¤ Motor and somatosensory skills
Medical interventions
• For diagnosis and
treatment
Counsel and follow up
• Explore alternatives to driving
• Monitor for depression and social isolation
• Adhere to state reporting regulations
Deficit not resolved
Refer to Driver Rehabilitation Specialist:
Is the patient safe to drive?
No Yes
Deficit resolved
Not at risk
Health maintenance
• Successful Aging Tips
• Tips for Safe Driving
• Mature Driving classes
• Periodic follow-up
If screen is positive—
• Ask health risk assessment/social history questions
• Discuss alternatives to driving early in the process
• Gather additional information

7
left-hand-turn collisions, which cause
more injury than more injury than
rear-end collisions.
44
Finally, preliminary
data from a Missouri study of medically
impaired drivers who were in crashes
indicate that the average age of the
vehicle was more than 10 years and the
cars often did not have air bags (personal
communication, Tom Meuser, University
of St. Louis-Missouri). If this latter obser-
vation is a contributing factor, improve-
ment should occur as future cohorts of
aging drivers purchase newer vehicles
with improved crashworthiness.
44. IIHS. (2003). Fatality Facts: Older People as
of November 2002. Arlington, Va: Insurance
Institute for Highway Safety.
Chapter 1—Safety and the Older Driver With Functional or Medical Impairments: An Overview
Figure 1.2
AMA ethical opinion
E-2.24 Impaired drivers and their physicians
The purpose of this policy is to articulate physicians’ responsibility to recognize
impairments in patients’ driving ability that pose a strong threat to public safety and
which ultimately may need to be reported to the Department of Motor Vehicles. It
does not address the reporting of medical information for the purpose of punish-
ment or criminal prosecution.
1. Physicians should assess patients’ physical or mental impairments that might
adversely affect driving abilities. Each case must be evaluated individually since
not all impairments may give rise to an obligation on the part of the physician.
Nor may all physicians be in a position to evaluate the extent or the effect of an
impairment (e.g., physicians who treat patients on a short-term basis). In mak-
ing evaluations, physicians should consider the following factors: (a) the physi-
cian must be able to identify and document physical or mental impairments
that clearly relate to the ability to drive; and (b) the driver must pose a clear risk
to public safety.
2. Before reporting, there are a number of initial steps physicians should take.
A tactful but candid discussion with the patient and family about the risks of
driving is of primary importance. Depending on the patient’s medical condition,
the physician may suggest to the patient that he or she seek further treatment,
such as substance abuse treatment or occupational therapy. Physicians also
may encourage the patient and the family to decide on a restricted driving
schedule, such as shorter and fewer trips, driving during non-rush-hour traffic,
daytime driving, and/or driving on slower roadways if these mechanisms would
alleviate the danger posed. Efforts made by physicians to inform patients and
their families, advise them of their options, and negotiate a workable plan may
render reporting unnecessary.
3. Physicians should use their best judgment when determining when to report
impairments that could limit a patient’s ability to drive safely. In situations where
clear evidence of substantial driving impairment implies a strong threat to
patient and public safety, and where the physician’s advice to discontinue driv-
ing privileges is ignored, it is desirable and ethical to notify the Department of
Motor Vehicles.
4. The physician’s role is to report medical conditions that would impair safe driv-
ing as dictated by his or her State’s mandatory reporting laws and standards of
medical practice. The determination of the inability to
drive safely should be made by the State’s Department of Motor Vehicles.
5. Physicians should disclose and explain to their patients this responsibility to
report.
6. Physicians should protect patient confidentiality by ensuring that only the mini-
mal amount of information
is reported and that reasonable security measures are used in handling that
information.
7. Physicians should work with their State medical societies to create statutes
that uphold the best interests of patients and community, and that safeguard
physicians from liability when reporting in good faith. (III, IV, VII) Issued June
2000 based on the report “Impaired Drivers and Their Physicians,” adopted
December 1999.

CHAPTER 2
Is the Patient at
Increased Risk for
Unsafe Driving?

11Chapter 2—Is the Patient at Increased Risk for Unsafe Driving?
Mr. Phillips, a 72-year-old man with
a history of hypertension, congestive
heart failure, type 2 diabetes mel-
litus, macular degeneration, and
osteoarthritis comes to your ofce for
a routine check-up. You notice that
Mr. Phillips has a great deal of trou-
ble walking to the examination room,
is aided by a cane, and has difculty
reading the labels on his medication
bottles, even with his glasses. While
taking a social history, you ask him
if he still drives, and he states that
he takes short trips to run errands,
reach appointments, and meet
weekly with his bridge club.
Mr. Bales, a 60-year-old man with
no signicant past medical history,
presents at the emergency department
with an acute onset of substernal
chest pain. He is diagnosed with
acute myocardial infarction. Follow-
ing an uneventful hospital course, he
is stable and ready to be discharged.
On the day of discharge, he mentions
that he had driven himself to the
emergency department and would
now like to drive himself home, but
cannot nd his parking voucher.
CHAPTER 2
Is the Patient at Increased
Risk for Unsafe Driving?
This chapter discusses the rst steps of
the Physician’s Plan for Older Drivers’
Safety (PPODS). In particular, we
provide a strategy for answering the
question, “Is the patient at increased
risk for unsafe driving?” This part of the
evaluation process includes your clinical
observation, identifying red ags such
medical illnesses and medications that
may impair safe driving, and inquiring
about new onset driving behaviors that
may indicate declining trafc skills.
To answer this question, rst—
Observe the patient
throughout the office visit.
Careful observation is often an impor-
tant step in diagnosis. As you observe
the patient, be alert to:
• Impaired personal care such as poor
hygiene and grooming;
• Impaired ambulation such as difculty
walking or getting into and out of
chairs
• Difculty with visual tasks; and
• Impaired attention, memory, language
expression or comprehension.
In the example above, Mr. Phillips
has difculty walking and reading his
medication labels. This raises a question
as to whether he can operate vehicle
foot pedals properly or see well enough
to drive safely. His physical limitations
would not preclude driving, but may
be indicators that more assessment
is indicated.
Be alert to conditions in the
patient’s medical history,
examine the current list of
medications, and perform
a comprehensive review
of systems.
When you take the patient’s history, be
alert to “red ags,”
45
that is, any medical
condition, medication or symptom that
can affect driving skills, either through
acute effects or chronic functional
decits (see Chapter 9). For example,
Mr. Evans, as described in Chapter 1,
presents with lightheadedness associated
with atrial brillation. This is a red ag,
and he should be counseled to cease
driving until control of heart rate and
symptoms that impair his level of con-
sciousness have resolved. Similarly, Mr.
Bales’ acute myocardial infarction is a
red ag. Prior to discharge from the
hospital, his physician should counsel
him about driving according to the
recommendations in Chapter 9 (see
Figure 2.1).
Mr. Phillips does not have any acute
complaints, but his medical history
identies several conditions that place
him at potential risk for unsafe driving.
His macular degeneration may prevent
him from seeing well enough to drive
safely. His osteoarthritis may make it
difcult to operate vehicle controls or it
may restrict his neck range of motion,
thereby diminishing visual scanning
in trafc. Questions in regard to his
45. Dobbs, B. M. (2005) Medical Conditions and
Driving: A Review of the Literature (1960-
2000). Report # DOT HS 809 690. Wahington,
DC: National Highway Trafc Safety Adminis-
tration. Accessed October 11, 2007.
at www.nhtsa.dot.gov/people/injury/research/
Medical_Condition_Driving/pages/TRD.html.
12 Chapter 2—Is the Patient at Increased Risk for Unsafe Driving?
diabetes include: Does he have any
end-organ damage such as sensory neu-
ropathies, chronic cognitive decline, or
uctuations from stroke that may affect
his ability to operate a motor vehicle?
Could any of his medications impair
driving performance?
Most older adults have at least one
chronic medical condition and many
have multiple conditions. The most
common medical conditions in older
adults include arthritis, hypertension,
hearing impairments, heart disease,
cataracts, dizziness, orthopedic impair-
ments, and diabetes.
46
Some of these
conditions have been associated with
driving impairment and will be dis-
cussed in more detail in subsequent
chapters. Additionally, keep in mind
that many prescription and nonpre-
scription medications have the po-
tential to impair driving skills, either
by themselves or in combination with
other drugs. (See Chapter 9 for a more
in-depth discussion on medications and
driving.) Older patients generally take
more medications than their younger
counterparts and are more susceptible
to their central nervous system effects.
Whenever you prescribe one of these
medications or change its dosage, coun-
sel your patient on its potential to affect
driving safety. You may also recommend
that your patient undergo formal
assessment of function (see Chapter 3)
while he/she is taking a new medication
that may cause sedation. Concern may
be heightened if there are documented
difculties in attention or visuospatial
processing speed (e.g., such as the Trails
B test [see Chapters 3 and 4]).
The review of systems can reveal
symptoms that may interfere with the
patient’s driving ability. For example,
loss of consciousness, confusion, falling
sleep while driving, feelings of faintness,
memory loss, visual impairment, and
muscle weakness all have the potential
to endanger the driver.
46. Health United States: 2002; Current Population
Reports, American with Disabilities, p. 70–73.
Figure 2.1
Counseling the driver in the
inpatient setting
When caring for patients in the inpatient
setting, it can be all too easy for physi-
cians to forget about driving. In a survey
of 290 stroke survivors who were inter-
viewed 3 months to 6 years post-stroke,
fewer than 35% reported receiving advice
about driving from their physicians, and
only 13% reported receiving any type of
driving evaluation. While it is possible that
many of these patients suffered such ex-
tensive deficits that both the patient and
physician assumed that it was unlikely for
the patient to drive again, patients should
still receive driving recommendations from
their physician.
Counseling for inpatients may include
recommendations for permanent driving
cessation, temporary driving cessation,
or driving assessment and rehabilita-
tion when the patient’s condition has
stabilized. Such recommendations are
intended to promote the patient’s safety
and, if possible, help the patient regain
his/her driving abilities.
Figure 2.2
Health risk assessment
A health risk assessment is a series of
questions intended to identify potential
health and safety hazards in the patient’s
behaviors, lifestyle, and living environment.
A health risk assessment may include
questions about, but not limited to:
• Physical activity and diet;
• Use of seat belts;
• Presence of smoke detectors and fire
extinguishers in the home;
• Presence of firearms in the home; and
• Episodes of physical or emotional
abuse.
The health risk assessment is tailored to
the individual patient or patient population.
For example, a pediatrician may ask the
patient’s parents about car seats, while a
physician who practices in a warm-climate
area may ask about the use of hats and
sunscreen. Similarly, a physician who sees
older patients may choose to ask about
falls, injuries, and driving.
At times, patients themselves or family
members may raise concerns. If the fam-
ily of your patient asks, “Is he or she safe
to drive?” (or if the patient expresses
concern), identify the reason for the
concern. Has the patient had any recent
crashes or near-crashes, or is he/she los-
ing condence due to declining
functional abilities? Inquiring about
specic driving behaviors may be more
useful than asking global questions
about safety. A list of specic driving
behaviors that could indicate concerns
for safety is listed in the Hartford guide,
“At the Crossroads.”
47
Physicians can
request family members or spouses to
monitor and observe skills in trafc
with full disclosure and permission from
the patient. Another tactic might be
identifying a family member who refuses
to allow other family members such
as the grandchildren to ride with the
patient due to trafc safety concerns.
Please note that age alone is not a red
ag! Unfortunately, the media often
emphasize age when an older driver is
involved in an injurious crash. This
“ageism” is a well-known phenomenon
in our society.
48
While many people
experience a decline in vision, cognition,
or motor skills as they get older, people
age at different rates and experience
functional changes to different degrees.
The focus should be on functional abili-
ties and medical tness-to-drive and
not on age per se.
Inquire about driving during
the social history/health risk
assessment.
If a patient’s presentation and/or the
presence of red ags lead you to suspect
that he/she is potentially at risk for
unsafe driving, the next step is to ask
whether he/she drives. You can do this
by incorporating the following ques-
tions into the social history or health
risk assessment (see Figure 2.2):
47. The Hartford. At the Crossroads. Hartford, CT.
www.thehartford.com/alzheimers/brochure.html.
Accessed December 12, 2007.
48. Nelson, T. (2002). Ageism: Stereotyping and
Prejudice Against Older Persons. Cambridge,
MA: MIT Press.

13Chapter 2—Is the Patient at Increased Risk for Unsafe Driving?
• “How did you get here today?” or
“Do you drive?”; and
• “Are you having any problems while
operating a motor vehicle?”;
• “Have others expressed concern
about your driving?”; and
• “What would you do if you had to
stop driving?”
If your patient drives, then his/her driv-
ing safety should be addressed. For acute
illness, this generally involves counsel-
ing the patient. For example, Mr. Bales
should be counseled to temporarily
cease driving for a certain period of
time after his acute myocardial infarc-
tion (see Chapter 9). If Mr. Phillips is
started on a new medication, he should
be counseled about the side effects and
their potential to impair driving perfor-
mance, if appropriate.
For chronic conditions, on the other
hand, driving safety is addressed by
formally assessing the functions that are
important for driving. This assessment
will be discussed further in the
next chapter.
Please note that some chronic medical
conditions may have both chronic and
acute effects. For example, a patient
with insulin-dependent diabetes may
experience acute episodes of hypogly-
cemia, in addition to having chronic
complications such as diabetic retinopa-
thy and/or peripheral neuropathy.
In this case, the physician should
counsel the patient to avoid driving
until acute episodes of hypoglycemia
are under control and to keep candy
or glucose tablets within reach in the
car at all times. The physician should
also recommend formal assessment of
function if the patient shows any signs
of chronic functional decline. (See
Chapter 9 for the full recommendation
on diabetes and driving.)
If your patient does not drive, you may
wish to ask if he/she ever drove, and if
so, what the reason was for stopping. If
your patient voluntarily stopped driving
due to medical reasons that are poten-
tially treatable, you may be able to
help her or him return to safe driving.
In this case, formal assessment of
function can be performed to identify
specic areas of concern and serve as
a baseline to monitor the patient’s
improvement with treatment. Referral
to a driver rehabilitation specialist in
these cases is strongly encouraged (see
Chapter 5).
Gather additional information.
To gain a better sense of your patient as
a driver, ask questions specic to driving.
The answers can help you determine the
level of intervention needed.
If a collateral source such as a family
member is available at the appointment
or bedside, consider addressing your
questions to both the patient and the
collateral source with the patient’s
permission. If this individual has had
the opportunity to observe the patient’s
driving, his/her feedback may be
valuable.
Questions to ask the patient and/or
family member:
• “How much do you drive?” (or
“How much does [patient] drive?”)
• “Do you have any problems when you
drive?” (Ask specically about day
and night vision, ease of operating
the steering wheel and foot pedals,
confusion, and delayed reaction to
trafc signs and situations.)
• “Do you think you are a safe driver?”
• “Do you ever get lost while driving?”
• “Have you received any trafc viola-
tions or warnings in the past two years?”
• “Have you had any near-crashes or
crashes in the past two years?”
Understand your patient’s
mobility needs.
At this time you can also ask about your
patient’s mobility needs and encourage
him/her to begin exploring alternative
transportation options before it be-
comes imperative to stop driving. Even
if alternative transportation options
are not needed at this point, it is wise
for the patient to plan ahead in case it
ever becomes necessary.
Some questions you can use to initiate
this conversation include:
• “How do you usually get around?”
• “If your car ever broke down, how
would you get around? Is there any-
one who can give you a ride? Can you
use a public train or bus? Does your
community offer a shuttle service or
volunteer driver service?”
Encourage your patients to plan a safety
net of transportation options. You might
want to say, “Mobility is very impor-
tant for your physical and emotional
health. If you were ever unable to drive
for any reason, I’d want to be certain
that you could still make it to your ap-
pointments, pick up your medications,
go grocery shopping, and visit your
friends.”
Sources for educational materials are
listed in Appendix B like the Hart-
ford insurance company’s “We need to
talk,” AARP materials, or University
of Michigan Transportation Research
Institute’s materials
49
, which could be
invaluable in planning for maintaining
out-of-home activities.
50
In the event
that your patient must cease driving,
the transition from driver to non-driver
status will be less traumatic if he/she has
already created a transportation plan.
In addition the handout in Appendix B,
Getting By Without Driving, can help
your patient get started.
49. University of Michigan Transportation
Research Institute. UMTRI Library; 2007.
www.umtri.umich.edu/pubsdata.php.
Accessed November 21, 2007.
50. The Hartford. Family Conversations With
Older Drivers. Hartford, CT. www.thehartford.
com/talkwitholderdrivers/. Accessed October 11,
2007.
14 Chapter 2—Is the Patient at Increased Risk for Unsafe Driving?
Red Flags for Further Assessment
Acute events
Prior to hospital or emergency department discharge, patients
and appropriate caregivers should be counseled as needed
regarding temporary driving cessation:
• Acute myocardial infarction;
• Acute stroke and other traumatic brain injury;
• Arrhythmia;
• Lightheadedness and pre-syncope;
• Syncope and vertigo;
• Seizure;
• Surgery;
• Delirium from any cause; and
• New sedating medications.
Patient’s or family member’s concern
Has your patient approached you with the question, “Am I
safe to drive?” (Alternatively, a family member may express
concern about the patient’s driving safety.) If so, nd out
the cause of concern. Note that age alone does not predict
driving tness—function, not age, is the determining factor.
Ask for specic causes of concern, such as recent crashes,
near-misses, trafc tickets, becoming lost, poor night vision,
forgetfulness, and confusion. Evaluate for function using the
Assessment of Driver Related Skills (ADReS) battery (Chap-
ters 3 and 4).
Medical history: Chronic medical conditions
Patients may require formal assessment to determine the
impact of these conditions on their level of function:
• Diseases affecting vision, including cataracts, diabetic retin-
opathy, macular degeneration, glaucoma, retinitis pigmen-
tosa, eld cuts, and low visual acuity even after correction;
• Cardiovascular disease, especially when associated with pre-
syncope, syncope or cognitive decits, including unstable
coronary syndrome, arrhythmias, palpitations, congestive
heart failure, hypertrophic obstructive cardiomyopathy, and
valvular disease;
• Neurologic disease, including dementia, multiple sclerosis,
Parkinson’s disease, peripheral neuropathy, brain injury,
spinal cord injury, and residual decits from stroke;
• Psychiatric disease, including mood disorders, depression,
anxiety disorders, psychotic illness, personality disorders,
and alcohol or other substance abuse;
• Metabolic disease, including type 1 and type 2 diabetes mel-
litus especially with hypoglycemic attacks or severe swings
in blood sugars, and hypothyroidism;
• Musculoskeletal disabilities, including arthritis and foot
abnormalities;
• Chronic renal failure;
• Respiratory disease, including chronic obstructive pulmonary
disease and obstructive sleep apnea; and
• Cancer and chemotherapy.
15Chapter 2—Is the Patient at Increased Risk for Unsafe Driving?
Medical history: Medical conditions with
unpredictable/episodic events
The patient should be counseled not to drive during any of
the following acute events until they have discussed this issue
with their physician:
• Pre-syncope or syncope;
• Angina;
• Seizure;
• Transient ischemic attacks;
• Hypoglycemic attacks;
• Vertigo;
• Alcoholism and hospitalization for detoxication; or
• Sleep attacks or cataplexy.
Medications
Many nonprescription and prescription medications have the
potential to impair driving ability, either by themselves or
in combination with other drugs. Combinations of drugs may
affect drug metabolism and excretion, and dosages may need
to be adjusted accordingly. (See Chapter 9 for a discussion of
each medication class.) Medications with strong potential to
affect the patient’s driving ability include:
• Anticholinergics;
• Anticonvulsants;
• Antidepressants;
• Antiemetics;
• Antihistamines;
• Antihypertensives;
• Antiparkinsonians;
• Antipsychotics;
• Benzodiazepenes and other sedatives/anxiolytics;
• Muscle relaxants;
• Narcotic analgesics; and
• Stimulants.
Review of systems
The review of systems can reveal symptoms or conditions
that may impair driving performance. In addition to further
work-up, driving safety should be addressed.
• General: fatigue, weakness;
• Head Ears Eyes Nose Throat (HEENT): headache, head
trauma, double vision, visual changes, vertigo;
• Respiratory: shortness of breath, use of oxygen;
• Cardiac: chest pain, dyspnea on exertion, palpitations,
sudden loss of consciousness;
• Musculoskeletal: muscle weakness, muscle pain, joint
stiffness or pain, decreased range of motion;
• Neurologic: loss of consciousness, feelings of faintness,
seizures, weakness/paralysis, tremors, loss of sensation,
numbness, tingling; and
• Psychiatric: depression, anxiety, memory loss, confusion,
psychosis, mania.
Assessment and plan
As you formulate a diagnosis/treatment plan for your patient’s
medical conditions, remember to address driving safety as
needed. You may need to counsel your patients about driving
when you:
• Prescribe a new medication, or change the dosage of a
current medication; and
• Work up a new-onset disease presentation or treat an
unstable medical condition. This includes many of the
medical conditions listed above.
Dobbs, B. M. (2005) Medical Conditions and Driving: A
Review of the Literature (1960-2000). Report # DOT HS
809 690. Washington, DC: National Highway Trafc Safety
Administration. www.nhtsa.dot.gov/people/injury/research/
Medical_Condition_Driving/pages/TRD.html.
Charlton, J., Koppel, S., O’Hare, M., Andrea, D., Smith, G.,
Khodr, B., Langford, J., Odell, M., & Fildes, B. (2004) Inu-
ence of chronic illness on crash involvement of motor vehicle
drivers, Monash University Accident Research Centre, Re-
port No. 213. www.monash.edu/muarc/reports/muarc213.html
For recent reviews please consult the following two extensive reviews on these topics, both available on-line:

CHAPTER 3
Assessing Functional
Ability

19
license,” you may nd it helpful to offer
reassurance that physicians do not have
that type of legal authority. Explain that
you may advise evaluation of driving if
needed and/or refer him/her to a driver
rehabilitation specialist or the Depart-
ment of Motor Vehicles (DMV).
Here is an example of how you could
suggest an evaluation to Mr. Phillips:
“Mr. Phillips, I’m concerned about your
safety when you drive. Your son tells me
that you were in a car crash recently and
that you’ve had several near crashes in the
past two years. Even though your medical
conditions are well managed, they can still
cause problems that can affect your driving
ability. I’d like you to do a few things for
me, such as walking down the hall while I
time you. These tests will help me decide
if there are areas we need to work on to
improve your driving safety.
“This is how it works: Based on what I
know about your health and how you do on
these tasks, we’ll do our best to identify any
potential treatable or reversible conditions.
For example, if you’re not seeing as well
as you should, then we’ll do what we can
to improve your vision. If there’s something
we can’t improve, then we can consult a
driver rehabilitation specialist. This type
of instructor, typically an occupational
therapist, will go out on the road with you
to watch you drive, then recommend ways
to make your driving safer. The goal is to
keep you on the road for as long as you are
safe to drive.”
As revealed in the PPODS algorithm
(Figure 1.1), the next step to managing
Mr. Phillips’ driving safety is a formal
assessment of the key functional abilities
related to driving. Specic information
in Mr. Phillips’ driving history—namely,
the crash, moving violations, or near
crashes—in addition to his medical
conditions, further support the need for
an assessment.
In this chapter, we discuss the functions
related to driving and present a brief
ofce test battery, the Assessment of
Driving Related Skills (ADReS). Each
test in ADReS assesses a key area of
function. Although not all functional
domains that are necessary or relevant
to driving are tested by the ADReS
battery, many key areas are and have
been validated with driving outcomes.
How do you broach the issue
of a driving assessment to
your patient?
Your patient may feel defensive about
being assessed and may even refuse
assessment for fear of being told that
he/she can no longer drive. After all,
driving is not only the primary form
of transportation for most Americans,
it also represents freedom and
independence.
In suggesting assessment to your patient,
it is best to use a direct but nonconfron-
tational approach. Reassure your patient
that you have his/her safety in mind
and emphasize that you would like to
assist him/her to drive safely for as long
as possible. If your patient expresses
fear that you will “take away my driver’s
Mr. Phillips, whom you met in
Chapter 2, has been accompanied
to the clinic by his son, who is in
the examination room with him.
Mr. Phillips tells you that he is a
safe driver. You request and obtain
permission to interview the son who
voices his concern. Four months ago,
Mr. Phillips was involved in a minor
car crash, in which he was found to
be at fault. He has also had several
near-crashes in the past two years.
However, he has never gotten lost
while driving.
In discussing Mr. Phillips’ trans-
portation options, you learn that he
drove himself to this appointment.
Driving is Mr. Phillips’ main mode
of transportation, and he drives
almost every day. Although Mr.
Phillips is certain—and his son
conrms—that family members and
neighbors would be willing to drive
him wherever he needs to go, he has
never asked for rides. “Why should
I ask for rides when I can just drive
myself around? Besides, I don’t want
to impose on my family or friends.”
CHAPTER 3
Assessing Functional
Ability

20 Chapter 3—Assessing Functional Ability
• Follow-up at the patient’s next ap-
pointment: Would he/she be willing
to complete the self-screening? Has
the patient put any of the tips into
practice? Does the patient have any
questions or concerns? Would he/she
be willing to undergo ADReS?
• If family members are concerned
about the patient’s driving safety,
you can give them a copy of How
to Assist the Older Driver, found in
Appendix B. Especially if the patient
has dementia, he/she will probably
lack insight and it will likely not
be fruitful to belabor the point. It is
important here to enlist family mem-
bers and obtain their aid in creating
a transportation plan for the patient
and encouraging the patient to be
evaluated by ADReS.
• If you are urgently concerned about
your patient’s driving safety, you may
wish to forego ADReS and refer your
patient directly to a driver rehabilita-
tion specialist (see Chapter 5) or to
your state DMV for a focused driving
assessment. Depending on your
State’s reporting laws, you may be
legally responsible for reporting
“unsafe” drivers to the DMV. (A
detailed discussion of the physician’s
legal responsibilities can be found in
Chapter 7. A reference list of report-
ing laws is provided in Chapter 8.)
In any case, the patient should be
referred with his/her knowledge.
At this point, the patient and/or
family might relent and be willing
to consider an evaluation from a
driving rehabilitation specialist.
Assessment of Driving-Related
Skills (ADReS)
The three key functions for safe driving
are (1) vision, (2) cognition, and (3)
motor/somatosensory function. ADReS
assesses some aspects of these three
important functions to help you identify
specic areas of concern.
Please note that ADReS does not pre-
dict crash risk! While many researchers
are working to create an easy-to-use
test battery that predicts crash risk,
further research is needed. However,
• Suggest that the patient take the
SAFER Driving survey. Also devel-
oped at the University of Michigan
Transportation Research Institute,
this is a Web-based tool (available at
um-saferdriving.org) that requires users
to answer questions about the severity
of health concerns they are expe-
riencing due to medical conditions
and medications. The Web site then
calculates the effects of these health
concerns on critical driving skills and
gives users individualized feedback on
how their driving may be declining;
what to do to continue driving safely
given these declines; and, if appro-
priate, recommendations for more
in-depth assessment. Research has
shown that feedback from the Web
site correlates positively with on-road
driving scores and an assessment from
an occupational therapist. Users also
report that the site is easy to use, the
information is helpful, and that they
discovered declines in themselves
of which they were not previously
aware.
54
• In the patient’s chart, document your
concern regarding his/her driving
ability, and support this with relevant
information from the patient’s presen-
tation, medical history, medications,
and reported driving history. Docu-
ment the patient’s refusal for further
assessment, along with any counseling
you have provided. (Current Proce-
dural Terminology [CPT
®
] codes for
counseling can be found in Appendix
A.) Not only will this remind you
to follow-up at the next visit, but
it could potentially protect you in
the event of a lawsuit. (A detailed
medicolegal discussion can be found
in Chapter 7.) In cases where the risk
is very high and the patient drives
despite your recommendations, you
might consider referral of the patient
to the DMV for further testing.
54. Eby, D. W., Molnar, L. J., Shope, J.T., & Del-
linger, A.M. Development and pilot testing of
an assessment battery for older drivers. J Safety
Res 38: 535-43.
What do you do if your patient
refuses assessment?
Despite your best efforts, your patient
may refuse to have his/her functional
abilities that are key to driving assessed.
If this occurs, you have several options:
• Encourage your patient to complete
the self-screening tool (Am I a Safe
Driver?) found in Appendix B. This
may help raise your patient’s level of
awareness and make him/her more
open to ADReS.
• Counsel your patient on the Success-
ful Aging Tips and Tips for Safe
Driving, both found in Appendix B.
These may raise your patient’s level
of awareness and encourage safe
driving habits.
• Suggest enrolling in a driving course
designed to improve trafc safety,
such as the Trafc Safety Course
offered by AARP
51
or those offered
by the AAA.
52
Roadwise Review is
a CD available from the AAA that
assesses important functional abili-
ties for driving and provides feedback
to older adults on the presence of
impairment.
53
Roadwise Review does
require the older adult to have a
computer and an assistant during the
playing of the CD. Give the patient a
copy of the Driving Decisions Work-
book. Developed by the University
of Michigan Transportation Research
Institute, this is a paper-and-pencil
workbook that provides users with
individualized feedback based on how
they answer questions. Research has
shown that workbook scores are posi-
tively correlated with on-road driving
scores and several clinical tests of
functional ability. The workbook can
be downloaded free of charge at:
http://deepblue.lib.umich.edu/bitstream/
2027.42/1321/2/94135.0001.001.pdf.
51. AARP Trafc Safety Course. www.aarp.org/
families/driver_safety/driver_safety_online_course.
html. Accessed October 14, 2007.
52. AAA Foundation for Trafc Safety Senior
Driver Web site. www.seniordrivers.org/home/
index.cfm. Accessed October 14, 2007.
53. AAA Exchange. Checking Your Driving Abili-
ties. www.aaapublicaffairs.com/Main/Default.as
p?SectionID=&SubCategoryID=38&CategoryID
=3&ContentID=315&. Accessed October 14,
2007.
21Chapter 3—Assessing Functional Ability
ptosis, which is more common in the
older population. Drivers with loss of
peripheral vision (e.g., glaucoma) may
have trouble noticing trafc signs or
cars and pedestrians that are about to
cross their path. Although earlier stud-
ies examining the relationship between
visual eld loss and driving performance
were equivocal, more recent studies
have found signicant relationships.
57
In ADReS, visual elds are measured
through confrontation testing.
Aspects of vision that are important for
safe driving
58
but are not included in
ADReS are:
• Contrast sensitivity: Older adults
require about three times more con-
trast than young adults to distinguish
targets against their background. This
decit in contrast sensitivity is further
exacerbated by low light levels. Thus,
older drivers may have problems
distinguishing cars or pedestrians
against background scenery, and this
may be much worse at night or during
storms.
59
While contrast sensitivity
has been found to be a valid predictor
of crash risk among older drivers,
60
most vision care specialists are not
familiar with measures of contrast
sensitivity, nor is it routinely mea-
sured in eye examinations. Further
research must be performed to produce
standardized, validated cut-off points
for contrast sensitivity, and further
work must be done to introduce
this concept to professionals in
eye care centers.
57. Dobbs, B. M. (2001). Medical Conditions and
Driving: Current Knowledge. Association for
the Advancement of Automotive Medicine/
National Highway Trafc Safety Administra-
tion, p. 24 Project DTNH22-94-G-05297.
Washington, DC: National Highway Trafc
Safety Administration
58. Walgreens. https://webapp.walgreens.com/ceP-
harmacy/programsHTML/transportation-tech.pdf.
Accessed October 14, 2007.
59. Owsley, C., & Ball, K. Assessing visual
function in the older driver. Clin Geriatr Med.
1993;9(2):389–401.
60. Dobbs, B. M. Medical Conditions and Driving:
Current Knowledge. Association for the Ad-
vancement of Automotive Medicine/ National
Highway Trafc Safety Administration, Project
DTNH22-94-G-05297. Washington, DC:
National Highway Trafc Safety Administra-
tion. 2001: p. 15–16.
To perform ADReS, you will need a
Snellen chart, tape to mark distances
on the oor, a stopwatch, and a pencil.
There are two paper-and-pencil tests in
ADReS, one of which requires a pre-
printed form. This is included on pages
28–29 and may be photocopied.
Vision
Vision is the primary sense utilized in
driving in comparison to other modali-
ties like hearing and proprioception,
and it is responsible for the majority
of driving-related sensory input.
55
In most States, candidates are required
to undergo vision testing to obtain
a driver’s license. Several States (see
Chapter 8) also require vision testing
at the time of license renewal.
Aspects of vision that are important for
safe driving and can be readily assessed
by a physician include:
• Visual acuity, and
• Visual elds.
Numerous studies show that visual
acuity declines between early and late
adulthood, although no consensus exists
on the rate of decline or decade of
onset. Decline in acuity is related to
physiologic changes of the eye that
occur with age and the increased
incidence of diseases such as cataracts,
glaucoma, and macular degeneration.
56
While far visual acuity is crucial to
many driving-related tasks, declines
in near visual acuity may be associ-
ated with difculty seeing or reading
maps, or gauges and controls inside the
vehicle. In ADReS, far visual acuity is
measured with a Snellen chart.
Visual elds may decline as a result of
the natural aging process and medical
conditions such as glaucoma, retinitis
pigmentosa, and stroke. In addition,
upper visual elds may be obstructed by
55. Shinar, D., & Schieber, F. (1991). Visual
requirements for safety and mobility of older
drivers. Hum Factors. 33(5):507-519.
56. Carr, D. B. Assessing older drivers for
physical and cognitive impairment. Geriatrics.
1993;48(5):46-51.
until physicians are able to test their
patients directly for crash risk, they can
test them indirectly by assessing the func-
tions that are necessary for safe driving.
Any impairment in these functions has
the potential to increase the patient’s
risk for crash. Once they are identied,
the physician is in a good position to
determine if the patient requires referral
to a specic subspecialist (e.g., ophthal-
mologist). Although cut-off scores are
provided for these tests (see Chapter 4),
the ADReS battery is a tool for identify-
ing areas of concern that require addi-
tional evaluation. The physician should
use his/her clinical judgment regardless
of the scores by utilizing all available
information (driving history, medical
history, and functional assessment). In
addition, not all important functions
are tested on the ADReS battery; rather
specic items were chosen for their
applicability and feasibility in the ofce
setting, along with their correlates with
impaired driving outcomes.
The tests in ADReS were selected by a
consensus panel of driving safety experts
who worked with the AMA, and were
chosen from among the many available
functional tests based on their ease of
use, availability, amount of time required
for completion, and quality of informa-
tion provided by the patient’s test perfor-
mance. The individual tests in ADReS
have been validated as measures of their
particular function and in some cases
have been studied with relation to driv-
ing. Although we are still awaiting more
evidenced-based medical studies to link
these tests with crash risk, these screens
can detect new-onset visual, cognitive,
or motor problems that may be amenable
to an intervention.
The tests are presented below by
function, following a discussion of the
function and how it relates to driving.
An accompanying score sheet on pages
28–29 can be photocopied and placed
in the patient’s chart. On the score
sheet, the tests are presented in the
recommended order of execution. CPT
®
codes for components of ADReS are
provided in Appendix A, and the score
sheet can serve as documentation for
these codes.
22 Chapter 3—Assessing Functional Ability
• Accommodation and adaptation:
Accommodation is the change in
the shape of the lens that assists with
bringing objects into focus. This is
an important skill for reading the
instrument panel in a car or viewing
objects in the mirror. Adaptation is
the ability to perceive objects when
levels of illumination are changing, as
might occur during nighttime driving
or in parking garages. Older adults
require more time than young adults
to adjust to abrupt changes in light
or darkness. As a result, older drivers
often report difculties dealing with
the sudden onset of bright lights, such
as the headlights of an oncoming car.
Glare may also play a role in their
visual difculties.
61
• Angular movement, dynamic visual
acuity, and depth perception. Older
adults must be able to detect objects
in motion such as judging the speed
of cars coming across their path dur-
ing left hand turns. This ties in with
the concept of dynamic visual acuity,
which may also require the detection
of letters or images (such as reading
trafc signs) while in motion. Depth
perception is important for near ob-
jects, but apparently becomes less of
an issue at further distances. A more
pertinent task is the ability to detect
changes in visual image size, such
as judging the speed of approaching
vehicles.
• Color. Many reviews on visual
abilities that are necessary for driving
tend to downplay the importance of
color detection, based on the current
level of evidence. Trafc lights in the
United States typically have mixed
colors embedded in the lights to
compensate for the small percentage
of the population that is red-green
color blind. However, the ability
to recognize trafc signs, which are
given specic colors based on a spe-
cic regulatory area, is important. In
addition, vehicle color may enhance
or diminish detection under certain
trafc conditions (e.g., a white car in
snowy weather, or a grey car in rainy
or foggy conditions).
61. Owsley, C., & Ball, K. Assessing visual func-
tion in the older driver. Clin Geriatr Med.
1993;9(2):389–401.
Assessment of Driving-Related Skills (ADReS)
Snellen E chart
The Snellen chart is used to test far visual acuity. The standard chart measures
9” x 23” and is printed on a durable, tear-resistant latex sheet, with eyelets for
easy hanging. Letters are printed on one side, and tumbling “E” symbols are
printed on the reverse.
With the chart hanging on a wall, the patient is instructed to stand 20 feet away.
Wearing his/her usual glasses or contact lenses, the patient reads the smallest line
possible with both eyes open. The patient’s visual acuity is based on the lowest full
row that he/she successfully reads. For example, if the best the patient can see is
20/40, then his/her acuity is 20/40 OU (oculus uterque). This process is repeated
for each eye individually (right eye: OD or oculus dexter; left eye: OS or oculus
sinister).
This test is best performed in a hallway with good lighting. Tape can be used to
mark a distance of 20 feet.
If you prefer, far visual acuity can be measured using the chart of your choice, such
as the Snellen chart for a 10-foot distance or the Sloan low vision letter chart for 6
meters (20 feet).
1
Near visual acuity can also be tested with commercially available charts, and
should be considered whenever a patient complains of difficulty seeing or reading
maps, or gauges and controls within the vehicle. Although not part of the ADReS
battery, many clinicians will check near vision using a Rosenbaum pocket chart.
Some limitations have been noted in testing using the Snellen chart. These
include—but are not limited to—the different number of letters per line, differ-
ent spacing between lines, the specific use of letters, and the spacing between
letters.
2
A trend in the field of eye care has been to use a newer chart called the
ETDRS (Early Treatment Diabetic Retinopathy Study) that in some studies of eye
diseases appears to be more accurate.
3
The ETDRS chart improves on the Snellen
test by having a similar number of letters per line and standard spacing between
the letters. Although it has not yet become the standard, it is possible that eye
clinics will eventually migrate toward this eye chart. For physicians offices that are
interested, ETDRS eye charts can be obtained from several sources and the stimuli
presented in a variety of formats (e.g., wall chart, computer).
1. Staplin, L., Lococo, K. H., Stewart, J., & Decina, L. E. (1999, April). Safe Mobility for Older People
Notebook. NHTSA Report No. DOT HS 808 853. Washington, DC: National Highway Trafc Safety
Administration.
2. Vector Vision. ETDRS Acuity Testing. www.vectorvision.com/html/educationETDRSAcuity.html. Accessed
October 14, 2007.
3. Falkenstein, I. A., Cochran, D. E., Azen, S. P., et al. Comparison of visual acuity in macular
degeneration: patients measured with Snellen and early treatment diabetic retinopathy study charts.
Ophthalmology. 10:319–23.
23Chapter 3—Assessing Functional Ability
Cognition
Driving is a complex activity that
requires a variety of high-level cognitive
skills. Among the cognitive skills that
are useful for driving
62
are:
• Memory—short-term, long-term,
and working memory;
• Visual perception, visual processing,
visual search, and visuospatial skills;
• Selective and divided attention;
• Executive skills (sequencing, plan-
ning, judgment, decision making);
• Language; and
• Vigilance.
Both crystallized memory and working
memory are necessary for driving. Not
only must drivers remember how to
operate their vehicle and what signs and
signals mean, they must also remember
their current destination and how to
get there.
63
In addition, drivers must be
able to retain certain information while
simultaneously processing other infor-
mation—a skill called working memory.
Working memory (and the other cogni-
tive skills to which it contributes) tends
to decline with age, while crystallized
memory remains relatively intact across
the life span. It is unclear at present
whether age-related memory impair-
ments reect only preclinical forms of
age-related diseases or whether these
occur independent of disease processes.
64
Visual perception, visual processing,
and visuospatial skills are necessary for
the driver to organize visual stimuli into
recognizable forms and know where
they exist in space. Without these skills,
the driver would be unable to recognize
a stop sign and determine its distance
from the car. In general, visual process-
62. Walgreens. https://webapp.walgreens.com/
cePharmacy/programsHTML/transportation-tech.
pdf. Accessed October 14, 2007.
63. Colsher, P. L., & Wallace R. B. Geriatric assess-
ment and driver functioning. Clin Geriatr Med.
1993;9(2):365–375.
64. Goetz, C. G. (1999). Textbook of Clinical
Neurology, 1st ed. Philadelphia: W.B. Saunders
Company.
ADReS (continued)
Visual fields by confrontation testing
The examiner sits or stands three feet in front of the patient, at the patient’s eye
level. The patient is asked to close his/her right eye, while the examiner closes his/
her left eye. Each fixes on the other’s nose.
The examiner then holds up a hand in each visual field simultaneously with a ran-
dom number (usually one or two) of fingers in each of the four quadrants, and asks
the patient to state the total number of fingers. With the fingers held slightly closer
to the examiner, the patient has a wider field of view than the examiner. Provided
that the examiner’s visual fields are within normal limits, if the examiner can see
the fingers, then the patient should be able to see them unless he/she has a visual
field defect.
The process is repeated for the other eye (patient’s left eye and examiner’s right
eye closed). The examiner indicates any visual field defects by shading in the area
of defect on a visual field representation.
Trail-making test, part B
This test of general cognitive function also specifically assesses working memory,
visual processing, visuospatial skills, selective and divided attention, and psycho-
motor coordination. In addition, numerous studies have demonstrated an associa-
tion between poor performance on the Trail-Making Test, Part B, and poor driving
performance.
1
(See Chapter 4 for further discussion.)
Part B involves connecting, in alternating order, encircled numbers (1–13) and
encircled letters (A–L) randomly arranged on a page. This test is scored by overall
time (seconds) required to complete the connections accurately. The examiner
points out and corrects mistakes as they occur; the effect of mistakes, then, is to
increase the time required to complete the test. This test usually takes
3 to 4 minutes to administer.
The examiner administers the test to the patient, stating, “Now I will give you a
paper and pencil. On the paper are the numbers 1 through 13 and the letters A
through L, scattered across the page. Starting with 1, draw a line to A, then to 2,
then to B, and so on, alternating back and forth between numbers and letters until
you finish with the number 13. I’ll time how fast you can do this. Are you ready?
Go.” The examiner records time-to-complete.
2
Although not recommended in the previous version of the ADReS battery, many
neuropsychologists recommend giving the Trails A test (connecting just numbers)
prior to giving the Trails B test. The rationale is at least twofold: (1) Trails A provides
an appropriate warm-up to Trails B, and allows the older adult some practice on a
simpler concept; and (2) in many of the driving studies that validated Trails B, Trails
A was given first. For clinicians who prefer to conduct both tests, collaborating with
a psychologist who uses the Trails A test (stimuli) can assist with administration
and oversight in the office setting. However, the recent Maryland Pilot Older Driver
Study (MaryPODS) that found an association with Trails B performance and at-fault
crashes in a cohort of older adults utilized only the practice trial of Trails B prior to
the full test. We have now included the practice trial of Trails B in the current stimuli
of the ADReS battery.
1. Staplin, L., Gish, K. W., & Wagner, E. K. (2003). MaryPODS revisited: updated crash analysis and
implications for screening program implementation. J Safety Res. 34:389–397.
2. Staplin, L., Lococo, K. H., Stewart, J., & Decina, L. E. (1999, April). Safe Mobility for Older People
Notebook. NHTSA Report No. DOT HS 808 853. Washington, DC: National Highway Trafc Safety
Administration.
24 Chapter 3—Assessing Functional Ability
ing may slow
65
and complex visuospatial
skills may decline with age, while visual
perception remains stable.
66
During driving, many demands are
made on attention. In particular, drivers
must possess selective attention—the
ability to prioritize stimuli and focus
on only the most important—in order
to attend to urgent stimuli (such as
trafc signs) while not being distracted
by irrelevant ones (such as roadside
ads). In addition, drivers must possess
divided attention in order to focus on
the multiple stimuli required by most
driving tasks. Attentional functioning
may decline with age,
67
with divided
attention showing more pronounced
changes than selective attention.
68
The most widely studied instrument
for detection of impairment in divided
attention and selective attention that
has been correlated with crash risk in
older adult drivers has been the Useful
Field of View (UFOV).
69
This test is
available for purchase and information is
available on the Visual Awareness Web
site.
70
Cost, time, and ability to bill,
as well as limited studies in a primary
care setting, might be potential barriers
to utilization in a physician’s ofce.
Another computerized set of tests that
assesses key functional abilities for driv-
ing is the Driving Health
©
Inventory
65. Owsley, C., & Ball K. Assessing visual
function in the older driver. Clin Geriatr Med.
1993;9(2):389–401.
66. Beers, M. H., & Berkow, R. (eds). (2000). The
Merck Manual of Geriatrics. Section 4, Chapter
32: Aging and mental health. Whitehouse
Station, NJ: Merck & Co., Inc..
67. Hartley, A. A. (1992). Attention. In: Craik, F.
I. M., & Salthouse, T.A. (eds). The Handbook
of Aging and Cognition. Pp. 3–50. Hillsdale, NJ:
Erlbaum.
68. Madden, D. J., Turkington, T. G., Provenzale, J.
M., Hawk, T. C., Hoffman, J. M., Coleman, R.
E. (1997). Selective and divided visual atten-
tion: age-related changes in regional cerebral
blood ow measured by H215O PET. Hum Brain
Mapp. 5:389–409.
69. Ball, K., Roenker, D.L., Wadley, V.G., et al.
(2006). Can high-risk older drivers be identied
through performance-based measures in a
Department of Motor Vehicles setting? J Am
Geriatr Soc. 54:77–84.
70. Visual Awareness.com. http://visualawareness.
com/Pages/request.html. Accessed October 14,
2007.
ADReS (continued)
Clock drawing test
Depending on the method of administration and scoring, the clock drawing
test (CDT) may assess a patient’s long-term memory, short-term memory, visual
perception, visuospatial skills, selective attention, abstract thinking, and executive
skills. Preliminary research indicates an association between specific scoring
elements of the clock drawing test and poor driving performance.
1
(See Chapter 4 for a further discussion.)
In this form of the CDT, the examiner gives the patient a pencil and a blank sheet
of paper and says, “I would like you to draw a clock on this sheet of paper. Please
draw the face of the clock, put in all the numbers, and set the time to ten minutes
after eleven.” This is not a timed test, but the patient should be given a reasonable
amount of time to complete the drawing. The examiner scores the test by examin-
ing the drawing for each of seven specific elements found on the ADReS score
sheet (see page 28 for score sheet).
2
Rapid pace walk
This is a measure of lower limb strength, endurance, range of motion, and bal-
ance. A 10-foot path is marked on the floor with tape. The subject is asked to
walk the 10-foot path, turn around, and walk back to the starting point as quickly
as possible. If the patient normally walks with a walker or cane, he/she may use it
during this test. The total walking distance is 20 feet.
The examiner begins timing the patient when he/she picks up the first foot, and
stops timing when the last foot crosses the finish mark. This test is scored by the
total number of seconds it takes for the patient to walk 10 feet and back.
3
In addition, the examiner should indicate on the scoring sheet whether the patient
used a walker or cane. Scores greater than 9 seconds are associated with an
increased risk of at-fault motor vehicle tasks.
4
1. Freund, B., Gravenstein, S., & Ferris, R. Use of the Clock Drawing Test as a Screen for Driving Compe-
tency in Older Adults. Presented at the American Geriatrics Society Annual Meeting, Washington, DC;
May 9, 2002; and Personal correspondence with B. Freund dated September 16, 17 and 19, 2002.
2. Ibid.
3. Staplin, L., Lococo, K. H., Stewart, J., & Decina, L. E. (1999, April). Safe Mobility for Older People
Notebook. NHTSA Report No. DOT HS 808 853. Washington, DC: National Highway Trafc Safety
Administration.
4. Staplin, L., Gish, K. W., & Wagner, E. K. (2003). MaryPODS revisited: updated crash analysis and
implications for screening program implementation. J Safety Res. 34:389–397.
25Chapter 3—Assessing Functional Ability
(DHI).
71
Similar to the ADReS battery,
the program has not yet been validated
in a large cohort of older adult drivers,
but the subcomponents have been
found to correlate with at-fault crash
risk.
72
Furthermore, the DHI did appear
to discriminate drivers with a history of
a crash from those without crashes in a
small cohort of drivers. In addition, this
battery of tests appears feasible and
acceptable to older drivers as a screen
for functional impairments.
73
Additional cognitive domains that have
been linked with driving impairment
include vigilance or sustained attention.
Although many older drivers may make
only short trips, some illnesses such as
untreated obstructive sleep apnea cause
persistent sleepiness or impaired atten-
tion. This risk would be present in this
example regardless of the duration of
the driving episode. In addition, many
older adults travel long distances for
vacations and to visit relatives, making
the ability to sustain attention over
time critical.
Language skills are necessary to read
trafc signs and are critical in knowing
the speed limit, identifying construc-
tion zones, and comprehending other
important informational cues along the
roadway. Geographic orientation refers
to the skill of nding unfamiliar routes
(e.g., map reading or using MapQuest)
or knowing the way to familiar places.
This skill likely involves executive
function, short- and long-term memory,
and language abilities. Impairment in
these cognitive domains have not been
well studied in regard to driving out-
comes, but could play a role in accident
causation in selected groups of medically
impaired drivers.
71. DrivingHealth.com. DrivingHealth Inventory.
www.drivinghealth.com/screening.htm, Accessed
October 14, 2007.
72. Ball, K., Roenker, D.L., & Wadley, V.G., et al.
(2006). Can high-risk older drivers be identied
through performance-based measures in a
Department of Motor Vehicles setting? J Am
Geriatr Soc. 54:77–84.
73. Edwards J. D., Leonard K. M., & Lunsman M.,
et al. (2008). Acceptability and validity of
older driver screening with the DrivingHealth,
Inventory. Accid Anal Prev. 40: 1157–1163.
ADReS (continued)
Manual test of range of motion
The examiner tests the patient’s range of motion by asking him/her to perform the
requested motions bilaterally:
• Neck rotation: “Look over your shoulder like you’re backing up or parking. Now
do the same thing for the other side.”
• Shoulder and elbow flexion: “Pretend you’re holding a steering wheel. Now pre-
tend to make a wide right turn, then a wide left turn.”
• Finger curl: “Make a fist with both of your hands.”
• Ankle plantar flexion: “Pretend you’re stepping on the gas pedal. Now do the
same for the other foot.”
• Ankle dorsiflexion: “Point your toes towards your body.”
The examiner scores the test by choosing the appropriate description of test
performance: (1) Within normal limits; or (2) not within normal limits: good range of
motion with excessive hesitation/pain or very limited range of motion.
Manual test of motor strength
The examiner tests the patient’s motor strength by manually flexing/extending the
patient’s limbs, and asking him/her to resist the examiner’s movements. The exam-
iner should test bilateral:
• Shoulder adduction, abduction and flexion;
• Wrist flexion and extension;
• Hand-grip strength;
• Hip flexion and extension; and
• Ankle dorsiflexion and plantar flexion.
1
Motor strength should be recorded on a scale of 0 to 5, as stated below:
Grade Definition
5/5 Normal strength: movement against gravity with full resistance
4/5 Movement against gravity and some resistance
3/5 Movement against gravity only
2/5 Movement with gravity eliminated
1/5 Visible/palpable muscle contraction, but no movement
0/5 No contraction
2
Strength that is slightly less than grade 5/5 but still greater than 4/5 may
be recorded as 5
–
/5. Similarly, strength that is slightly greater than 4/5 but
still less than 5/5 may be recorded as 4
+
/5. This applies to all other grades
of strength as well.
1. Messinger-Rapport, B. J., & Rader E. (2000). High risk on the highway: how to identify and treat the
impaired older driver. Geriatrics. 55(10):32–45.
2. Maxwell, R. W. (1996). Maxwell Quick Medical Reference, 3rd ed. Tulsa, OK: Maxwell Publishing
Company, Inc.

26 Chapter 3—Assessing Functional Ability
ties, such as range of motion and muscle
function, with driving. Driving impair-
ment has been associated with the
inability to reach above the shoulder.
79
Older adults with physical frailty may
be at increased risk for a motor vehicle
crash,
80,81
and studies have indicated
they appear to be more vulnerable to
injury.
82
Walking less than one block a
day, impaired left knee exion, and foot
abnormalities have been associated with
an adverse driving event.
83
Another
study revealed that more difculty
walking one-quarter mile in comparison
to a control group was associated with
increase crash risk.
84
In ADReS, motor
function is measured through the Rapid
Pace Walk, Manual Test of Range of
Motion, and Manual Test of Motor
Strength measures.
79. Hu Hu, P. S., Trumble, D. A., & Foley, D. J., et
al. (1998). Crash risks of older drivers: a panel
data analysis Accid Anal Prev. 30:569–581.
80. Sims, R. V., McGwin, G., & Allman, R. M., et
al. (2000). Exploratory study of incident vehicle
crashes among older drivers. J Gerontol Series A
Bio Sci Med Sci. 55: M22–27.
81. Marottoli, R. A., Wagner, D. R., Cooney, L. M.,
& Tinetti, M. E. (1994). Predictors of crashes
and moving violations among elderly drivers.
Ann Intern Med; 121:842–846.
82. Kent, R., Funk, J., & Crandall, J. (2003). How
future trends in societal aging, air bag avail-
ability, seat belt use, and eet composition will
affect serious injury risk and occurrence in the
United States. Traff Inj Prev. 4: 24–32.
83. Marottoli, R. A., Wagner, D. R., Cooney, L. M.,
& Tinetti, M. E. (1994). Predictors of Crashes
and Moving Violations Among Elderly Drivers.
Annals of Internal Medicine, 121, 842–846.
84. Sims, R. V., McGwin, G., Pulley, L., et al.
(2001). Mobility Impairments in Crash
Involved Drivers. J Aging Health. 12:430.s.
Executive skills are required to analyze
driving-related stimuli and formulate
appropriate driving decisions. Executive
skills allow a driver to appropriately
make the decision to stop at a red light
or at a green light if a pedestrian is in
the path of the vehicle. The capacity
for this kind of logical analysis tends to
decline with age.
74
Dementia and some medications’ side
effects in the older population may
impact cognition. The fact that crashes
involving older drivers commonly occur
in complex situations in which task
demand exceeds performance suggests
that cognitive limitations may play a
signicant role in crash causation.
75
In the ADReS battery, cognition is
measured through the Trail-Making
Test, Part B, and the Clock Drawing
Test using Freund Scoring Criteria.
74. Beers M. H., & Berkow R. (eds). (2000). The
Merck Manual of Geriatrics. Section 4, Chapter
32: Aging and mental health. Whitehouse
Station, NJ: Merck & Co., Inc.
75. Lundberg C., Hakamies-Blomqvist L., Almkvist
O., & Johansson K. (1998). Impairments
of some cognitive functions are common in
crash-involved older drivers. Accid Anal Prev.
30(3):371–377.
Motor and Somatosensory Function
Driving is a physical activity that
requires motor and somatosensory
abilities such as:
• Muscle strength and endurance;
• Range of motion of the extremities,
trunk, and neck; and
• Proprioception.
76
Motor abilities are necessary for operat-
ing vehicle controls appropriately and
consistently and turning to view trafc.
Even before driving, motor abilities are
needed to enter the car safely and fasten
the seat belt. The natural process of
aging may involve a decline in muscle
strength, muscle endurance, exibility,
and joint stability. (Whether proprio-
ception changes appreciably with age
has not been solidly established.
77
)
Furthermore, osteoarthritis and other
musculoskeletal problems are common
in the elderly. Patients who suffer pain
and limitations from these conditions
may not only experience direct effects on
their driving ability, but also decrease
their physical activity, causing further
decline in motor function.
Most of the difculty in driving an
automobile for patients with muscle
or arthritic disorders involves difcul-
ties with the use of seat belts and keys,
adjusting seats and mirrors, using the
pedals, steering, and transferring in and
out of the car.
78
Several efforts have
been made to correlate functional abili-
76. Marottoli, R. A., & Drickamer M. A. (1993).
Psychomotor mobility and the elderly driver.
Clin Geriatr Med. 9(2):403–411.
77. Ibid.
78. Jones, J. G., McCann, J., & Lassere, M. N.
(1991). Driving and arthritis. Br J Rheumatol. 30
361–364.
27Chapter 3—Assessing Functional Ability
ADReS score sheet
When administering the ADReS
battery, you may nd it helpful to use
the ADReS Score Sheet which can be
found at the end of this chapter. This
form may be photocopied, lled out,
and placed in the patient’s chart. The
ADReS Score Sheet presents the tests in
the simplest order of administration and
provides space for recording test results.
We also recognize that these tests may
not necessarily be performed by the
physician but assigned to ofce staff
such as the nurse or physician extender.
CPT
®
codes for components of the
ADReS battery are provided in Appen-
dix A, and the ADReS Score Sheet can
serve as documentation for these codes.
Although you may administer the tests
in the order you prefer, we recommend
the following sequence:
• Visual Fields by Confrontation
Testing;
• Snellen E Chart—If your ofce has
a long hallway, hang the chart at the
end of the hallway and mark a 20-foot
distance on the oor with tape. Have
the patient stand at the tape.
• Rapid Pace Walk—Mark a 10-foot
distance on the oor. With the
patient already standing at the
20-foot mark, have him/her walk
to the 10-foot mark, then back.
• Manual Test of Range of Motion—
This is performed when the patient
has returned to the examination
room.
• Manual Test of Motor Strength;
• Clock Drawing Test—Ask the patient
to turn over the Trail Making Test
sheet and draw a clock on the
blank side.
• Trail Making Test, Part B.
A discussion of these tests’ efcacy,
scoring, and recommended interven-
tions based on performance is included
in the next chapter.
28 Chapter 3—Assessing Functional Ability
Assessing Driving Related Skills (ADReS) Score Sheet
Patient’s name: ______________________________________________________ Date: __________________________
1. Visual elds: Shade in any areas of decit.
2. Visual acuity: _________ OU __________ OS _________OU
Was the patient wearing corrective lenses? If yes, please specify: ______________________________________________
If either eye acuity worse than 20/40, consider referral to ophthalmologist.
3. Rapid pace walk: ____________ seconds
(>10 secs, abnormal and consider referral for driving evaluation and/or evaluation of gait disorder) Was this performed
with a walker or cane? If yes, please specify: ______________________________________________________________
4. Range of motion: Specify ‘Within Normal Limits’ or ‘Not WNL.’ If not WNL, describe.
Right Left
Neck rotation
Finger curl
Shoulder and elbow exion
Ankle plantar exion
Ankle dorsiexion
Plan for any deciencies (consider referral to OT/PT, address pain management, if indicated, and/or referral to driving
clinic for vehicle modication)
5. Motor strength: Provide a score on a scale of 0–5.
Right Left
Shoulder adduction
Shoulder abduction
Shoulder exion
Wrist exion
Wrist extension
Hand grip
Hip exion
Hip extension
Ankle dorsiexion
Ankle plantar exion
Plan for any deciencies: (consider referral to OT/PT or driving clinic for vehicle modication)
LPatient’s R
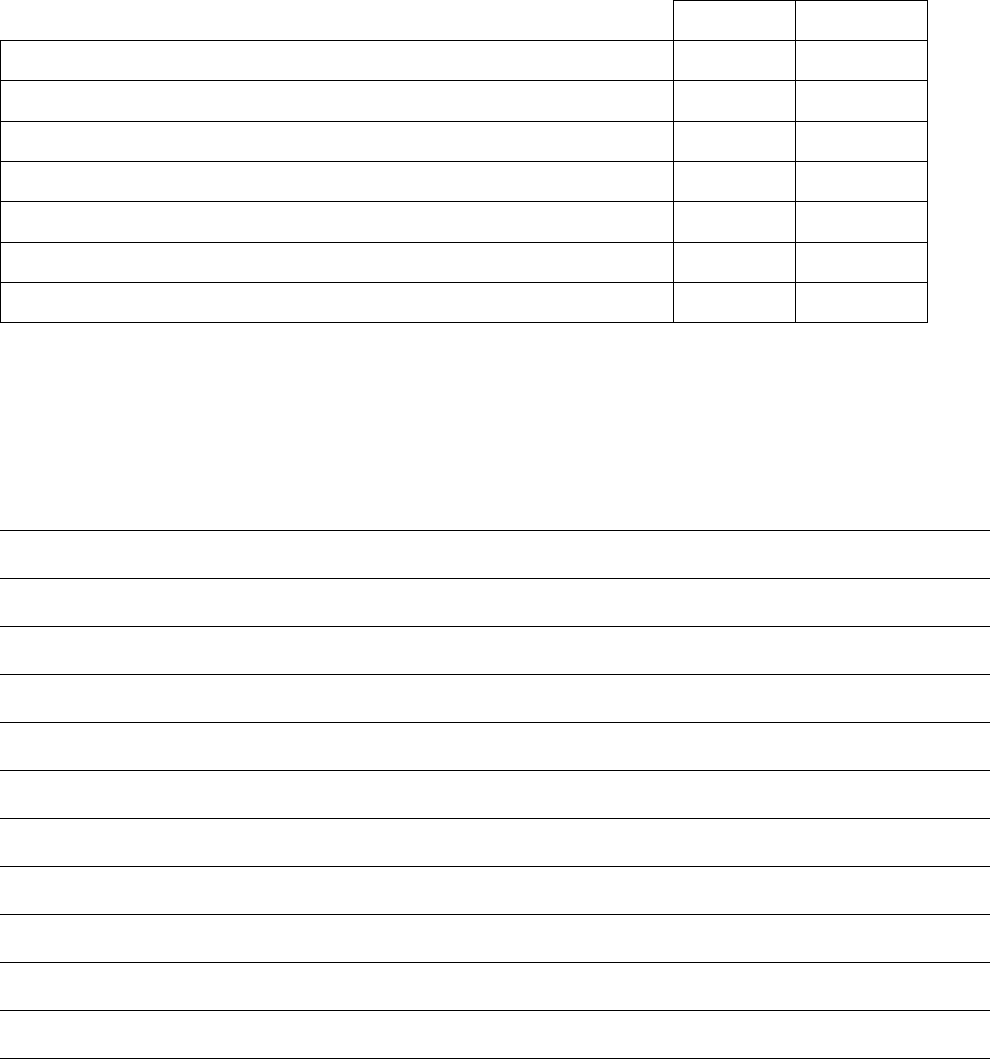
29Chapter 3—Assessing Functional Ability
ADReS Score Sheet (continued)
Patient’s name: ______________________________________________________ Date: __________________________
6. Trail-Making Test, Part B: ____ seconds
(score greater than 180 secs abnormal, consider referral to driving evaluation clinic and/or work-up for
cognitive/visual/motor impairment )
7. Clock drawing test: Please check ‘yes’ or ‘no’ to the following criteria
Yes No
Only the numbers 1-12 are included (no duplicates or omissions)
The numbers are drawn inside the clock circle
The numbers are spaced equally or nearly equally from each other
The numbers are spaced equally or nearly equally from the edge of the circle
One clock hand correctly points to 2
There are only two clock hands
There are no intrusive marks, writing or hands indicating incorrect time
(any abnormal elements consider referral to driving evaluation clinic and/or work-up for cognitive/visual/
motor impairment)
Assessment/Plan:
30
Trail-Making Test, Part B Patient’s name: _________________________ Date: __________________________
13
8
9
I
4
B
3
1
5
C
H
12
G
A
E
F
K
2
L
6
11
J
7
D
10
End
Begin

CHAPTER 4
Physician Interventions
33Chapter 4—Physician Interventions
Visual acuity
Although many States currently require
far visual acuity of 20/40 for an unre-
stricted license, there is a paucity of
evidence that links static visual acuity
to crash risk. In fact, studies undertaken
in some States have demonstrated that
there is no increased crash risk between
20/40 and 20/70, resulting in several
new State requirements.
88
However,
some studies have found that those
States that require visual testing during
license renewal for older adults have
lower crash rates.
89,
90
General recommendations on visual
acuity and driving are stated below.
Please note that these recommenda-
tions are subject to each State’s
licensing requirements.
For visual acuity greater than
20/40 (e.g., more impaired), the
physician should:
• Ensure that the underlying cause of
vision loss is adequately treated, if
treatment is possible. If the patient
is not currently under the care of an
ophthalmologist or optometrist,
referral is recommended.
• Recommend that the patient has and
uses the appropriate glasses or contact
lenses. Again, if the patient is not
currently under the care of a special-
ist, referral is recommended.
88. American Academy of Ophthalmology. Policy
Statement: Vision Requirements for Driving.
Approved by Board of Trustees, October 2001.
89. Levy, D. T. (1995). The relationship of age
and State license renewal policies to driving
licensure rates. Accid Anal Prev. 27(4):461–467.
90. Shipp, M. D. (1998). Potential human eco-
nomic cost-savings attributable to vision testing
policies for driver license renewal, 1989–1991.
Optom Vis Sci. 75:103–118.
On the ADReS battery, Mr. Phillips
takes 11 seconds to perform the
Rapid Pace Walk. His visual acu-
ity is 20/50 OD and 20/70 OS. His
motor strength is 4-/5 in both lower
extremities, and 4/5 in both upper
extremities. He has limited range
of motion on neck rotation; ankle
plantar exion and dorsiexion are
within normal limits. It takes him
182 seconds to complete the Trail-
Making Test, Part B, and his clock
drawing is scored as “normal” for
all seven criteria.
Now that Mr. Phillips has undergone
ADReS, what does his performance
indicate? In this chapter, we help you
interpret your patient’s test performance
by providing you with scoring cut-offs.
86
We have also provided examples of
interventions to help you manage and
treat any functional decits that are
identied through ADReS. Recently, the
ADReS battery has been shown to have
high levels of inter-rater reliability.
87
As you review the recommended in-
terventions, remember that the goal of
physician evaluation is to identify, cor-
rect, or stabilize any functional decits
that may impair the patient’s driving
performance and refer to a driver reha-
bilitation specialist (DRS), if appropri-
ate (for more details, see Chapter 5).
86. Please be aware that the recommendations
stated in this chapter are subject to your State’s
reporting laws and DMV requirements.
87. Posse, C., McCarthy, D. P., & Mann, W. C.
(2006). A pilot study of interrater reliability of
the assessment of driving-related skills: Older
Driver Screening Tool. Top Geriatr Rehab The
Older Driver, Part 2. 22: 113–120.
Despite your encouragement, Mr.
Phillips (introduced in Chapter 2)
hesitates to take the Assessment
of Driver Related Skills (ADReS)
battery because he says, “I don’t
see the need for it.” You reiterate
your concerns for his safety, and
give him a copy of the Am I a Safe
Driver? self-assessment handout to
take home. In addition, you counsel
Mr. Phillips on the Successful Aging
Tips and Tips for Safe Driving hand-
outs. Mr. Phillips agrees to allow
his son to observe his driving, and
you give the son the How to Assist
the Older Driver handout (see Ap-
pendices). You document all of this
in Mr. Phillips’ chart and schedule
a follow-up visit. Alternatively, the
Hartford guide “At the Crossroads”
has a driving behavior checklist that
could be lled out by family members
(p.11).
85
Although not systemati-
cally studied, this type of objective
evaluation could also be revealing.
At Mr. Phillips’ next visit, you ask
him if he has tried putting any of the
Tips for Safe Driving into practice.
He admits that he had another close
call, and his son states he observed
several driving errors. These moti-
vated Mr. Phillips to complete the
self-assessment. He claims that the
self-assessment was an eye-opening
experience, and he is now willing to
undergo ADReS.
85. The Hartford. Alzheimers, Dementia &
Driving. Hartford, CT. www.thehartford.com/
alzheimers/brochure.html. Accessed October
24, 2007.
CHAPTER 4
Physician Interventions
34 Chapter 4—Physician Interventions
• Recommend that the patient reduce
the impact of decreased visual acuity
by restricting travel to low risk areas
and conditions (e.g., familiar sur-
roundings, non-rush hour trafc,
low speed areas, daytime, and good
weather conditions).
• Be aware that the patient may require
more frequent (e.g., yearly) assessment
of visual acuity to detect further
visual decline caused by chronic,
progressive diseases.
For visual acuity less than
20/70 (e.g., more impaired),
the physician should:
• Follow the recommendations stated
above, and
• Recommend an on-road assessment
performed by a DRS to evaluate the
patient’s performance in the actual
driving task, where permitted and
available (see Chapter 5).
For visual acuity less than
20/100 (e.g., more impaired),
the physician should:
• Follow the recommendations stated
above, and
• Recommend that the patient not
drive unless safe driving ability can be
demonstrated in an on-road assess-
ment performed by a DRS, where
permitted and available.
Visual fields
Research shows that visual eld loss
can signicantly affect driving safety. In
examining 10,000 volunteer California
license applicants, Johnson and Keltner
found signicant deterioration in visual
elds among drivers over age 60. In
addition, they found that drivers with
binocular visual eld loss had driving
crash and conviction rates more than
twice as high as age- and gender-
matched drivers with normal elds.
91
Recently, studies focused on a more
homogenous group of older adults with
a specic disease (e.g., glaucoma) that
91. Johnson, C. A., & Keltner, J. L. (1983).
Incidence of visual eld loss in 20,000 eyes
and its relationship to driving performance.
Arch Ophthalmol. 101:371–375.
is known to impair visual elds have
found correlation with increased crash
risk in patients with moderate to severe
eld defects.
92, 93
While it is known that an adequate
visual eld is important for safe driv-
ing, there is no conclusive evidence
to dene what is meant by “adequate.”
Most likely, this varies widely from
patient to patient and may depend on
the presence of other co-morbidities.
For example, a driver with a restricted
visual eld but excellent scanning
ability may drive as safely as a driver
with an unrestricted visual eld but
poor neck rotation.
94
General recommendations on visual
eld and driving are stated below. Physi-
cians should be aware of their States’
specic visual eld requirements, if any,
and adhere to them.
For visual eld defects noted on
clinical examination, the physician
should:
• Ensure that the underlying cause of
visual eld loss is adequately treated,
if treatment is possible. If the patient
is not currently under the care of an
ophthalmologist or optometrist,
referral is recommended.
• Automated visual eld testing may
help dene the extent of the defect,
and ophthalmologists have a number
of useful instruments for measuring
visual elds.
• For binocular visual eld of question-
able adequacy (as deemed by clinical
judgment), an on-road assessment
performed by a DRS is strongly rec-
ommended. Through driving rehabili-
tation, the patient may learn how to
92. Szlyk, J. P., Mahler, C. L., Seiple, W., et al.
(2005). Driving performance of glaucoma
patients correlates with peripheral visual eld
loss. J Glaucoma. 14:145–150.
93. McGwin, G., Jr., Mays, A., Joiner, W., et al.
(2004). Is glaucoma associated with motor
vehicle collision involvement and driving
involvement and driving avoidance? Invest
Ophthalmol Vis Sci. 45: 3934–3939.
94. American Academy of Ophthalmology. Policy
Statement: Vision Requirements for Driving.
Approved by Board of Trustees, October 2001.
compensate for decreased visual elds.
In addition, the DRS may prescribe
enlarged side- and rear-view mirrors
as needed and train the patient in
their use.
• Be aware that the patient may require
re-testing of visual elds in the future
for visual eld defects caused by
chronic, progressive diseases.
Cognition
Although the following cognitive tests
are scored separately, interventions are
recommended if the patient reaches
designated cut-off values (as described
below) on either of them.
Trail-Making Test, Part B
A time for completion of greater than
3 minutes (180 seconds) signals a need
for intervention,
95
such as a review of
causes for the abnormal result (e.g.,
dementia, sedating medication) and/or
referral to a DRS.
Numerous studies have demonstrated
an association between performance on
the Trail-Making Test, Part B (TMT-B),
and cognitive function and/or driving
performance. In a study of 1,700 drivers
65 and older who were applying for
renewal of their North Carolina driver’s
license, TMT-B test results were strong-
ly associated with recent prior crash
involvement.
96
A study of 105 drivers
in Nebraska 65 to 88 years old showed
that on-road driving performance sig-
nicantly correlated to TMT-B perfor-
mance (correlation coefcient -0.42).
97
Most recently, data from the Maryland
95. Staplin, L., Lococo K.H., Gish K.W., &
Decina L.E. (2003). Model driver screening
and evaluation program & Maryland pilot older
driver study. NHTSA Report Number DOT HS
809 581. Washington, DC: National Highway
Trafc Safety Administration.
96. Stutts, J. C., Stewart, J. R., & Martell C.
(1998). Cognitive test performance and
crash risk in an older driver population.
Accid Anal Prev. 30(3):337–346.
97. Tarawneh, M. S., McCoy, P. T., Bishu, R. R.,
Ballard, J. L. (1993). Factors associated
with driving performance of older drivers.
Transportation Res Record. 1405:64–71.

35Chapter 4—Physician Interventions
Your patients may be unaware of the
potential effects of polypharmacy on
cognitive ability and driving.
• If possible, treat the underlying
disorder and/or adjust the medica-
tion regimen as needed. Remember,
it is critical that every patient have a
complete evaluation to identify the
underlying cause or causes and receive
proper treatment.
• Refer the patient to a neurologist,
psychiatrist, or neuropsychologist
for diagnosis or treatment as needed.
If the patient has a degenerative
dementia, such as Alzheimer’s disease,
begin treatment with appropriate
medications as indicated.
• Recommend an on-road assessment
performed by a DRS to assess the
patient’s performance in the actual
driving task. An initial comprehensive
on-road assessment with retesting at
regular intervals is particularly useful
for progressive dementing illnesses.
Strongly recommend that the patient
begin exploring alternative forms of
transportation now, and encourage
him/her to involve family members/
caregivers in these discussions.
It is again emphasized that these tests
should not be the sole determinant as
to whether an older adult should drive,
and this was the conclusion of a recent
review on this subject.
103
However,
impairments on these tests are associated
with increased risk, and referral for
further evaluation, such as performance-
based road testing, should be consid-
ered. In addition, it is unlikely that
future tness-to-drive evaluations will
rely on one test but likely will employ
a battery of tests.
104
If the patient’s performance
warrants interventions, the
physician should:
• Gather (or refer for) more informa-
tion to include detailed history
and examination of cognitive and
functional abilities, as needed;
• Identify or interview a reliable
informant (e.g., family member or
caregiver) who can assist with the
evaluation;
• Identify the cause of the
cognitive decline;
¤ Check for reversible causes
of cognitive decline;
105
¤ Screen for depression;
106
¤ Review the patient’s medication
regimen and the side effects of
the medications, and question the
patient about the onset of cognitive
decline in conjunction with new
medications or dosage changes.
103. Langford, J. (2008). Usefulness of off-road
screening tests to licensing authorities when
assessing older driver tness to drive. Trafc Inj
Prev. 9:328–335.
104. Stave, W. B., Justiss, M. D., McCarthy, D. P., et
al. (2008). Predictability of clinical assessments
for driving performance. J Safety Res. 39:1–7.
105. Based on history, examination, and cogni-
tive testing, order laboratory tests as needed
to evaluate for causes of cognitive decline:
CBC for anemia or infection; comprehensive
metabolic prole for electrolyte imbalance and
renal function; nger stick for blood sugar, pulse
oximetry for hypoxia, TSH for hypothyroidism;
liver function tests; vitamin B12 and folate
for vitamin deciency, and based on the prior
probability, noncontrast CT or MRI scan.
106. Knopman, D. S. (2001). Practice parameter: di-
agnosis of dementia (an evidence-based review).
Report of the Quality Standards Subcommittee
of the American Academy of Neurology.
Neurology. 56(9):1143–1153.
Pilot Older Driver Study
98
demonstrated
a signicant correlation between TMT-
B performance and future at-fault crash
in the license renewal sample.
Clock Drawing Test, Freund Clock
Scoring for Driving Competency
Any incorrect or missing element on
the Freund Clock Scoring Criteria
signals a need for intervention, such
as a review of causes for the abnormal
result (e.g., dementia) and/or referral
to a DRS.
Clock Drawing Tests (CDT) have been
found to correlate signicantly with
traditional cognitive measures, and to
discriminate healthy individuals from
those with dementia.
99
Of all the mea-
sures that have correlated with impaired
driving performance in older adults
with dementia, tests of visuospatial
skill ability have had the highest level
of prediction.
100
Several versions of the
CDT are available, each varying slightly
in the method of administration and
scoring.
101
The Freund Clock Scoring is
based on seven “principal components”
(as outlined on the ADReS Score
Sheet), which were derived by analyz-
ing the clock drawings of 88 drivers 65
and older against their performance on
a driving simulator.
102
Errors on these
principal components correlated signi-
cantly with specic hazardous driving
errors, signaling the need for formal
driving evaluation.
98. Ball, K. K., Roenker, D. L., Wadley, V. G., et al.
(2006). Can high-risk older drivers be identied
through performance-based measures in a
Department of Motor Vehicles setting?
J Am Geriatr Soc. 54:77–84.
99. Royall, D. R., Cordes, J. A., & Polk, M. J.
(1998). Clox: An executive clock drawing task.
J Neurol Neurosurg Psychiatry. 64:588–594.
100. Reger, M. A., Welsh, R. K., Watson, G. S., et al.
(2004). The relationship between neuropsy-
chological functioning and driving ability in
dementia: a meta-analysis. Neuropsychology.
18:85–93.
101. Royall, D. R., Mulroy, A R., Chiodo, L K.,
Polk, M J. (1999). Clock drawing is sensitive to
executive control: a comparison of six methods.
J Gerontol Psychol Sci. 54B(5):328–333.
102. Freund, B., Gravenstein, S., Ferris, R., et al.
(2005). Drawing clocks and driving cars. J Gen
Intern Med. 20:240–244.
36 Chapter 4—Physician Interventions
Motor ability
Although the following tests are scored
separately, interventions are recom-
mended if the patient reaches designated
cut-off values (as described below) on
any of the individual tests.
Rapid Pace Walk
A time for completion of greater than 9
seconds signals a need for intervention,
107
such as determination of the cause for
slowed gait speed (e.g., Parkinson’s dis-
ease) and/or referral to a DRS.
The Rapid Pace Walk assesses lower
limb mobility, trunk stability, and
balance. In a prospective cohort study
of 283 drivers 72 and older, subjects
who took longer than 7 seconds to
complete the test were twice as likely
to experience an adverse trafc event
(crash, violation, or being stopped by
the police) in the year following the
test.
108
More recently, data from the
Maryland Pilot Older Driver Study—a
study of almost 2,000 drivers over age
55 who were license renewal applicants-
-demonstrated a correlation between
performance on the Rapid Pace Walk
and future at-fault crash in the license
renewal sample (odds ratio 1.70).
109
Manual Test of Motor Strength
Less than grade 4/5 strength in either
upper extremity or the right lower ex-
tremity signals a need for intervention,
such as vehicle modication. (If the
patient drives a vehicle with manual
transmission or reports using both feet
to operate the brake and accelerator
pedals,
110
this applies to the left lower
extremity as well.)
107. Staplin, L., Gish, K. W., & Wagner, E. K.
(2003). MaryPODS revisited: updated crash
analysis and implications for screening program
implementation. J Safety Res. 34:389–397.
108. Marottoli, R. A., Cooney, L. M., Wagner, R.,
Doucette, J., & Tinetti, M. E. (1994). Predictors
of automobile crashes and moving viola-
tions among elderly drivers. Ann Intern Med.
121(11):842–846.
109. Ibid.
110. Although this is not considered the recom-
mended way of driving, many older drivers
initially learned to drive using both feet to
operate the pedals.
(Continues on next page)
Figure 4.1: Dementia and driving
We encourage all physicians to pursue a diagnosis of dementia. Dementia is one
of the most serious disorders in the older population, and affects 4 to 5 million
persons in the United States.
1
However, it is frequently unrecognized and undocu-
mented by primary care physicians
2
—a situation that is particularly unfortunate
since early treatment and planning may stabilize or slow the course of the disease,
improve the safety and comfort of the patient, and reduce caregiver stress.
With regard to driving, patients with progressive dementia ultimately become
unsafe to drive, yet often lack the cognitive abilities to be aware of their limitations.
When it becomes unsafe for these patients to drive, it frequently falls on family
members and caregivers to enforce driving cessation and arrange alternative
forms of transportation. With early diagnosis, patients and their families have
the opportunity to plan ahead for a smooth transition from driving to non-driving
status. Valuable information about an individual’s driving ability may come from
observations of informants. (For a more detailed discussion of driving cessation
and the dementia patient, see Chapter 6. Several recent reviews in the literature
on this topic also may be helpful to the clinician.
3, 4
)
Figure 4.2: The copilot phenomenon
Copiloting refers to a situation in which an individual drives with the assistance of a
passenger who provides navigational directions and instructions on how to drive.
Patients with dementia may rely on passengers to tell them where to drive and
how to respond to driving situations, while patients with vision deficits may ask
passengers to alert them to traffic signs and signals.
The use of copilots is not rare. In a study of the prevalence and cessation of driving
among older men with dementia, about 10 percent of the 59 subjects who were
still driving relied on copilots.
5
Patients should be advised to not continue driving
unless they are capable of driving safely without the use of a copilot. In many traffic
situations, there is insufficient time for the copilot to detect a hazard and alert the
driver, and for the driver to then respond quickly enough to avoid a crash. In such
situations, the driver places not only him/herself in danger, but also the copilot and
other passengers. Furthermore, the use of copilots to meet standards for licen-
sure raises questions of who, exactly, is licensed to drive; how the presence of the
copilot can be ensured; and what standards for medical fitness-to-drive should be
applied to the copilot.
6
Patients who are not safe to drive should be recommended to stop driving, regard-
less of their need or use of a copilot. Copilots should never be recommended to
unsafe drivers as a means to continue driving. Instead, efforts should focus on
helping the patient find safe transportation for him/herself and the family members
who may depend on them. Conversely, some safe drivers feel more comfortable
driving with a passenger to give them company and help with navigation. While
using a passenger to assist as a copilot with navigation is an acceptable practice,
use of a copilot to provide instruction on how to drive is not recommended.
As long as these drivers have the ability to drive safely on their own, passenger
assistance is an acceptable and advisable practice.
1. Beers, M.H., &Berkow, R. (2000). The Merck Manual of Geriatrics. Section 5, Chapter 40. Whitehouse
Station, NJ: Merck & Co., Inc.
2. Valcour, C. G., Masaki, K. H., Curb, J. D., & Blanchette, P. L. The detection of dementia in the primary
care setting. Arch Intern Med. 160:2964–2968.
3. Brown, L. B., & Ott, B. R. (2004). Driving and dementia: a review of the literature. J Geriatr Psychiatry
Neurol. 17:232–240.
4. Carr, D. B., Duchek, J. M., Meuser, T. M., et al. (2006). Older adult drivers with cognitive impairment.
Am Fam Physician. 73:1029–1034.
5. Foley, D. J., Masaki, K. H., Ross G. W., &Whwite L. R. (2000). Driving cessation in older men with
dementia. J Am Geriatr Soc. 48(8):928–930.
6. Fox, G. F., & Bashford, G. M. (1997). Dementia and driving: balancing
personal independence and public safety. Med J Australia. 167:406–407.

37Chapter 4—Physician Interventions
The manual test of motor strength
evaluates separate muscle groups in
both the upper and lower limbs. The
U.S. Public Health Service guidelines
on musculoskeletal ability and driving
state that a driver should have at least
grade 4/5 strength in the right lower
extremity and both upper extremities.
111
The physician should also be aware
that the amount of strength required for
safe driving may depend on the vehicle
driven by the patient. For example, a
patient who drives an older car that
does not have power steering or oper-
ates a large vehicle (e.g., a school bus,
which is not uncommon for retirees)
may require greater strength to safely
drive the vehicle.
Manual Test of Range of Motion
If the patient’s range of motion is not
within normal limits (i.e., if the patient
has a good range of motion with exces-
sive hesitation/pain or a very limited
range of motion), this signals the need
for intervention. Recently, the inability
to recognize an object that is presented
directly behind a patient (e.g., intact
cervical range of motion) was correlated
with increased risk of a motor vehicle
crash.
112
Scoring for range of motion is based on
simple dichotomous outcomes (normal
vs. impaired), and this is due to several
reasons: (1) Physicians are not usually
trained in use of goniometers nor have
the devices in the ofce setting; (2)
range of motion requirements vary with
automobile design, and thus it is dif-
cult to specify exact requirements;
(3) as discussed in the visual elds
section, the impact of limited range of
motion on driving safety also depends
on other functions; and (4) as with all
the other tests in the ADReS battery,
a patient’s poor performance should be
a stimulus for optimization of func-
111. Marottoli, R. A., & Drickamer, M. A. (1993).
Psychomotor mobility and the elderly driver.
Clin Geriatr Med. 9(2):403–411.
112. Ball, K. K., Roenker, D. L., Wadley, V. G., et al.
(2006). Can high-risk older drivers be identied
through performance-based measures in a
Department of Motor Vehicles setting? J Am
Geriatr Soc. 54:77–84.
tion, rather than for immediate driving
restrictions.
If the patient’s performance on this
test is not within normal limits, the
physician should be certain to elicit
the reason: Do these movements cause
muscle or joint pain? Does the patient
complain of tight muscles or stiff joints?
Do these movements cause a loss of
balance? Patients with a history of falls
have been noted to be at increased risk
of motor vehicle crashes.
113
Knowing
the answers to these questions will help
in the management of the patient’s
physical limitations.
If the patient’s performance war-
rants interventions, the physician
should:
• Encourage the patient to drive a
vehicle with power steering and
automatic transmission, if he/she
does not already do so.
• Recommend that the patient
maintain or commence a consistent
regimen of physical activity, including
cardiovascular exercise, strengthening
exercises, and stretching. (Successful
Aging Tips, in Appendix B, suggests
some exercises.)
• Refer the patient to a physical
therapist or occupational therapist
as needed for training and exercises
to improve strength and/or range of
motion.
• Provide effective pain control if the
patient’s range of motion and mobil-
ity are limited by pain. This may
include prescribing analgesics or med-
ications that treat the underlying dis-
order (e.g., a urate-lowering drug for
gout), or changing when the patient
takes pain medications so that relief is
achieved prior to driving. Please note
that many analgesics (including nar-
cotics and skeletal muscle relaxants)
have the potential to impair driving
ability, and may be more deleteri-
ous to driving performance than the
instigating pain. These medications
113. Margolis, K. L., Kerani, R. P., McGovern, P., et
al. (2002). Risk factors for motor vehicle crashes
in older women. J Gerontol Series A-Bio Sci Med
Sci. 57:M186–191.
should be avoided, if possible, or
prescribed in the lowest effective dose
possible. Patients should be advised to
refrain from driving when rst taking
these medications until they know
whether they are tolerated.
• Refer the patient to a specialist for
management of any joint disease,
podiatry issues, or neuromuscular
problems. Post-stroke patients with
residual decits that interfere with
the patient’s handling of car controls
should also be referred.
• Recommend an on-road assessment,
performed by a DRS, to assess the
patient’s performance in the actual
driving task. A comprehensive on-
road assessment is particularly useful
for assessing the impact of physical
fatigue on the patient’s driving skills.
• The DRS may prescribe adaptive de-
vices as needed (e.g., a spinner knob
on the steering wheel to compensate
for poor hand grip or an extended
gear shift lever to compensate for
reduced reach), and train the patient
in their use.
What do you do next?
After administering ADReS, you can
follow one of three courses of action.
(See also the Physician’s Plan for Older
Drivers’ Safety, Figure 1, Chapter 1.)
If the patient performs well on all three
sections of the ADReS battery, you may
advise him/her that there are no medical
contraindication to safe driving and no
need for further work-up or treatment.
Counsel the patient on health mainte-
nance by providing the Successful Aging
Tips and Tips for Safe Driving handouts,
and periodically follow-up on the
patient’s driving safety. However, if
there is evidence of a new onset of
impaired driving behaviors (e.g., a
decline from baseline) as described by
the patient and/or family, further
evaluation may be warranted despite
a normal score.
If the patient performs poorly on any
section of ADReS, but the causes of
poor performance are medically correct-
able, pursue medical treatment until the
38 Chapter 4—Physician Interventions
patient’s function has improved to the
fullest extent possible. The patient may
need to be counseled to limit driving as
treatment proceeds. Assess the patient’s
level of improvement with repeat
administration of ADReS. If the patient
now performs well on all three sections
of the ADReS battery, counsel him/her
on health maintenance as above.
If the patient’s poor performance on the
ADReS battery cannot be medically
corrected, or if the patient’s function
shows no further potential for improve-
ment with medical interventions, refer
him/her to a DRS.
The ADReS battery is useful as an
in-ofce assessment, but it does not
evaluate the patient’s performance in
the actual driving task, and the results
even if abnormal are not sufcient to
recommend driving cessation. For this,
an on-road assessment performed by
a DRS is needed. The DRS can more
specically determine the patient’s
level of driving safety and correct his/
her functional impairments, if possible,
through adaptive techniques or devices.
The role of the DRS is discussed in the
next chapter.

CHAPTER 5
The Driver
Rehabilitation Specialist

41Chapter 5—The Driver Rehabilitation Specialist
tion Specialists (ADED)
115
by
fullling education and experience
qualications
116
and passing a certica-
tion examination.
117
Certied driver
rehabilitation specialists (CDRSs)
renew their certication every three
years by fullling a minimum amount
of contact hours. While many DRSs
either hold certication or are in the
process of obtaining the necessary
education and experience to sit for
the examination, certication is not
required to practice driver rehabilita-
tion nor for ADED membership.
115. The acronym ADED was retained when the
association changed its name from the Associa-
tion of Driver Educators for the Disabled to its
current name.
116. Candidates must fulll one of the following
requirements: A. An undergraduate degree or
higher in a health-related area of study with
one year full time experience in degree area
of study and an additional one year full time
experience in the eld of Driver Rehabilitation;
B. Four year undergraduate degree or higher
with a major or minor in Trafc Safety and/or a
Driver and Trafc Safety Endorsement with one
year full time experience in Trafc Safety and
an additional two years of full time experience
in the eld of Driver Rehabilitation; C. Two
year degree in health-related area of study with
one year experience in degree area of study and
an additional three years full time experience
in the eld of Driver Rehabilitation; D. Five
years of full time work experience in the eld
of Driver Rehabilitation. Association of Driver
Rehabilitation Specialists: Driver Rehabilitation
Specialist Certication Exam fact sheet (www.
driver-ed.org/public/articles/index.cfm?Cat=10).
117. Examination content includes (1) program
administration, (2) the pre-driving assessment,
(3) the in-vehicle assessment, (4) the on-road
evaluation, (5) interpretation of assessment
results, and (6) planning and implementation
of recommendations. Association of Driver
Rehabilitation Specialists: Driver Rehabilitation
Specialist Certication Exam fact sheet
(www.driver-ed.org/public/articles/index.cfm?Cat=10).
Despite your medical interventions,
your patients will sometimes continue
to demonstrate functional impairments
that may impair their driving perfor-
mance. In these cases, a DRS is an
excellent resource. A DRS can perform
a more in-depth functional assessment
and evaluate performance with an ac-
tual driving task. Based on the patient’s
performance, the DRS can recommend
that he/she continue driving with or
without further restrictions or interven-
tions, recommend adaptive techniques
and devices to overcome functional
decits, or recommend that the
patient cease driving and offer
mobility counseling.
This chapter provides you with
information you should have when
you refer your patient to a DRS.
What is a driver rehabilitation
specialist?
A DRS is one who “plans, develops,
coordinates and implements driving ser-
vices for individuals with disabilities.”
114
DRSs are often occupational therapists
who undergo additional training in
driver rehabilitation. Aside from occu-
pational therapy, DRSs also come from
backgrounds such as physical therapy,
kinesiotherapy, psychology, and driver
education.
Many DRSs receive certication from
the Association for Driver Rehabilita-
114. Association of Driver Rehabilitation Specialists:
Driver Rehabilitation Specialist Certication
Exam fact sheet (www.driver-d.org/public/articles/
index.cfm?Cat=10).
After scoring Mr. Phillips’ (introduced
in previous chapters) performance
on the ADReS battery, you discuss
the results with him. You assure him
that he scored well on the cognitive
tests, but that his performance on
the visual and motor tasks indicates
a need for further evaluation and
treatment.
You recommend that Mr. Phillips
make an appointment with his oph-
thalmologist, whom he has not seen
for over a year. You also recommend
that he begin exercising regularly
by walking for 10-minute intervals,
three times a day, and stretching
gently afterwards. His son, who is
present at the clinic visit, offers to
exercise with him several times a
week. You schedule Mr. Phillips to
return to your clinic in one month.
When Mr. Phillips arrives for his
follow-up appointment, he is wear-
ing new glasses. His vision with the
new glasses is 20/40 OU. You retest
his motor skills, and he is now able
to complete the Rapid Pace Walk
in 8.0 seconds. His lower extremity
strength has improved to 4+/5, but
his range of motion on nger curl
and neck rotation remain restricted.
With Mr. Phillips’ agreement, you
refer him to a driver rehabilitation
specialist (DRS) for an evaluation
and adaptive equipment, if necessary.
CHAPTER 5
The Driver
Rehabilitation Specialist
42 Chapter 5—The Driver Rehabilitation Specialist
assessment if they meet the minimum
state standards for health and vision,
and the client holds a valid driver’s
license or permit. The on-road assess-
ment is performed in a driver rehabilita-
tion vehicle equipped with dual brakes,
a rear-view mirror and eye-check mirror
for the DRS, and any necessary adaptive
equipment.
Please note that clients who perform
poorly on the clinical assessment may
still undergo on-road assessment. In
these cases, the DRS may recommend
on-road assessment for one of two
reasons: (1) clients who perform poorly
on individual components of the clini-
cal assessment may still demonstrate
safe driving due to over-learning the
driving task; and (2) clients and family
members may need concrete evidence
of unsafe driving, which can only be
documented through observation of
behind-the-wheel performance.
Who can driver rehabilitation
specialists help?
Driver assessment and rehabilitation
are appropriate for a broad spectrum of
visual, physical, and/or cognitive dis-
abilities. DRSs work with clients who
have dementia, stroke, arthritis, low
vision, learning disabilities, limb ampu-
tations, neuromuscular disorders, spinal
cord injuries, mental health problems,
cardiovascular diseases, and other causes
of functional decits.
Vehicle modication can be as straight-
forward as providing extended gear shift
levers, padded steering wheels, or extra/
larger mirrors to patients with arthritis,
and training the client in their use.
It can also be as complex as working
with a client with dementia and his/her
caregivers to determine the individual’s
driving needs, plan driving routes for
the client (e.g., avoiding left hand turns
or busy intersections), supervise practice
drives, and provide close and extended
follow-up.
and the potential for improvement
with retraining is poor. In these
cases, alternative transportation op-
tions are reviewed with the client.
¤ Re-evaluation. This option is
indicated if a client’s function is
expected to improve, or if a client
demonstrates adequate skills to
drive at present but has a progres-
sive disorder that may cause future
decline.
Passenger Vehicle Evaluation
• Assessment of vehicle, vehicle
modications, and equipment needed
for the client’s safe transport as a
passenger.
• Consideration of the needs of the
patient’s family (for example, certain
lifts or tie-down systems may be
recommended due to an assisting
family member’s physical limitations).
Treatment and Intervention
• Adaptive driving instruction or driver
retraining, with or without vehicle
modications.
• Coordination of vehicle modications:
¤ Vehicle consultation: The DRS
serves as a consultant to clients
who are purchasing a new vehicle
to ensure that the vehicle will ac-
commodate the necessary adaptive
equipment.
¤ Vehicle modication recommenda-
tions: The DRS provides written
recommendations for all vehicle/
equipment needs to the client,
third party payer, and vehicle/
equipment dealer.
¤ Vehicle inspection: The DRS is
involved with the client and adap-
tive equipment dealer in a nal
tting to ensure optimal function-
ing of the recommended vehicle/
equipment.
An initial driver evaluation can last
one to four hours, depending on the
client’s presenting disabilities and
driving needs. Following the clinical
assessment, clients undergo an on-road
What do driver rehabilitation
specialists do?
A DRS evaluates the client’s driving
skills, recommends rehabilitation as
needed, and can suggest vehicle and/or
route modications (e.g., such as avoid-
ing left hand turns) to enable the per-
son to resume or continue driving safely.
Although driver rehabilitation programs
vary, most typically include the follow-
ing elements in their evaluation:
Driver Evaluation
• Clinical assessment, including review
of driving history, driving needs, and
license status; review of medical his-
tory and medications; visual/percep-
tual assessment; assessment of range
of motion, motor strength, coordina-
tion, sensation, and reaction time;
and cognitive assessment.
• Functional (on-road) assessment, in-
cluding assessment of vehicle ingress/
egress, mobility aid management (e.g.,
ability to transport a wheelchair or
scooter), vehicle preparation, vehicle
control, adherence to trafc rules and
regulations, environmental awareness
and interpretation, and consistent use
of compensatory strategies for visual,
cognitive, physical, and behavioral
impairments.
• Communication of assessment results
and recommendations to the client:
¤ Return to driving, with or without
adaptive driving equipment.
¤ Limit driving with restrictions
placed on either the geographic
areas or conditions in which the
client drives.
¤ Attend a remedial driving course to
establish/maintain defensive driv-
ing skills.
¤ Receive adaptive driving instruc-
tion or driver retraining using a
vehicle matched to the client’s
individual needs.
¤ Stop driving. This is advised when
a client does not demonstrate the
necessary skills to resume driving,
43Chapter 5—The Driver Rehabilitation Specialist
• How many years of experience does
the DRS (or program) have? In many
cases, experience may be a more
important indicator of quality than
certication alone—there are many
well-qualied DRSs who are not
certied.
• Does the DRS provide both the
clinical assessment and on-road as-
sessment? A DRS who provides both
components of the evaluation (or a
program whose specialists perform
both components as a team) is ideal.
Referral to two separate specialists
or centers is inconvenient for the
physician and the patient, and often
presents a greater insurance reim-
bursement challenge. In addition,
some programs utilize a driving simu-
lator program, which has strengths of
reliability, but weaknesses of validity,
lack of standardization, paucity of
evidence that correlates it with other
important outcomes, and possibly
sickness induced by the simulator.
• Does the DRS provide rehabilitation
and training? A good DRS (or pro-
gram) should be experienced in both
assessment and rehabilitation, and
should be able to prescribe adaptive
devices or vehicle modications and
train the patient in their use.
• How much can the patient expect to
pay out-of-pocket for assessment, re-
habilitation and adaptive equipment?
• Who will receive a report of the
assessment outcome? In most cases,
reports are sent to the patient and to
the physician and/or referring agency
(e.g., workers compensation or ofce
of retirement services) Some DRSs
also send reports to family members,
at the request of the family and with
the client’s consent. Whether or not
the DRS reports to the State DMV
is highly variable: In States with
mandatory reporting laws, the DRS
and/or physician may send a report; if
reporting is not legally required, some
DRSs will still send a report in the
interest of public safety. The policy of
the DRS should be discussed with all
parties prior to the evaluation.
• If the patient receives recommenda-
tions to cease driving, does the DRS
procedures (e.g., patient pays up-front
and is reimbursed when insurance pay-
ments are received, or payment is col-
lected directly from insurance provider).
Where can I find a driver
rehabilitation specialist?
Driver rehabilitation programs and
DRSs are still fairly rare, but in private
practice they are often afliated with
hospitals, rehabilitation centers, driving
schools, and State departments of mo-
tor vehicles. DRS services may also be
found through area agencies on aging,
universities, and area departments of
education. Before referring patients to
driving schools for driver assessment
and rehabilitation, physicians are urged
to determine that the staff has training
and experience in driver rehabilitation.
A background in driver education
alone may be insufcient for appropriate
assessment of medically impaired drivers
and correct interpretation of
the assessment.
To locate a DRS in your area, you
may wish to start by calling the occupa-
tional therapy departments in your
local hospitals or rehabilitation centers.
The ADED’s online directory is another
good source of information. The direc-
tory, which can be found by clicking the
Directory button at www.driver-ed.org or
www.ADED.net, lists all 553 ADED
members (as of December 2006),
including 251 certied DRSs. You can
search the directory by State, county,
type of facility, program services offered,
and professional background of the
DRS, as well as by name of the DRS
or name of the driver rehabilitation
program. Please note that not all ADED
members provide direct assessment
and rehabilitation services; some are
involved solely in vehicle modication,
as indicated in their “program services”
eld. Many local chapters of the
Alzheimer’s Association (www.alz.org)
also provide lists of area driving
evaluation programs.
When selecting a DRS or driver
rehabilitation program, the patient
and family may want to ask:
What is the cost of driver
assessment and rehabilitation?
While the cost of driver assessment and
rehabilitation varies between programs
and according to the extent of services
provided, the range is typically $300
to $400+ (as of this printing) for a
full assessment and $100 an hour for
rehabilitation. If adaptive equipment
is required, the cost is approximately
$70 to $100 for a spinner knob, $400 to
$500 for a left foot accelerator, $700 to
$900 for hand controls, and thousands
of dollars for reduced-effort steering sys-
tems, wheelchair lifts, and raised roofs
and dropped oors on vans.
Two programs that may pay for driver
assessments, driver rehabilitation, and
vehicle modications are each State’s
workers compensation and vocational
rehabilitation programs. However,
not all drivers—and often many older
drivers—will not qualify for either
program, and insurance coverage from
Medicare, Medicaid, and private insur-
ance companies is variable. To date,
these expenses are usually out of pocket.
In general, Medicare does not reimburse
for driving services, and private insur-
ance companies—basing their coverage
on Medicare’s covered services—tend
to follow suit. However, some driver
rehabilitation programs have success-
fully pursued insurance reimbursement
from Medicare and other providers.
(Note that while Medicare may provide
partial or full reimbursement for driver
assessment and rehabilitation, it does
not cover the cost of adaptive equip-
ment.) At present, the American
Occupational Therapy Association
(AOTA) is actively lobbying for consis-
tent Medicare coverage of occupational
therapy-performed driver assessment
and rehabilitation, with the assertions
that these services fall under the scope
of occupational therapy practice and
that driving is considered an instrumen-
tal activity of daily living.
Because rates and extent of insurance
reimbursement vary among driver
rehabilitation programs, patients should
be encouraged to inquire about program
rates, insurance coverage, and payment
44 Chapter 5—The Driver Rehabilitation Specialist
Remind your patient to schedule a
follow-up appointment with you after
he/she undergoes evaluation. If your
patient is safe to drive (with or without
restrictions, adaptive devices, and/or
rehabilitation), reinforce any recom-
mendations made by the DRS. When
applicable, family and caregivers should
be informed of these recommendations.
Also remember to counsel your patient
on the Successful Aging Tips and Safe
Driving Tips handouts, and encourage
him/her to start planning alternative
forms of transportation in case they
ever become necessary. If your patient
is not safe to drive, then you will
need to counsel him/her on driving
cessation. This is discussed in the
following chapter.
Special mention is made of other reha-
bilitation specialists who may be helpful
for impairments that are not uncommon
in older adults. For instance, physical
therapists may be able to improve muscle
weakness, range of motion or physi-
cal frailty. Visual rehabilitation may be
available in some specialized centers.
Neurophthalmologists or optometrists
may provide vision training, especially
for patients with neurological insults that
affect convergence, alignment, nystagmus,
eye apraxia, and/or visual neglect from
stroke, head injury, brain tumors,
and trauma.
What if driver assessment is
not an option?
Unfortunately, driver assessment and
rehabilitation may not always be feasible
options for your patients. In some areas,
DRSs simply are not available. Even if
a DRS is available, your patient may
refuse further assessment, or may
be unable to afford it.
• If driver assessment through a driver
rehabilitation specialist is not an
option, you have several choices:
• Some occupational therapists are
“generalists” and still may be able to
perform off-road tests and/or mobility
counseling. Referral to these types
of health professionals may actually
be a more common option in your
community.
send you to someone who can assist us with
your driving abilities. Consider this a kind
of ‘driving check-up,’ to be sure you are t
to drive.
“This person, who’s called a driver
rehabilitation specialist, will ask you some
questions about your medical history and
test your vision, strength, range of motion,
and thinking skills—similar to what we did
the last time you were here. He/she will
also take you out on the road and watch
your driving, and might recommend some
accessories or modications for your car,
such as extra mirrors, and show you how
to use them.
“The cost of these assessments ranges any-
where from $300 to $400, and there may
be additional costs for accessories or reha-
bilitation training. However, it is possible
insurance may pay for part of the assess-
ment and training. I know this sounds like
a lot of money, but I think this is important
for your safety. If you were to ever get into
a serious car crash, your medical bills or
the costs for someone you injured could end
up costing you more money. We should try
to prevent that from happening.”
Most programs will require a written
physician prescription. When writing
the driving evaluation prescription, try
to list a specic cause for assessment
and rehabilitation. Assessment that is
ordered the patient is “an older adult,”
“debilitated,” or “frail” does not provide
adequate guidance to the DRS and can
complicate insurance reimbursement.
On the other hand, “OT driver evalu-
ation for hand weakness such as poor
nger exion or limited neck rotation
secondary to arthritis,” “DRS evaluation
for hemianopia secondary to stroke,”
and “DRS evaluation for cognitive
impairments secondary to Alzheimer’s
disease” provide more guidance for
the DRS and are more likely to be
reimbursed by insurance. In addition,
most DRS programs will send the
physician a referral form that includes
space for a list of current diagnoses
and medications.
provide any counseling or aid in iden-
tifying alternative forms of transpor-
tation? Please note that DRS counsel-
ing does not preclude the need for
physician follow-up. Many times, the
patient may be too distressed at the
time of DRS counseling to absorb
information. Mobility counseling is
crucial for reinforcement of this in-
formation, and it demonstrates to the
patient the physician’s involvement
and support.
CarFit is an educational program created
by the American Society on Aging and
developed in collaboration with AAA
(American Automobile Association),
AARP, and the American Occupational
Therapy Association. CarFit offers older
adults the opportunity to check out how
well their personal vehicles “t” them.
An evaluation, typically performed by
an occupational therapist or a trained
volunteer, employs a checklist for correct
positioning of the seat, use of mirrors,
and so forth. Information and materials
for community-specic resources and ac-
tivities that could make drivers personal
vehicles t better, enhance their safety as
drivers, or increase their mobility in the
community are available. More informa-
tion on referring your patients to this
service can be found at www.car-t.org.
Making the referral
Prior to making the referral, let your pa-
tient know why he/she is being referred,
what the assessment and rehabilitation
will accomplish, what these will consist
of, and how much he/she can expect to
pay out-of-pocket for these services.
For example, you could tell
Mr. Phillips:
“Mr. Phillips, I’m pleased that you can see
better with your new glasses, and that your
physical tness has improved with your
walking. I’d like you to keep up the good
work. However, I’m still concerned about
your hands and your neck. I’m concerned
about your poor grip on the steering wheel,
and I’m worried that you can’t see around
you well enough to drive safely. I’d like to
45Chapter 5—The Driver Rehabilitation Specialist
• If there are changes in driving behav-
ior that you feel are likely to improve
your patient’s driving safety (e.g.,
avoiding driving at night, rush hour,
adverse weather conditions, etc.),
make these recommendations to your
patient and follow up for compliance.
• Private driving schools and driving
education programs may be available
in your area; however, they may not
have expertise in assessing older
adults with medical impairments.
• If you are urgently concerned about
your patient’s driving safety, you may
wish to refer your patient to your
state DMV for a driving assessment.
Depending on your state’s reporting
laws, you may be legally responsible
for reporting “unsafe” drivers to the
DMV. (A detailed discussion of the
physician’s legal and ethical respon-
sibilities can be found in Chapter 7;
a reference list of reporting laws is in
Chapter 8.) The patient should be
• Driving educational specialists are
often based at high schools or afli-
ated with programs for novice drivers.
Yet, some of these specialists have
developed experience in assessing
and counseling medically impaired
drivers and may be a resource in your
community.
• Advise your patient to continue,
restrict, or cease driving based on
the medical history, the results of
ADReS, and your clinical judgment.
As always, document your recommen-
dation in the patient’s chart. Some
physicians have the patient sign a
document for the le acknowledging
the doctor’s recommendation to
cease driving.
• You might consider the evaluation
of another health professional
such as a geriatrician, neurologist,
psychiatrist, or neuropsychologist
for a patient who has a chronic
disease such as Alzheimer’s.
referred with his/her knowledge, and
this should be documented in the
chart. Many States will require the
physician to ll out forms that require
medical information and vision test-
ing results, and provide an opinion
on whether the driver should undergo
visual and/or on-the-road testing.
• If there are no medical contraindica-
tions to continued driving, remember
to counsel your patient on Successful
Aging Tips and Safe Driving Tips and
encourage him/her to start planning
alternative forms of transportation.
46 Chapter 5—The Driver Rehabilitation Specialist

CHAPTER 6
Counseling the Patient
Who is no Longer Safe
to Drive

49
For various reasons, physicians may be
reluctant to discuss driving cessation
with their patients. Physicians may fear
delivering bad news or be concerned
that the patient will lose mobility and
all its benets. Physicians may avoid
discussions of driving altogether because
they believe that a patient will not
heed their advice or become angry. The
physician may also be concerned about
losing a patient to another practice.
These concerns are all valid. However,
physicians have an ethical responsi-
bility to protect their patients’ safety
through assessment of driving-related
functions, exploration of medical and
rehabilitation options to improve their
patients’ driving safety, and—when all
other options have been exhausted—
recommendations for driving restriction
or driving cessation. Physicians are
inuential in a patient’s decision to stop
driving; in fact, advice from a doctor is
the most frequently cited reason that a
patient stops driving.
118
In this chapter, we discuss the key
points to address when counseling a
patient to stop driving and provide
strategies for managing challenging
cases. When counseling a patient to
stop driving, the following steps may
be useful:
118. Persson, D. (1993). The elderly driver: deciding
when to stop. Gerontologist. 33:88–91.
and the senior citizen shuttle in his
community will be adequate for his
transportation needs, and he plans
to give his car to his granddaughter.
Your next patient is Mrs. Allen an
82-year-old woman who is ac-
companied by her daughter. The
daughter reports that her mother,
who lives alone, has become increas-
ing forgetful, repeats herself within
minutes, and has difculty dressing
herself, performing personal hygiene
tasks, and completing household
chores. She is particularly concerned
about her mother’s daily trips to
the grocery store two miles away.
Mrs. Allen has become lost while
on these trips and—according to the
store manager—has handled money
incorrectly. Dents and scratches
have appeared on the car without
explanation. Mrs. Allen’s daughter
has asked her mother to stop driving
and tried to take the car keys, but
Mrs. Allen responds with anger and
resistance each time. The daughter
would like to know how to manage
her mother’s long-term safety and
health, and would especially like to
know how to address the driving
issue. What do you tell her?
For most of us, driving is a symbol of
independence and a source of self-es-
teem. When an individual retires from
driving, he/she not only loses a form of
transportation, but all the emotional
and social benets derived from driving.
Mr. Phillips returns for follow-up
after undergoing driver assessment.
From the driver rehabilitation spe-
cialist (DRS) report, you know that
the DRS recommends that Mr. Phil-
lips resume driving after his car has
been tted with wide-angle rear-view
mirrors. At the visit, Mr. Phillips
states that he is driving more com-
fortably with this adaptive device.
You counsel him on the Tips for Safe
Driving and Successful Aging Tips,
advise him to continue walking, and
encourage him to start planning
alternate transportation options. His
daughter is recruited to assist with
these discussions and interventions.
You continue to provide care for Mr.
Phillips’ chronic conditions and fol-
low up on his driving safety. Three
years later, Mr. Phillips’ has a right
middle cerebral artery stroke and
decits of left-sided weakness and
hemispatial inattention. His health
has declined to the extent that you
believe it is no longer safe for him
to drive. You also feel that due to
the xed nature of his decits (more
than six months since the event)
driver rehabilitation is unlikely to
improve his driving safety. Mr. Phil-
lips has decreased his driving over
the years, and you now tell him that
it is time to stop driving completely.
Mr. Phillips replies, “We’ve talked
about this before, and I gured it
was coming sooner or later.” He feels
that rides from family and friends
CHAPTER 6
Counseling the Patient
Who is no Longer Safe
to Drive
50 Chapter 6—Counseling the Patient Who is no Longer Safe to Drive
long explanations. Rather, you should
focus on making certain your patient
understands your recommendation and
understands that this recommenda-
tion was made for his/her safety. If the
patient is competent but will allow the
presence of a spouse or family member,
having this person present may be help-
ful when communicating this sensitive
information. All discussions should be
documented in the chart.
Discuss transportation
options.
Once you have recommended that
your patient stop driving, you need to
explore possible transportation alterna-
tives. Unfortunately, driving cessation
has been associated with a decrease
in social integration.
119
Discuss with
your patient the fact that there may be
alternative ways to reach destinations.
Encourage your patient to take control
of his/her future by creating a transpor-
tation plan. (Please note: If your patient
does not have the cognitive capabili-
ties for these tasks, see the section on
patients who lack decision-making
capacity later in this chapter.)
Give your patient resources to explore
options (see Appendix B handout
sheets). By providing this information,
you empower your patient to formu-
late a personal plan for transportation.
Special mention is made of The Hart-
ford insurance company’s educational
brochures “We Need to Talk” and “At
the Crossroads.” These guides provide
excellent worksheets for dening perti-
nent out-of-home activities, initiating
discussions between patients and their
families, and assisting the patient and
the family member on deciding how
specic trips will be accomplished.
120
This process will help your patient pre-
serve a sense of self-determination and
119. Mezuk, B., & Rebok, G. W. (2008). Social
integration and social support among older
adults following driving cessation. J Gerontol
Series B Psychol Sci Social Sci. 63:S298-303.
120. The Hartford. (2007). Alzheimer’s, Dementia
& Driving. Hartford, CT. www.thehartford.com/
alzheimers/brochure.html. Accessed October 24,
2007.
Explain to your patient
why it is important to
stop driving.
If your patient has undergone the
ADReS battery (see chapters 3 and 4)
or assessment by a driver rehabilitation
specialist, explain the results of the
assessment in simple language. Clearly
explain what the results tell you about
his/her level of function, and then
explain why this function is important
for driving. State the potential risks of
driving, and end with the recommen-
dation that your patient stop driving.
This might be a good time to discuss the
patient’s thoughts or feelings, especially
if he/she did cause a crash. If the patient
should not drive, you might discuss is-
sues related to injury, public safety, and/
or liability. This discussion should be
put in writing and if the patient lacks
decision-making capacity, involve a
family member or caregiver.
For example, you could say to
Mr. Phillips:
“Mr. Phillips, the results of your eye exam
show that your vision isn’t as good as it
used to be. Good vision is important for
driving, because you need to be able to
see the road, other cars, pedestrians, and
trafc signs. With your impaired vision
due to underlying eye disease and now a
stroke, I’m concerned that you’ll get into a
car crash. Since your vision cannot be cor-
rected to a level safe for driving, for your
own safety and the safety of others, it’s
time for you to retire from driving. In addi-
tion, there are legal requirements for vision
and you do not meet those any longer. “
Your patient may become upset or angry
at your recommendation to stop driv-
ing. Acknowledge your patient’s feelings
and be empathetic to any emotional
responses. While you should be sensi-
tive to the practical and emotional
implications of driving cessation, it
is also necessary to be rm with your
recommendation. At this time, it is
best to avoid engaging in disputes or
Figure 1
Transportation alternatives
• Walking
• Train/subway
• Bus
• Taxi
• Friends/family
• Paratransit
• Community transportation services
• Hospital shuttles
• Medi-car
• Delivery services
• Volunteer drivers (church, synagogue,
community centers)
• Private for-profit elderly care services

51Chapter 6—Counseling the Patient Who is no Longer Safe to Drive
independence. While older adult non-
drivers usually prefer rides from friends
and family, they are often uncomfort-
able with the accompanying feelings
of dependency.
121
Using alternative
transportation options such as buses,
trains, cabs, or even walking, offers pa-
tients independence from having to rely
on others. However, these may not be
a reasonable alternative for those with
physical frailty and/or dementia.
To begin a discussion on driving alter-
natives, ask if your patient has made
plans to stop driving or how he/she cur-
rently nds rides when driving is not an
option. Offer alternative transportation
methods for your patient to use (Figure
6.1). Explore any barriers your patient
foresees to these methods (i.e., nancial
constraints, limited service and destina-
tions, and required physical skills for
accessibility).
Help your patient identify his/her
most feasible transportation options, as
there often are necessary cognitive and
physical skills required to access certain
transportation alternatives. Stress the
importance of planning ahead for social
activities—which contribute to quality
of life. Your patients can contact their
Area Agency on Aging and/or Alzheim-
er’s Association for information on local
resources such as taxis, public trans-
portation services, and senior-specic
transportation services. To nd contact
information for your local area, call the
nationwide Eldercare Locator at
800-677-1116. This might be a good
time to refer to a social worker or a
gerontological care manager who may
be aware of alternate modes of transpor-
tation and/or can deal with the patient’s
feelings of social isolation or depression.
The Federal Government has rec-
ognized the limited transportation
alternatives that are currently available
(especially in rural areas) for an aging
country with an increasing number of
older adults who will no longer be able
121. Coughlin, J. (2001). Transportation and the
Older Persons: Perceptions and Preferences.
AARP Public Policy Institute Issue Paper.
Figure 6.2
Encourage family/caregiver
assistance
• Encourage family to promote the
health and safety of their loved one
by endorsing your recommendation
and assisting in securing needed
transportation.
• Include them in the mobility
counseling process.
• Provide resources to caregivers.
• Give copies of the How to Assist the
Older Driver resource sheet (see
Appendix B).
• Refer caregivers to the National
Family Caregivers Association (NCFA)
at 800-896-3650 or www.nfcacares.
org to find resources and tips on
caring for loved ones.
• Look for signs of caregiver burnout.
• Keep the communication door open
to the family.
• In the case of cognitive impairment
where it is believed the patient does
not have decision-making capacity
(e.g., lack of insight), communication
with a family member to reinforce
recommendations is imperative.
• Recognize that if the caregiver has
depended on the patient for trans-
portation, the situation may require
more time, counseling, and support
to meet the needs of the family.
to operate an automobile. To that end,
legislation has been enacted to sup-
port funding of novel programs to assist
seniors with transportation to needed
destinations. To nd more information
on transportation options, please go
to www.unitedweride.com.
Encourage your patient to involve fam-
ily members in creating a transportation
plan. Obtain your patient’s permission
when involving family or caregivers,
and encourage them to offer rides and
formulate a weekly schedule for running
errands. They can also help arrange for
delivery of prescriptions, newspapers,
groceries and other services (See Figure
6.2 for more tips). However, do not
ignore your patient while including the
caregiver in the discussion.
Reinforce driving cessation.
The message to cease driving is essen-
tial to ensure your patient’s safety, yet
also presents a signicant demand on
your patient to change his/her current
behavior. Therefore, you will need to
ensure that your patient understands
the reasons (legal, health and safety)
why you have recommended driving
discontinuation. Your patient may be-
come argumentative or emotional dur-
ing the ofce visit. He/she may not fully
comprehend your recommendations and
may not remember all the information
you provide. To help re-enforce your
message:
• Ask your patient if he/she has any
questions regarding the assessment
and your recommendation. Reassure
your patient that you are available
should he/she have questions or need
further assistance.
• Ask your patient to reiterate to you,
why he/she must not drive. Stress this
recommendation is for personal safety
and the safety of others on the road.
• Your patient may benet from the
visual reinforcement of a prescrip-
tion with the words “Do Not Drive.”
Ensure that your patient understands
why he/she is receiving this prescrip-
tion, so as to avoid feelings of anxiety
or anger. See Figure 3 for further re-

52
able to plan for and schedule transpor-
tation to and from necessary appoint-
ments. Ensure that your patient has
secured reliable and sufcient transpor-
tation resources to meet his/her needs.
Consider referral to a social worker or
gerontological care manager.
As an example of a follow-up conversa-
tion with Mr. Phillips in your ofce, you
could state the following;
Physician: Here is a prescription for your
medicines, you’ll need to rell this at your
pharmacy after our appointment … now
how did you get here to the ofce today?
Mr. Phillips: Oh, my son dropped
me off.
Physician: I see, has he been driving
you lately?
Mr. Phillips: Yes, ever since I stopped
driving, he and his wife have been taking
me where I need to go. He is going to pick
me up in 15 minutes.
Physician: How has that been working
for you?
Mr. Phillips: This has worked quite well.
Physician: Will he be able to take you to
the pharmacy?
Mr. Phillips: Yes, that will not be a
problem.
Physician: It’s wonderful that you have
found them to be a reliable source for rides.
What do you do when one of them is
unable to drive you where you need to go?
Be alert to signs of depression, neglect,
and social isolation (see Figures 6.4
122
and 6.5 for details). Older adult who
stop driving are at increased risk for
122. APA. (2000). Diagnostic and Statistical Manual
of Mental Disorders, Fourth Edition, Text Revi-
sion. Washington, DC: American Psychiatric
Association.
enforcement tips.
• Send your patient a follow-up letter
(see Figure 6.6). Place a copy of this
letter in the patient’s chart as docu-
mentation and another visual tool for
re-enforcement. The letter should be
written in simple language to ensure
your patient understands your recom-
mendation. You can use the sample
letter in Figure 6.6 as a template.
• Discuss State reporting requirements
with your patient (see Chapter 7 and
Chapter 8 for more details). In the
case of mandatory reporting laws,
inform your patient that you are
required by law to inform your local
DMV of medical conditions that
could affect a patient’s safe operation
of a vehicle. Let your patient know
the DMV will follow up, and what to
expect as part of this evaluation (i.e.,
review of driving record, required
road test). In States with voluntary
laws, a referral to the DMV could still
be appropriate and patients may need
to hear they will be reported if they
drive against medical advice.
• Help facilitate family members’ assis-
tance in encouraging driving cessa-
tion, and if necessary, encourage your
patient to self-report his/her impair-
ment to the DMV. It may be helpful
to enlist other trusted allies, such as
clergy, friends, or the family attorney.
• Ask your patient to return to you in
one month for a follow-up assess-
ment. (See next section for details of
this visit.)
Follow-up with your patient.
At your patient’s follow-up appoint-
ment, you will want to assess:
• Your patient’s ability to comply with
the stop driving recommendation.
• Transportation resources your patient
has identied and has or has not uti-
lized, looking especially at viability.
• Signs of isolation or depression.
Start the assessment by asking the
patient how he/she got to the appoint-
ment that day. This will help you de-
termine whether your patient has been
Figure 6.3
Tips to reinforce driving cessation
Tip 1: Give the patient a prescription
on which you have written “Do Not
Drive, For Your Safety and the Safety
of Others.” This acts as a reminder for
your patient and also emphasizes the
strength of your message.
Tip 2: Remind your patient this recom-
mendation is for his/her safety and for
the safety of other road users.
Tip 3: Ask the patient how he/she
might feel if they were to get in a crash
and injure themselves or someone else.
Tip 4: Use economic arguments. Point
out rising gas and oil prices, expense
of car maintenance (tires, tune-ups,
insurance), registration/license fees,
financing expenses and depreciation
of car value. Web sites are available
to demonstrate the financial burden of
owning and operating a car, and it may
be useful to perform this exercise with
the older adult.
1
Also, some physicians
will state that the patient’s life savings
may be at stake if they drive against
medical advice and injure someone.
Tip 5: Have a plan in place that involves
family member support for alternative
transportation.
1. The Real Cost of Car Ownership Calculator.
(2007). Bikes at Work Inc. www.bikesatwork.
com/carfree/cost-of-car-ownership.html.
Accessed December 13, 2007.
Chapter 6—Counseling the Patient Who is no Longer Safe to Drive

53
Physician: Mr. Adams, when do you
think it’s an appropriate time for a person
to stop driving?
Mr. Adams: I suppose when they
drive unsafely or are a threat to others
on the road.
Physician: That is an excellent
observation; and I would agree with you.
Mr. Adams: Well, a friend of mine
doesn’t drive very well. He drives all over
the road and runs red lights. I won’t get in
the car with him anymore because I worry
about what may happen.
Physician: That can be a scary situation
for your friend and others on the road as
well. It’s great that you are aware of the
potential danger and that you know how to
ensure your own safety. I am wondering,
is there someone whom you trust, and who
would tell you when they thought it was
unsafe for you to continue driving?
Many older drivers are able to iden-
tify peers whose driving they consider
unsafe, yet may not have the insight
to recognize their own unsafe driving
habits. Ask your patients if they have
friends with whom they are afraid to
drive and why. It’s important to have
your patients begin to think about what
they can expect when their driving abil-
ities begin to decline. Let your patients
know they are not alone and that many
people make the decision to restrict
or cease driving when safety becomes
a concern. Encourage your patients to
obtain a second opinion if they feel ad-
ditional consultation is necessary.
• Have your patient identify support
systems. Ask your patient to list fam-
ily members, church groups, neigh-
bors, etc. who are able and willing to
help with transportation decisions.
This will help your patient become
aware of a supportive network and
feel more at ease when searching for
alternative transportation.
Situation #1:
The resistant patient.
If your patient is belligerent or refuses to
stop driving, it is important for you to
understand why. Knowing this will help
you address your patient’s concerns.
Listen to your patient. Use supportive
statements when addressing your pa-
tient’s concerns. Let your patient know
you are there as an advocate for his/her
health and safety.
Physician: Mr. Adams, I understand you
drove yourself to the appointment today.
This worries me. At our last visit, I recom-
mended that you retire from driving. I am
wondering why you chose to drive yourself
here today?
Mr. Adams: Well, doctor, I don’t under-
stand it. I’ve never gotten into an accident.
My driving is ne and frankly, I don’t think
you have any right to tell me not to drive.
Physician: It sounds like you are frus-
trated and I can’t imagine how difcult it
must be for you to adjust to a life without
driving. It’s not an easy choice to make;
however, it’s the best choice for your health
and safety, and as your physician, that is
my primary concern. I want to help make
this easier for you. Let’s talk about some
of your concerns regarding retiring from
driving.
Remember driving cessation can have
severe emotional and practical implica-
tions for your patients, and they may
have a difcult time adjusting.
• Have the patient dene when a
person would be unt to drive. This
will better help your patient recognize
impairment in his/her own driving
capabilities and will help you assess
your patient’s judgment and insight.
In addition, it might open up discus-
sion where you can each reach some
common ground.
decreasing out-of-home activities.
123
Driving cessation has also been as-
sociated with an increase in depres-
sive symptoms in the elderly
124
125
in
addition to an increased risk of nursing
home placement.
126
Because depres-
sive symptoms have also been linked to
physical decline and mortality in the
elderly,
127
it is important to continue
to monitor your patient for any signs of
decompensation. Ask your patient how
he/she is managing without driving.
Educate family members and caregivers
on signs of depression and inquire about
any concerns they may have.
Continue to assess and treat your
patient’s functional or cognitive impair-
ments. If they improve to the extent
that the patient is safe to drive again,
notify the patient and give him/her the
resource sheet on Tips for Safe Driving
(see Appendix B).
Situations that require
additional counseling.
It may be necessary to provide addi-
tional counseling to encourage driv-
ing retirement or to help your patient
cope with this loss. Below, we provide
potential situations (e.g., new patient
scenarios) that may arise with patients
who have difculty coping or adhering
to the recommendation to stop driving.
123. Marottoli, R. A., de Leon, C. F. M., Glass, T. A.,
et al. (2000). Consequences of driving cessation:
decreased out-of-home activity levels. J Gerontol
B Psychol Sci Soc Sci. 55:S334–340.
124. Marrottoli, R. A., Mendes de Leon, C., Glass, T.
A., Williams, C. S., Cooney, L. M., Berkman, L.
F., et al. (1997). Driving cessation and increased
depressive symptoms: prospective evidence
from the New Haven EPESE. J Am Geriatr Soc.
45:202–210.
125. Fonda S. J., Wallace R. B., Herzog A. R. (2001).
Changes in driving patterns and worsening
depressive symptoms among older adults.
J Gerontol. 56(6):S343–351.
126. Freeman E. E., Gange S. J., Munoz B., Wet
S. K. (2006). Driving status and risk of entry
into long-term care in older adults. Am J Public
Health. 96:1254–1259.
127. Berkman L. F., Berkamn C. S., Kasl S., et al.
(1986). Depressive symptoms in relation to
physical health and functioning in the elderly.
Am J Epidemiol. 124:372–388.
Chapter 6—Counseling the Patient Who is no Longer Safe to Drive
54
Situation #2: Your patient presents
with symptoms of depression.
This results from a combination of
factors such as diminished health,
social isolation, or feelings of loss.
If you suspect your patient may be
depressed (see Figure 6.4
128
), conduct a
full assessment to determine the most
appropriate treatment. Talk with your
patient and appropriate family members
about symptoms of depression and avail-
able treatment options. Consider refer-
ring your patient to individual therapy
or group therapy, and social/recreational
activities. Also consider treatment with
medications if appropriate, or referral to
a mental health professional. Normalize
this experience for your patient—
acknowledge they have suffered a loss—
and recognize this may be an especially
difcult time for them.
Situation #3: Your patient lacks
decision-making
capacity.
When your patient presents with sig-
nicant cognitive impairment, or lacks
insight or decision-making capacity
as in certain cases of dementia, it is
imperative that you employ the help of
the appointed guardian, caregiver, or
surrogate decision-maker to encourage
your patient to stop driving. Let family
and caregivers know they play a crucial
role in helping the patient nd alterna-
tives to driving. Inform the family that
you will be available to support and
assist in any way you can. In rare in-
stances, it may be necessary to appoint
a legal guardian for the patient. In turn,
the guardian may forfeit the patient’s
car and license on behalf of the safety of
the patient. These actions should only
be used as a last resort. From a practical
standpoint, hiding, donating, disman-
tling, or selling the car may also be
useful in these difcult situations.
128. APA. (2000). Diagnostic and Statistical
Manual of Mental Disorders, Fourth Edition,
Text Revision. Washington, DC: American
Psychiatric Association.
• Help your patient view the positives
of this decision—an opportunity to
assert control over a limitation. Of-
ten, discussion of relinquishing driv-
ing privileges tends to focus on the
negative aspects of driving cessation;
i.e., “losing independence” or “giving
up freedom.” Help your patients view
this as a step in health promotion
and safety for themselves and others.
Use phrases such as “it’s time to retire
from driving” and point out that he/
she may still request rides from family
and utilize community services, and
will have lower costs and responsibil-
ity for maintaining an automobile.
• Refer patient to social worker. Your
patient may need additional help in
securing resources and transitioning
to a life without driving. Social work-
ers can provide supportive counseling
to patients and families, assess your
patient’s psychosocial needs, assist in
locating and coordinating commu-
nity services and transportation, and
enable your patient to maintain inde-
pendence and safety, while preserving
quality of life. The National Associa-
tion of Social Workers Register of
Clinical Social Workers is a valuable
resource for nding social workers
in your area who have met national
veried professional standards for
education, experience and supervi-
sion. Order information or access the
on-line Register at www.socialwork-
ers.org (see Appendix B for more
details)Another resource for social
workers may be your local hospital
and a referral source may be the Area
Agency on Aging or the Alzheimer’s
Association.
Figure 6.4
Questions to assess for major
depression (adapted from the DSM-
IV-TR)
1
• Has your mood been down lately
on a consistent basis?
• Have you lost interest or pleasure in
all or most activities?
• Have you noticed any changes in
appetite or weight?
• Have you noticed any changes in
sleeping habits or in concentration?
• Have you noticed feelings of
worthlessness or recurrent
thoughts of death?
Figure 6.5
Signs of neglect or self-neglect
The patient has:
• An injury that has not been properly
treated
• Symptoms of dehydration and/or
malnourishment
• Weight loss
• Soiled clothing
• Recurrent falls with or without injuries
• Evidence of inadequate or inappropri-
ate administration of medications
• Spoiled or outdated food in the
refrigerator
• Loss of income from difficulty with
finances
1. 146 American Psychiatric Association (APA)
2000. Diagnostic and Statistical Manual IV-R.
(Fourth Edition-Text Revision). Washington:
American Psychiatric Association.
Chapter 6—Counseling the Patient Who is no Longer Safe to Drive
55
Situation #4: Your patient shows signs
of self-neglect or neglect.
Your patient may be unable to secure
resources for him/herself and may be
isolated, lacking sufcient support
from family, friends or an appointed
caregiver. If your patient does not have
the capacity to care for him/herself, or
family and caregivers lack the ability
to adequately care for your patient, be
alert for signs of neglect or self-neglect
(see Figure 6.5). If you suspect neglect
or self-neglect, involve adult protective
services (APS). Neglect is the failure of
a caregiver to fulll his/her caregiving
responsibilities, whether due to will-
ful neglect or an inability as a result of
disability, stress, ignorance, lack of ma-
turity, or lack of resources. Self-neglect
is the failure to provide for one’s own
essential needs. APS will investigate
for neglect, self-neglect or abuse of the
elderly person. APS can secure services
such as case planning, monitoring, and
evaluation; and can arrange for medical,
social, economic, legal, housing, law
enforcement and other emergency or
supportive services. To obtain contact
information for your State ofce, call
the Eldercare Locator at 800-677-1116.
Chapter 6—Counseling the Patient Who is no Longer Safe to Drive

56
Figure 6.6
July 1, 2009
Clayton Phillips
123 Lincoln Lane
Sunnydale, XX 55555
Dear Mr. Phillips:
I am writing to follow-up on your clinic visit on June 20, 2009. As you recall, we talked about your safety when
you drive a car. I tested your vision (eyes), strength, movement, and thinking skills, and asked you about your
health problems and medicines. I recommended that you stop driving due to your slowed reaction time, poor vi-
sion and muscle weakness.
I know that driving is important to you, and I know that it is hard to give up driving, but your safety is more
important than driving. To help you get around, you can ask for rides from your son and your friends. You can
also use the special bus in your neighborhood. The hand out How to Assist the Older Driver (enclosed) has some
other ideas that we talked about. As we discussed, I am also sending a copy of these materials to your son and you
two can discuss this plan together.
I want to make sure you can still visit your friends, and go other places without a car. It is important for you to
maintain your connection with the community. Please see me again in one month—we will talk about how this
plan is working for you.
For a mandatory reporting State considering adding:
As we discussed, the State of _____ requires me to submit the names of potentially unsafe drivers. Because I am
required by law to do this, I have given your name to the ____ Department of Motor Vehicles (DMV). The DMV
will send you a letter in a few weeks to discuss your driver’s license.
For a voluntary reporting State consider adding:
It is very important that you do not drive since you are putting yourself and the public at risk. If you continue to
drive, I will need to report you to the Department of Motor Vehicles for an evaluation and possible revocation of
your license.
Please call my ofce if you have any questions. I look forward to seeing you next month.
Sincerely,
Your Physician
Enc: How to Assist the Older Drive
cc: Your son
Note the sample letter in Figure 6.6 has been written at a 5th grade reading level, as measured by the S.M.O.G. Readability Formula
Chapter 6—Counseling the Patient Who is no Longer Safe to Drive

CHAPTER 7
Ethical and Legal
Responsibilities of the
Physician

59
light duties of the physician that are
relevant to the issue of driving.
These include:
“ Duty to Protect”
The Patient
Protecting the patient’s physical and
mental health is considered the physician’s
primary responsibility. This includes not
only treatment and prevention of ill-
ness, but also caring about the patient’s
safety. With regard to driving, physi-
cians should advise and counsel their
patients about medical conditions and
possible medication side effects that
may impair one’s ability to drive safely.
Certain states have enacted mandatory
reporting requirements, which place the
physician in danger of both civil and
criminal liability for failure to report.
131
Wording in the Pennsylvania law has
led the Pennsylvania DMV to state that
physicians who do not report “could be
held responsible as a proximate cause of
an accident resulting in death, injury or
property loss caused by your patient; the
Pennsylvania statute further states that
131. OR. REV. STAT.§ 807.710 (2001)
Driving is a difcult topic to address,
particularly when there is the risk of
damaging the patient-physician rela-
tionship, violating patient condentiality,
and potentially losing patients. To
complicate matters, many physicians are
uncertain of their legal responsibility,
if any, to report unsafe drivers to their
state DMV.
129,130
As a result, physicians
are often faced with a dilemma: should
they report the unsafe driver to the
State DMV at the expense of breaching
condentiality and potentially damaging
the patient-physician relationship, or
should they forego reporting and risk
being liable for any potential patient or
third-party injuries for failing to report?
Furthermore, should they engage the
family in taking the responsibility for
driving restriction or cessation?
The Physician’s Ethical Duties
Current legal and ethical debates high-
129. Kelly, R., Warke, T., & Steele, I. (1999). Medical
restrictions to driving: the awareness of patients
and doctors. Postgrad Med J. 75:537–539.
130. Miller, D., Morley, J. (1993). Attitudes of
physicians toward elderly drivers and driving
policy. J Am Geriatr Soc. 40:722–724.
Upon further evaluation, you
diagnose Mrs. Allen (see Chapter
6) with Alzheimer’s disease. It is
readily apparent that her condition
has progressed to the extent that she
is no longer safe to drive and that
rehabilitation is not likely to improve
her driving safety. You tell Mrs.
Allen that she must stop driving
for the sake of her safety and the
safety of others on the road. You
also explain that the State physician
reporting law requires you to notify
the Department of Motor Vehicles
(DMV) of your diagnosis. Initially,
Mrs. Allen does not comprehend,
but when you specically tell her
that she can no longer drive herself
to the grocery store every day, she
becomes agitated and abusive,
screaming, “I hate you!” and “I’m
going to sue you!” Her daughter
understands your decision to report
Mrs. Allen to the DMV, but is now
concerned that she will encounter
legal problems if her mother attempts
to drive without a license. She asks
if it is absolutely necessary for you to
report her mother. What do you say?
This chapter is intended to provide a general overview of a
physician’s ethical and legal responsibilities as related to
reporting unsafe drivers to their State’s DMV. While some
sections of this chapter address issues that are inherently legal,
the chapter is not intended to provide legal advice. The views,
discussion, conclusions and legal analysis are those of the
authors and do not represent the opinions, policies or ofcial
positions of NHTSA. This chapter conveys the current
environment at the time of publication and compiles general
knowledge to assist physicians in understanding the reporting
process. Laws, regulations and policies vary not only by State
but also by local jurisdiction, and are subject to change. There-
fore, it is important for physicians to seek out legal advice
from a licensed attorney in their States on specic issues or
questions that may arise with an individual patient. The
cases cited in this chapter are provided as examples of the
range of opinions in attempting to fairly dene the scope of
the physician’s responsibility to report impaired drivers. The
cases additionally demonstrate society’s efforts to provide safe
environments for its citizens.
For your reference, we have compiled a State-by-State list
of reporting laws, licensing requirements, license renewal
information, and DMV contact information in Chapter 8.
Please note that information may have changed since the
publication of this guide. You are encouraged to contact
your State DMV for the most up-to-date information.
CHAPTER 7
Ethical and Legal
Responsibilities of
the Physician
60 Chapter 7—Ethical and Legal Responsibilities of the Physician
Portability and Accountability Act of
1996, or HIPAA.
139
Patient condenti-
ality is dened as the physician’s ethical
obligation to keep information about
the patient and his/her care unavailable
to those—including the patient’s family,
the patient’s attorney, and the government
—who do not have the authorization to
receive or review this information.
140,141
Patient condentiality is crucial within
the physician-patient relationship
because it encourages the free exchange
of information, allowing the patient to
describe symptoms for diagnosis and
treatment.
142
Without belief in the
patient condentiality of their care,
individuals may be less likely to seek
treatment, disclose information for
effective treatment, or trust the health
care professional.
143
The need for patient condentiality
cannot be considered absolute; a
patient is entitled to freely disclose his
or her symptoms and condition to his
or her physician in condence except
where the public interest or the private
interest of the patient so demands, and
thus a patient possesses a limited right
to patient condentiality in extra-
judicial disclosures subject to exceptions
prompted by the supervening interest of
society.
144
Thus, patient condentiality
does not necessarily protect the physi-
139. Health Insurance Portability and Accountability
Act of 1996 (HIPAA), Public Law 104-191.
45 C.F.R.§ 164.512(a)—Uses and Disclosures
Required by Law (2000). Federal Register / Vol.
65, No. 250 / Thursday, December 28, 2000 /
Rules and Regulations; page 82811. Available
at www.hhs.gov/ocr/privacy/hipaa/administrative/
privacyrule/prdecember2000all8parts.pdf
140. Justice J. Patient condentiality and pharmacy
practice. Consult Pharmacist. 1997:12(11).
Available at: www.ascp.com/public/pubs/tcp/1997/
nov/patient.html.
141. Tasman A, Kay J, Lieberman JA, Fletcher J
(eds). Psychiatry, 1st ed. Philadelphia: W.B.
Saunders Company; 1997: p. 1808.
142. Retchin SM, Anapolle J. An overview of the
older driver. Clin Geriatr Med. 1993;9(2):279-
296.
143. Ferguson v. City of Charleston, 532 US 67
(deliberating in a South Carolina court case
the benets and risks of physician disclosing
condential patient information when that
condential information may protect patients
and society from possible harm).
144. Tasman A, Kay J, Lieberman JA, & Fletcher
J (eds). (1997). Psychiatry, 1st ed. P. 1808.
Philadelphia: W. B. Saunders Company.
states, physicians have been found
liable for third-party injuries because
they failed to advise their patients
about medication side effects,
136
medical
conditions,
137
and medical devices
138
that may impair driving performance
thus causing harm to those other than
the patient.
Maintaining patient
confidentiality
Patient condentiality is the right of an
individual to have personal, identi-
able medical information kept private;
these protections are enumerated in the
federal statute, the Health Insurance
136. Gooden v. Tips, 651 SW 2d; 364. Kaiser v.
Suburban Transportation System, 65 Wn. 2d
461, 398 P.2d 14 (stating in this Washington
state case, that a physician could be held liable
due to the fact that a patient took medication
completely unaware that it would have any
adverse effect on him because the physician
failed to warn his patient, whom he knew to
be a bus driver, of the dangerous side effects of
drowsiness or lassitude that may be caused by
taking this particular medication).
137. Caldwell v. Hassan, 260 Kan. 769 (nding in a
Kansas court case that that the doctor had no
duty to protect bicyclists - a third party- from
his patient’s actions because the patient who
had a sleep disorder was aware of the problem
and admitted to knowing that she should have
stopped driving).
Duvall v. Goldin, 362 NW 2d 275 (nding
in a Michigan court case that the physician
was liable to third persons injured as it was
foreseeable that a doctor’s failure to diagnose or
properly treat an epileptic condition could have
created a risk of harm to a third party and that
as a result of the patient’s medical condition,
caused an automobile accident involving the
third persons).
Myers v. Quesenberry, 144 Cal App 3d 888,
(nding in a California court case that if a
physician knows or should know a patient’s
condition will impair the patient’s mental
faculties and motor coordination, a comparable
warning is appropriate).
Schuster v. Alternberg, 424 NW 2d 159 (nding
in a Wisconsin court case that if it was
ultimately proven that it could have been
foreseeable to a psychiatrist, exercising due care,
that by failing to warn a third person or failing
to take action to institute detention or commit-
ment proceedings someone would be harmed,
negligence could be established).
138. Joy v. Eastern Maine Medical Center, 529 A2d
1364 (nding in a Maine court case that when
the doctor knew, or reasonably should have
known that his patient’s ability to drive has been
affected by treatment that the doctor provided,
he had a duty to the driving public as well as to
the patient to warn his patient of that fact).
providers who do not comply with
their legal requirement to report may
be convicted of a summary criminal
offense”.
132
Some cases illustrate that a
physician’s failure to advise the patient
about such medical conditions and
medication side effects can be considered
negligent behavior.
133
The Public
In addition to caring for their patients’
health, physicians may, in certain
circumstances and jurisdictions, have
some responsibility for protecting the
safety of the public.
134,135
In certain
132. Title 75 PA. CODE § 1518(b) The Vehicle
Code (stating physicians are immune from
any civil or criminal liability if they do report
patients 15 years of age or older who have been
diagnosed as having a condition that could
impair his/her ability to safely operate a motor
vehicle; but, if the physician does not report
could, then, possibly be held responsible as a
proximate cause of an accident resulting in
death, injury, or property loss caused by the
physician’s patient. Also, physicians who do
not comply with their legal requirement to
report may be convicted of a summary criminal
offense). Available at www.dmv.state.pa.us/
pdotforms/fact_sheets/fs-pub7212.pdf
133. Gooden v. Tips, 651 SW 2d 364 (stating in a
Texas court case that physicians have a duty
to warn patients that medications may impair
driving but that physicians do not have a duty
to control a patient’s behavior).
Wilschinsky v. Medina, 108 NM 511 (stating in
a New Mexico court case the physician owed
a duty of care to an individual harmed by the
physician’s patient, that the patient’s doctor’s
duty specically extended to persons the patient
injured by driving a car from the doctor’s ofce
after being injected with drugs that were known
to affect judgment and driving ability; the
medical standards for administering drugs had to
dene the physician’s duties of care).
134. Tarasoff v. Regents of University of California, 13
Cal. 3d 177. It should be noted that the Tarasoff
ruling per se, upon which the principles of
‘Duty to Warn’ and ‘Duty to Protect’ are based,
originally applied only in the state of California
and now applies only in certain jurisdictions.
The U.S. Supreme Court has not heard a case
involving these principles. Many states have
adopted statutes to help clarify steps that are
considered reasonable when a physician is pre-
sented with someone making a threat of harm to
a third party. Tasman A, Kay J, Lieberman JA,
Fletcher J (eds). Psychiatry, 1st ed. Philadelphia:
W.B. Saunders Company; 1997: p. 1815
135. Brisbine, supra, 2002 PA Super 138, *; 799 A.2d
89 (dening factors applied in a Pennsylvania
court case in determining the existence of a
duty: (1) the relationship between the parties;
(2) the social utility of the actor’s conduct; (3)
the nature of the risk imposed and foreseeability
of the harm incurred; (4) the consequences of
imposing a duty upon the actor; (5) the overall
public interest in the proposed solution).
61Chapter 7—Ethical and Legal Responsibilities of the Physician
own state and/or have poor insight into
their own driving abilities,
153
or simply
cannot face voluntarily giving up their
freedom to drive. Although the au-
thors of this guide are not aware of any
supporting studies, there are concerns
about “doctor shopping,” failure to
disclose pertinent information in order
to secure more favorable opinions, or
approaching a new clinician who is un-
aware of the pertinent medical diagno-
ses. Physicians may be unaware of what
functional battery or tests to perform
to determine tness-to-drive.
154
Inter-
rater reliability has been reported to be
low when different physicians lled out
the same type of medical report on the
same patient.
155, 156
However, physicians
will continue to play an integral role
in these types of evaluations and will
require education in this area.
157
Thus, a
comprehensive approach such as iden-
tifying medical conditions or red ags,
and using the ADReS battery should
assist physicians in addressing some of
the concerns.
Physicians Concerns about Reporting
A study of 523 Canadian physicians’
attitudes on medical tness to drive
found that most physicians would
report unt drivers, but at the same
time believed this reporting could
adversely affect the condentiality
expectations within the patient-
physician relationship.
158
Physicians
153. Kelly RM., Warke T, & Steele J. (1999).
Medical restriction to driving: the awareness
of patients and doctors. Postgrad Med J,
75:537-539.
154. Ibid.
155. Steir TS, Kitai E, Wiener A, & Kahan E.
(2003). Are medical reports on tness to drive
trustworthy? Postgrad Med J. 79:52-54.
156. Di Stefano M & Macdonald W. (2003).
Assessment of older drivers: relationships among
on-road errors, medical conditions and test
outcome. J Safety Res. 34:415-429.
157. Kakaiya R, Tisovec R, & Fulkerson P. (2000).
Evaluation of tness to drive: the physician’s
role in assessing elderly or demented patients.
Postgrad Med J. 107:229-236.
158. Shawn C, Marshall MD, & Gilbert N. (1999).
Saskatchewan physicians’ attitudes and knowl-
edge regarding assessment of medical tness
to drive. Canadian Medical Association Journal.
160(12):1701-1704. Molnar & Eby; Medical
Fitness to Drive & A Voluntary Reporting
Law: The AAA Foundation for Trafc Safety,
pg 30 (2008).
et al. on medically impaired drivers
who are referred for tness-to-drive
evaluations found that very few older
adults retain their license (<3%) when
referred by any source.
150
Notably, very
few (<30%) of referrals came from phy-
sicians- most reports were submitted
by police ofcers- indicating a need
to educate health professionals in this
area. The mean age of the study group
was 80 and had an elevated crash risk
prior to license referral when compared
to controls. The majority of the referrals
were due to an underlying cognitive
impairment such as dementia (45%),
although visual impairment was present
30% of the time. Of the 4,100 reported
individuals, 144, (3.5%) retained a
driver’s license after the process.
Missouri has a voluntary reporting law
and further study is required to deter-
mine the benets between mandatory
reporting States and those that allow
voluntary reporting.
151
Differences in referral rates, laws, and
procedures probably account for varia-
tions among states. The information
from the various states suggests that
more research is needed on the sources
of referral, barriers for reporting and the
medical conditions of these drivers to
determine whether referral is useful or
whether other common conditions are
underreported.
Limitations of Reports: Most states
require that physicians ll out their
state’s forms when assessing tness to
drive. Physicians may experience prob-
lems or barriers to providing the state
with accurate information. Taylor and
colleagues found that patients, in fact,
may not inform their doctor of relevant
medical history that could pertain to
driving.
152
Older drivers may have a
poor understanding of the laws in their
150. Meuser T, Carr DB, & Ulfarsson GF. Motor-Ve-
hicle Crash History and Licensing Outcomes for
Older Drivers Reported as Medically Impaired
in Missouri. Accident Analysis and Prevention.
Accepted November 2008 (in press).
151. Ibid.
152. Taylor J, Chadwick DW, & Johnson T. (1995).
Accident experience and notication rates
in people with recent seizures, epilepsy or
undiagnosed episodes of loss of consciousness.
Q J Med. 88:733-740.
cian in the impaired driver situation.
145
Reporting Facts and Trends
Medically Impaired Driver Reports
National Highway Trafc Safety
Administration (NHTSA) provides
some information on state reporting for
medically impaired drivers.
146
Data from
Oregon in 1993 suggested that close
to 5,300 reports were submitted each
year. About 55% were for drivers over
age 65 years, and surprisingly one-third
of reports were self-referral. Health
care providers accounted for 37% of
all reports. The two leading reasons for
referral were epilepsy (19%) and stroke
(15%). Few people had their license
suspended. In 1995 Florida reported
that 11.7% of referred drivers had their
license suspended.
147
Pennsylvania requires health profes-
sionals to report any medical condition
that can impair the ability to control
or safely operate a motor vehicle.
148
In 2008, Pennsylvania received over
27,000 reports, and 22% of these
individuals have impairments serious
enough to merit recall of their driv-
ing privilege. An additional 21% of
reports result in restrictions placed on
the individual’s driving privilege. Half
of the recalls were attributed to seizure
disorders, while 16% were attributable
to other neurological disease.
149
A recent Missouri report by Meuser,
145. Ferguson v. City of Charleston, 532 US 67.
146. National Highway Trafc Safety Administra-
tion. Family and Friends Concerned about
an Older Driver. Available at www.nhtsa.dot.
gov/people/injury/olddrive/FamilynFriends/state.
htm. (Accessed 11/12/07). Also see, Molnar &
Eby; Medical Fitness to Drive & A Voluntary
Reporting Law: The AAA Foundation for
Trafc Safety (2008).
147. National Highway Trafc Safety Administra-
tion. Family and Friends Concerned about an
Older Driver. www.nhtsa.dot.gov/people/injury/
olddrive/FamilynFriends/state.htm. Accessed
11/12/07.
148. Title 75 PA. CODE § 1518(b) The Vehicle
Code.
149. PENNSYLVANIA DEPARTMENT OF
TRANSPORTATION; PHYSICIAN REPORT-
ING FACT SHEET; March 2008. Available
at www.dmv.state.pa.us/pdotforms/fact_sheets/
fs-pub7212.pdf (Accessed September 23, 2009)
62
report patients to the DMV, physicians
should have patient authorization in
order to disclose medical information.
In these states, physicians who disclose
medical information without patient
authorization may be liable for breach
of condentiality. Nevertheless, this
should not dissuade physicians from
reporting when it is necessary and justi-
ed to protect the patient and/or public.
The AMA recognizes that the safety of
older drivers is a growing public health
concern that is best addressed through
multi-sector efforts to optimize vehicle
design, the driving environment, and
the individual’s driving capabilities.
166
Please refer to chapter 1 in this guide to
review AMA Ethical Opinion E-2.24
“Impaired Drivers and Their Physicians.”
Putting it all together
How can you fulll these competing
legal and ethical duties? In this section,
we provide recommendations for
achieving this balance.
Counsel your patient and if indicated,
include the family.
Patients should be advised of medical
conditions, procedures and medications
that may affect driving performance.
(A reference table of medical conditions
and medications that may affect driving
performance, with recommendations for
each, can be found in Chapter 9.) If you
can get the patient’s permission, involve
the family in the counseling process
whenever it seems appropriate. If the
patient does not have decision-making
capacity (e.g., due to Alzheimer’s
disease), this information should be
given to a cognitively intact surrogate
decision-maker.
Recommend driving cessation
as needed.
As discussed in the previous chapters,
you should recommend that a patient
cease driving if you believe that he/
166. AMA policy H-15.954 Older Driver Safety;
(CSA Rep. 6, A-03).
mittee on Uniform Trafc Laws and
Ordinances (NCUTLO) reporting of a
“Model Driving Impairment Law” has
suggested that physician immunity from
civil liability should be an important
component of any law.
163,164
Physicians
have concerns about breach of con-
dentiality; however, several exceptions
to maintaining condentiality exist. For
example, information may be released
if the patient gives his/her consent,
or may be released without patient
authorization in order to comply with
reporting statutes (such as child abuse
reporting statutes) and court orders.
The Health Insurance Portability and
Accountability Act (HIPAA) has a
regulation that allows for reporting
information that includes a patient’s
protected health information when it is
in the public interest.
165
In some cases,
the act of reporting itself may help
protect the physician from damages
sought by third parties.
Adhering to State Reporting Laws
Because each state has its own reporting
laws, we have provided a state-by-state
reference list in the following chapter.
Please note that information may
have changed since the publication
of this guide. You should contact your
State DMV for the most up-to-date
information.
Please note that in states where there
are no laws authorizing physicians to
163. Reporting of Driver Impairment Model Law;
The National Committee on Uniform Trafc
Laws and Ordinances, at www.ncutlo.org/
impairment.htm Accessed Sept 24th, 2009.
164. Lococo K, Staplin L. (2004) In-Depth Study
to Identify Best Practices for Licensing Drivers
with Medical and Functional Impairments and
Barriers to their Implementation. #DTNH22-
02-P-05111; National Highway Trafc Safety
Administration; 2004.
165. HIPAA (45-CFR-164.512) allows for reporting
to the state when the situation is signicant
enough to put public safety at risk. Source:
http://answers.hhs.gov/cgi-bin/hhs.cfg
Also see 45 C.F.R. Part 160, Subpart B, for
specic requirements related to preemption
of state law, “Permitted uses and disclosures 5.
Public interest and benet activities” Available
at www.hhs.gov/ocr/privacy/hipaa/understanding/
summary/index.html
have raised concerns about mandatory
reporting, stating it can violate privacy,
compromise the ability to counsel
patients, and negatively impact the
doctor-patient relationship.
159
Some
physicians have suggested that man-
datory reporting has the potential to
discourage patients from seeking
health care.
160
Six states have mandatory reporting
requirements: California, Delaware,
Nevada, New Jersey, Oregon, and
Pennsylvania. In California, physicians
are required to report specic conditions
such as seizure disorders or Alzheimer’s
disease, among other conditions. Cable
et al. found that physicians practicing
in mandatory reporting States are more
likely to report impaired drivers to the
licensing agency.
161
Thus, physicians
may choose not to report in certain situ-
ations unless they are required by law to
do so. We are not aware of any studies
that examine the efcacy of mandatory
or voluntary reporting laws, or any that
have drawn comparisons between States
with differing approaches. But, physi-
cians are required to follow the law of
their particular state as it now stands.
We urge you to become familiar with
your state’s laws.
Immunity and Condentiality: Of the 43
states with voluntary reporting laws,
18 currently do not protect reporting
health professionals from liability for
civil damages.
162
The National Com-
159. Molnar & Eby; Medical Fitness to Drive & A
Voluntary Reporting Law: The AAA Founda-
tion for Trafc Safety, pg 30 (2008).
160. Kelly R, Warke T, Steele I. Medical restric-
tions to driving: the awareness of patients and
doctors. Postgrad Med J. 1999;75:537-539. Karen
West et al., The Mandatory Reporting of Adult
Victims of Violence: Perspectives from the
Field, 90 Ky. L.J. 1071 (2001-2002).
161. Cable G, Reisner M, Gerges S, & Thirumava-
lavan V. Knowledge, attitudes, and practices of
geriatricians regarding patients with dementia
who are potentially dangerous automobile
drivers: a national survey. J Am Geriatr Soc.
48(1):100-102. (2000).
162. Lococo K. (2003). Summary of Medical
Advisory Board Practices in the United States.
Task Report Prepared Under NHTSA Contract
No. DTNH22-02-P-05111. Available at
www.aamva.org/KnowledgeCenter/Driver/At-Risk/
ProgramPracticesRecommendationsAndModelLaws
.htm
Chapter 7—Ethical and Legal Responsibilities of the Physician

63
your patient may be potentially at risk
for unsafe driving.
• Any counseling specic to driving
(e.g., documenting that the patient
is aware of the warning signs of
hypoglycemia and its effects on
driving performance).
• Formal assessment of your patient’s
driving-related functions (e.g.,
documenting that the patient has
undergone the ADReS battery and
including the ADReS scoring sheet
in the chart).
• Any medical interventions and
referrals you have made to improve
the patient’s function and any repeat
testing to measure improvement.
• A copy of the DRS report, if the
patient has undergone driver
assessment and/or rehabilitation.
• Your recommendation on whether
the patient should continue driving
or cease driving. If you recommend
that the patient cease driving, include
a summary of your interventions (e.g.,
“sent letter to patient to reinforce
recommendation,” “discussed trans-
portation options and gave copy of
‘Patient Resource Sheet’,” “contacted
family members with patient’s permis-
sion,” and “reported patient to DMV
with patient’s knowledge”). Include
copies of any written correspondence
in the chart or electronic record.
• Follow-up for degree of success in
using alternate transportation options
and any signs of social isolation and
depression. Document any further
interventions, including referral to a
social worker, geriatric care manager,
or mental health professional.
Additional legal and ethical
concerns
What should you do if you nd yourself
in a particularly challenging situation?
In this section, we offer recommenda-
tions for several potential situations:
Situation 1: My patient threatens to sue
me if I report him/her to the DMV.
A patient’s threat to sue should by no
means deter you from complying with
information condential. Even in
States that offer anonymous reporting
or reporter condentiality, it is a good
idea to be open with your patients.
You may wish to remind the patient
that ultimately the physician does not
determine driver licensing. This is the
responsibility of the State. Thus, the
State has the nal decision on deter-
mining whether the patient should still
be allowed to drive.
When submitting your report, provide
only the information necessary or
required to establish that your patient
may be unsafe. Consider giving your
patient a copy of his/her report. By
providing your patients with as much
information as possible, you can involve
them in the process and give them a
greater sense of control.
Before contacting your patient’s family
members and caregivers, request the
patient’s permission to speak with these
parties and document this in the chart.
If your patient maintains decisional
capacity and denies permission for you
to speak with these parties, you must
respect the patient’s wishes.
Document diligently.
Through documentation, you provide
evidence of your efforts to assess and
maintain your patient’s safety. In the
event of a patient or third-party crash
injury, good documentation may protect
you against a judgment from a lawsuit.
To protect yourself legally, you should
document your efforts, conversations,
recommendations, and any referrals for
further testing in the patient’s chart.
167
In other words, you should document
all the steps of Physician Plan for Older
Drivers’ Safety (PPODS) (see page 6)
that you have performed, including:
• Any direct observations of your
patient’s functional status, red ags
as described in PPODS, or driving
history that lead you to believe that
167. Carr DB. The older adult driver. Am Fam
Physician. 2000;61(1):141-148.
she may be an unsafe driver and that
his/her driving cannot be made safe
by any available medical treatment,
adaptive device, or adaptive technique.
As always, base your clinical judgment
on the patient’s driving abilities rather
than the patient’s age. This recom-
mendation should be documented in
the chart and there should be a system
in the ofce setting to check on future
compliance with recommendations.
Know and comply with your State’s
reporting laws.
You must know and comply with your
State’s reporting laws (see Chapter 8).
If you fail to follow these laws, you may
be liable for patient and third-party
injuries.
If your State has a mandatory medi-
cal reporting law, report the required
medical condition(s) using the DMV’s
ofcial form. If your State has a volun-
tary physician reporting law, report the
information using the DMV’s ofcial
form and any other reporting guidelines.
If the DMV’s guidelines do not indi-
cate what patient information must be
reported, provide only the minimum
information necessary to show that your
patient may be an unsafe driver.
Reduce the impact of breaching
patient confidentiality
In adhering to the State’s reporting laws,
it may be necessary for the physician to
breach their patient’s condentiality.
However, you can do several things
to reduce the impact of this on the
patient-physician relationship.
Providing Notice to the DMV
Before reporting to the DMV, tell
your patient what you are about to do.
Explain that it is your ethical, and in
some cases legal, responsibility to refer
him/her to the State DMV, and describe
what kind of follow-up can be expected
from the DMV. Assure your patient
that out of respect for his/her privacy,
you will disclose only the minimum
information required and hold all other
Chapter 7—Ethical and Legal Responsibilities of the Physician

64
• Discuss the nancial and emotional
burden a car collision would cause
them, their family, and all others
involved.
• If your patient is cognitively impaired
and lacks insight into this problem,
the issue must be discussed with the
individual who holds decision-making
authority for the patient and with any
other caregivers. These parties should
understand their responsibility to
prevent the patient from driving.
• If your patient continues to drive and
your state has a physician reporting
law, adhere to the law by reporting
your patient as an unsafe driver (even
if you have already done so previ-
ously, resulting in the revocation of
your patient’s license). If your state
does not have a physician reporting
law, base your decision to report as in
Situation 2 (see above). The DMV,
as the agency that grants and revokes
the drivers license, will follow-up as it
deems appropriate.
Situation 4: My patient threatens to
find a new doctor if I report him/her to
the DMV.
This situation, while unfortunate,
should not prevent you from adhering
to your state’s reporting laws. As a
physician, it is your responsibility to
care for your patients’ health and safety,
regardless of such threats.
Several strategies may help you diffuse
this situation:
• Reiterate the process and information
used to support your recommendation
that the patient stop driving.
• Reiterate your concern for the safety
of your patient, his/her passengers,
and those sharing the road.
• Remind your patient that you try to
provide the best possible care for
his/her health and safety. State that
driving safety is as much a part of
patient care as encouraging patients
to wear a seat belt, keep a smoke
detector in the house, oss their
teeth, and have regular physical
check-ups.
stop driving despite your best efforts,
then you must consider which is more
likely to cause the greatest amount of
harm: breaching the patient’s conden-
tiality versus allowing the patient to
poten-tially injure himself/herself and
third parties in a motor vehicle crash.
According to AMA Policy E-2.24 (see
Chapter 1), “in situations where clear
evidence of substantial driving impair-
ment implies a strong threat to patient
and public safety, and where the physi-
cian’s advice to discontinue driving
privileges is ignored, it is desirable and
ethical to notify the Department of
Motor Vehicles.”
Situation 3: My patient has had his/
her license suspended by the DMV for
unsafe driving, but I am aware that he/
she continues to drive.
This patient is clearly violating the law,
and several questions are raised: Is the
physician responsible for upholding the
law at the expense of breaching patient
condentiality? Since the license
has been revoked by the DMV, is the
driving safety of the patient now the
responsibility of the DMV, the physi-
cian, or both?
There are several steps you can take in
this situation:
• Ask your patient why he/she continues
to drive. Address the specic causes
brought up by your patient (see the
previous chapter for recommendations).
With your patient’s permission, the
family should be involved in nding
solutions such as alternative methods
of transportation.
• Ask your patient if he/she understands
that he/she is breaking the law.
Reiterate your concerns about the
patient’s safety, and ask how he/she
would feel about causing a crash and
potentially being injured or injuring
someone else. Discuss the nancial
and legal consequences of being
involved in a crash without a license
or auto insurance. Many clinicians
will remind the patient and/or family
that the patient could have nancial
liability for any injuries caused by
driving.
your state’s reporting laws. If a patient
threatens to sue, there are several steps
you can take to protect yourself in the
event of a lawsuit:
• Know if your state has passed legisla-
tion specically protecting health
care professionals against liability
for reporting unsafe drivers in good
faith.
168
(This information can be
found in the following chapter.)
• Even if your state has not passed
such legislation, physicians generally
run little risk of liability for follow-
ing mandatory reporting statutes in
good faith. Consult your attorney
or malpractice insurance carrier to
determine your degree of risk.
• Make certain you have clearly docu-
mented your reasons for believing
that the patient is an unsafe driver.
Be aware that physician-patient privilege
does not prevent you from reporting your
patient to the state DMV. Physician-
patient privilege, which is dened as the
patient’s right to prevent disclosure of
any communication between the physi-
cian and patient by the physician, does
not apply in cases of required reporting.
Remind the patient that ultimately the
physician does not determine licensing.
This is the responsibility of the state.
Thus, the state has the nal decision on
determining whether the patient should
still be allowed to drive.
Situation 2: Should I report an unsafe
driver even if my state does not have
any reporting laws?
In this situation, the physician’s rst
priority is to ensure that the unsafe
driver does not drive. If this can be ac-
complished without having the patient’s
license revoked, then there may be no
need to report the patient to the DMV.
Before reporting your patient, you may
address the risk of liability for breaching
patient condentiality by following the
steps listed under Situation 1.
However, if your patient refuses to
168. Tasman A, Kay J, Lieberman JA, Fletcher J
(eds). Psychiatry, 1st edition. Philadelphia: W.B.
Saunders Company; 1997; p. 1809.
Chapter 7—Ethical and Legal Responsibilities of the Physician

65Chapter 7—Ethical and Legal Responsibilities of the Physician
Before consulting the reference list in Chapter 8, it will be helpful to familiarize
yourself with the terms and concepts provided in the Glossary of Terms.
Glossary of Terms
Anonymity and Legal Protection: Several States offer anonymous reporting
and/or immunity for reporting in good faith. More than half of all the States will
maintain the condentiality of the reporter, unless otherwise required by a court
order.
169
Driver Rehabilitation Programs: These programs, run by driver rehabilitation
specialists (DRS), help identify at-risk drivers and improve driver safety through
adaptive devices and compensatory techniques. Clients typically receive a clini-
cal evaluation, driving evaluation, and—if necessary—vehicle modications and
training. (Driver assessment and rehabilitation are discussed in greater detail in
Chapter 5.)
Duty to Protect: In certain jurisdictions state physicians have a legal duty to
warn the public of danger their patients may cause, especially in the case of
identiable third parties.
170
With respect to driving, mandatory reporting laws
and physician reporting laws provide physicians with guidance on their duty
to protect.
Good Faith: Honest and respectful in all professional interactions
171
Immunity for reporting: Many States exempt physicians from liability for civil
damages brought by the patient if the physician reported the patient to the
DMV beforehand.
Mandatory Medical Reporting Laws: In some States, physicians are required to
report patients who have specic medical conditions (e.g., epilepsy, dementia)
to their State DMV. These States provide specic guidelines and forms that can
be obtained through the DMV.
Medical Advisory Boards: Medical Advisory Boards (MAB) generally consist of
local physicians who work in conjunction with the DMV to determine whether
mental or physical conditions may impair an individual’s ability to drive. Some
MABs specify mitigation that would permit continued licensure. MABs vary
among States in size, role, and level of involvement.
Physician Reporting Laws: Some states require physicians to report “unsafe”
drivers to the State DMV, with varying guidelines for dening “unsafe.” The
physician may need to provide: (a) the patient’s diagnosis; and (b) any evidence
of a functional impairment that can affect driving (e.g., results of neurological
testing) to prove that the patient is an unsafe driver.
172
169. Sterns HL, Sterns R, Aizenberg R, & Anapole R. (2001, August). Family and Friends Concerned
About an Older Driver. NHTSA Report No. DOT HS 809 307. “State Reporting Practices.” Wash-
ington, DC: National Highway Trafc Safety Administration.
170. Tarasoff v. Regents of University of California, 13 Cal. 3d 177.
171. The American Medical Association Principles of Medical Ethics; Preamble, generally I-IX. Adopted
June 1957; revised June 1980; revised June 2001. Code of Medical Ethics of the American Medical
Association: Council on Ethical and Judicial Affairs; 2008-2009 Edition. American Medical Associa-
tion, 2008.
172. Messinger-Rapport B & Rader E. (2000). High risk on the highway: how to identify and treat the
impaired older driver. Geriatrics. 55(10)32-45.
• Encourage your patient to seek a
second opinion. A DRS may evaluate
the patient if this has not already
been done, or the patient may consult
another physician.
• If your state DMV follows up on
physician reports with driver retesting,
inform the patient that just as it is
your responsibility to report him/
her to the DMV, it is the patient’s
responsibility to prove his/her driving
safety to the DMV. Emphasize that
the DMV makes the nal decision,
and that only the DMV can legally
take away the license. Remind your
patient that you have done every-
thing medically possible to help him/
her pass the driver test.
• As always, maintain professional
behavior by remaining unemotional
and not expressing hostility toward
your patient even if he/she ultimately
makes the decision to seek a new
physician.

66 Chapter 7—Ethical and Legal Responsibilities of the Physician
Glossary of Terms (continued)
Physician Liability: Previous cases have illustrated situations in which the
physician was held liable for civil damages caused by his/her patient’s car
collision when there was a clear failure to report an at-risk driver to the DMV
prior to the incident.
173
Renewal Procedures: License renewal procedures vary by State. Some States
have age-based renewal procedures; that is, at a given age, the State may reduce
the time interval between license renewal; restrict the ability to obtain license
renewal by mail; require specic vision, trafc law and sign knowledge; and/or
require on-road testing. Very few States require a physician’s report for license
renewal.
174
Restricted Drivers License: Some States offer the restricted license as an
alternative to revoking a driver’s license. Typical restrictions include prohibiting
night driving, limiting driving to a certain distance from home, requiring adap-
tive devices, and shortening the renewal interval. To our knowledge, the efcacy
of these types of restrictions has not been tested.
Third (3rd) Party: The generic legal term for any individual who does not
have a direct connection with the physician or legal transaction, but who
might be affected by it, e.g., anyone injured other than the patient.
173. Capen K. (1994). New court ruling on tness-to-drive issues will likely carry “considerable weight”
across country. Can Med Assoc J. 151(5):667.
174. Tripodis VL. (1997). Licensing policies for older drivers: balancing public safety with individual
mobility. Boston Coll Law Rev. 38 B.C.L. Rev 1051.

CHAPTER 8
State Licensing and
Reporting Laws

69
effects of license renewal timing, and
tests of visual acuity, knowledge and
road examinations on older driver fa-
talities. The researchers concluded that
tests of visual acuity were associated
with a lower fatal crash risk for older
drivers.
179
Another study investigated
the effect of renewal testing by compar-
ing the crash rates of older adults in
Indiana and Illinois (which at the time
required vision, knowledge, and road
testing at age 75) with similar controls
in states that do not have age-based
testing (e.g., Ohio and Michigan). In
states that had age-based testing, there
was a 7 percent reduction in involve-
ment in injurious crashes, but an
increase in at-fault single-vehicle crash
rates.
180
The authors concluded that
routine road testing was not warranted.
An examination of the effects of shorter
licensure renewal periods for older
adults along with an analysis of the
crashes before and after discontinuation
of road tests for those under 75 in Illinois
was performed. Comparing changes in
1989 from before to after new policies
were enacted, no effects were observed
on crashes, fatal crashes, crash rates, or
licensure rates of older drivers. Although
there are no data to support an im-
provement in public safety when
road testing the general older adult
population during license renewal,
mandatory road testing requirements
along with vision testing have been
179. Levy, D. T. (1995). The relationship of age
and state license renewal policies to driving
licensure rates. Accid Anal Prev. 27(4):461–467.
180. Lange, J. E., & McKnight, A. J. (1996). Age-
based road test policy evaluation. Transport Res
Rec. 1550:81–87.
one year (Illinois at age 87) to ve years
(Arizona, Colorado, South Carolina).
Surprisingly, one state actually has a
decelerating renewal for older drivers,
with no renewal required after age 65
(Tennessee). Over time, there has been
a trend toward lengthening the period
of license renewal. Seventeen states
have special renewal provisions for older
drivers, including in-person renewal,
vision tests, written tests, road tests, a
medical certication of tness, or some
combination of these. Thus, a minority
of states have requirements for more-
frequent testing for adults over 65.
176
A variety of options can apply due to
the special renewal provisions of older
drivers. These include license renewal,
revocation or suspension, restriction,
or shortening of the renewal cycle.
A recent review indicates that in some
jurisdictions in Australia age-based
assessment has not been associated with
safety benets.
177
Some of the literature
supports vision testing during license
renewal for older adults. One investiga-
tor compared occupant motor vehicle
fatalities for those over age 60 in states
with and without a vision-related reli-
censing laws and concluded there would
be a 12.2-percent reduction in fatalities
over the period of study if the majority
of states without such laws were to adopt
one.
178
Another study examined the
176. Morrisey, M. A., & Grabowski, D. C. (2005).
State motor vehicle laws and older drivers.
Health Econ. 14(4):407–419.
177. Fildes, B. N., Charlton, J., Pronk, N., et al.
(2008). An Australian model license reas-
sessment procedure for identifying potentially
unsafe drivers. Trafc Inj Prev. 9:350–359.
178. Shipp, M. D. (1998). Potential human eco-
nomic cost-savings attributable to vision testing
policies for driver license renewal 1989–1991.
Optom Vis Sci. 75:103–118.
Each state has its own licensing and
license renewal criteria for drivers of
private motor vehicles. In addition,
certain states require physicians to
report unsafe drivers or drivers with
specic medical conditions to the
driver licensing agency.
This chapter contains licensing agency
contact information, license renewal
criteria, reporting procedures and medi-
cal advisory board information, listed
by state. These materials are intended
to guide physicians in understanding
their legal responsibilities and managing
the driving safety of their patients. The
information in this chapter should not
be construed as legal advice nor used to
resolve legal problems. If legal advice
is required, please consult an attorney
who is licensed to practice in your state.
Please note that information may have
changed since the publication of this guide.
You should contact your State DMV for
the most up-to-date information.
License renewal practices
among states
Practices vary among states for license
renewal based on age. A recent review
summarized some of these nuances, and
are reviewed in this paragraph.
175
Many
states require renewal every four to ve
years, and one state requires no renew-
als until age 65 (Arizona). Fourteen
states require some type of accelerated
renewal for older drivers, ranging from
age 60 to 80, with the length of the
accelerated renewal cycle ranging from
175. Molnar, L. J., & Eby, D. W. (2005). A brief look
at driver license renewal policies in the United
States. Public Policy and Aging Report. National
Academy on an Aging Society. 15;1, 13–17.
CHAPTER 8
State Licensing and
Reporting Laws

70 Chapter 8—State Licensing and Reporting Laws
safety benets for mandatory assessment
programs.
185
Similarly, a comparison of
Swedish and Finnish licensing practices
did not demonstrate an advantage for
age-related license renewal require-
ments. Finland requires regular medi-
cal evaluations starting at age 70 for
license renewals, whereas Sweden has
no age-related requirements. The Finn-
ish program not only did not have a
reduction in crash rates but was actually
associated with higher pedestrian fatal-
ity rates.
186
Specific state information
Information on each specic state was
obtained from each state’s driver licens-
ing agency and reects the most current
information at the time of publication.
Please note that this information is
subject to change. Contact your specic
states statutes for up-to-date changes
in the laws or requirements. This is
especially important when it comes to
creating a clinic policy or deciding on
an individualized approach to reporting.
Legal counsel is recommended to advise
your decision-making in this area.
When information was not available
from an individual state’s driver licensing
agency, the following references were
used and remain as useful resources for
clinicians. The Insurance Institute for
Highway Safety and Insurance Informa-
tion Institute sites are usually updated
at frequent intervals and the Web site
will indicate the latest version.
185. Langford, J., Fitzharris, M., Newstead, S., & Ko-
ppel, S. (2004). Some consequences of different
older driver licensing procedures in Australia.
Accid Anal Prev. 36: 993–1001.
186. Hakamies-Blomqvist, L., Johansson, K., &Lun-
dberg, C. (1996). Medical screening of older
drivers as a trafc safety measure: a comparative
Finnish-Swedish evaluation study. J Am Geriatr
Soc. 446:650–653.
noted to decrease license renewal
rates.
181
A recent U.S. study raises further doubt
about the efcacy of intensive screen-
ing during the license renewal process.
Vision tests were not found to reduce
crash risk, while an in-person renewal
requirement reduced fatalities for driv-
ers 85 and older by 16.3 percent.
182
This
may result from license renewal staff
requesting that older adults be evaluat-
ed, with subsequent revocation of their
license or some older drivers deciding
to give up their licenses rather than go
through the renewal process.
These testing procedures and regulations
do impose signicant costs on states,
and at times inconvenience and costs
to individual drivers. If licenses are
revoked, older adults face the problems
of restricted mobility and loss of out-of-
home activities, which may decrease
social connectedness. In addition, the
impact on family members and caregiv-
ers, such as time away from work, is
not insignicant. This burden must
be carefully weighed against the actual
“added value” or benets of improved
public safety.
183
International experience
In Australia, different states have
various requirements for older adults,
ranging from no license renewal
requirements, to vision, road, and/or
requirement for a medical evaluation
from a physician.
184
One study found
similar crash rates across populations
based on the number of licenses issued,
indicating there were no demonstrable
181. Levy, D. T., Werrick, J. S., Howard, K. A. (1995).
Relationship between driver’s license renewal
policies and fatal crashes involving drivers 70
years and older. JAMA. 274:1026–1030.
182. Grabowski, D. C., Campbell, C. M., Morrisey,
M. A. (2004). Elderly licensure laws and motor
vehicle fatalities. JAMA. 291:2840–2846.
183. Miller, T.R., & Levey, D.T. (2000). Cost-out-
come analysis in injury prevention and control:
eighty-four recent estimates for the United
States. Med Care. 2000;28(6):562–582.
184. Fildes, B., Pronk, N., Langford, J., Hull, M.,
Frith, W., & Anderson, R. (2000). Model
license re-assessment procedure for older and
disabled drivers (Report # AP-176/00).
Canberra, Australia: Ausroads.
71
Name of State & DMV
contact information
Alabama Department of Public Safety
PO Box 1471
Montgomery, AL 36102-1471
www.dps.state.al.us
334-242-4239
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
20/40
20/60 in best eye with or without
corrective lenses. Class D only.
Yes-for daylight driving only for
2 years then will be reviewed.
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
110° both eyes-Class D only
Keystone View
Color vision requirement Must be able to distinguish between amber, red, and green. New and professional drivers only
Restricted licenses Yes
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
4 years
In-person
Yes
No
No
Age-based renewal procedures No special requirements for age.
Reporting Procedures
Mandatory medical reporting No
Physician/medical reporting Physician reporting is encouraged.
Immunity Yes
Legal protection Yes
DMV follow-up Driver notified in writing of referral. For diabetes, seizures, and convulsions, etc., a form is sent to be
completed by patient’s doctor.
Other reporting Will accept information from courts, police, other DMVs, family members, and anyone who completes
and signs the appropriate forms.
Anonymity Yes, unless the subjects request a copy of their medical records by completing the necessary forms,
having them notarized, and paying the proper fee for copying these records.
Medical Advisory Board
Role of the MAB The MAB was created to assist the Director for Public Safety concerning the medical aspects of driver
license. The MAB consists of at least 18 members, with the chair elected on an annual basis. They as-
sist the Medical Unit.
Medical Review contact
information
The Medical Unit may be reached at 334-242-4239.
Alabama
72
Alaska
Name of State & DMV
contact information
Alaska Department of Motor Vehicles
3300 B Fairbanks Street
Anchorage, AK 99503
www.state.ak.us/dmv/
907-269-5551
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
20/40
20/100 needs report from eye
specialist—license request deter-
mined by discretion
Only under certain conditions spe-
cifically recommended by physician
in regards to lighting conditions,
number of miles to and from specific
locations. Need letter stating “with
the bioptic telescopes this patient
can safely operate a motor vehicle
without endangering the public under
the following conditions:”
Visual fields Minimum field requirement .........................................................None
Color vision Is there a color vision requirement? .............................................No
Road test Type of road test ........................................................................N/A
Restricted licenses Yes
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
5 years
Mail in every other cycle
Yes, at in-person renewal
No
No
Age-based renewal procedures No renewal by mail for drivers 69+, and to drivers whose prior renewal was by mail.
Reporting Procedures
Mandatory medical reporting No
Physician/medical reporting A licensee should self-report medical conditions that cause loss of consciousness to the DMV.
Immunity No
Legal protection N/A
DMV follow-up All medical information submitted to DMV is reviewed by the Department of Public Safety personnel.
Other reporting Requires retest/re-exam upon receipt of documented problem by law enforcement, other DMVs, and
family members.
Anonymity N/A
Medical Advisory Board
Role of the MAB Alaska does not have a Medical Advisory Board
Medical Review contact
information
Referrals for reexamination can be sent to:
Department of Administration, Juneau Driver Licensing | Po Box 110221 | Juneau, Alaska 99811
907-465-4361 | fax 907-465-5509
73
Arizona
Name of State & DMV
contact information
Arizona Motor Vehicle Department
Medical Review Program
Mail Drop 818Z
PO Box 2100
Phoenix, AZ 85001-2100
www.dot.state.az.us/MVD/mvd.htm
623-925-5795 phone
623-925-9323 fax
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
20/40
20/60 in best eye restricted to
daytime only
No
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
70°, 35° Nasal
Keystone view
Color vision Is there a color vision requirement? .............................................Commercial Drivers Licenses only
Road test Depends on physician recommendation and provided information
Restricted licenses Yes, daylight only
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
12 years
N/A
Yes
No
If recommended
Age-based renewal procedures At age 65, reduction of cycle to 5 years. No renewal by mail after age 70
Reporting Procedures
Mandatory medical reporting No
Physician/medical reporting Yes
Immunity Yes
Legal protection Reporting immunity is granted
DMV follow-up Follows physician recommendation
Other reporting Will accept information from courts, police, other DMVs, family members and other resources.
Anonymity Yes
Medical Advisory Board
Role of the MAB Reports are reviewed by the Medical Review Program staff to determine of a license requires
a re-examination of driving skills/written testing, or medical/psychological evaluation.
Medical Review contact
information
Mail Drop 818Z
Medical Review Program
PO Box 2100
Phoenix, AZ 85001
623-925-5795
Fax 623-925 9323
74
Name of State & DMV
contact information
Arkansas Driver Control
Hearing Officer, Rm 1070
1910 West 7th
Little Rock, AR 72203
www.state.ar.us/dfa/odd/motor_vehicle.html
501-682-1631
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/50
20/40
20/40 in best eye for unrestricted;
20/60 restricted
Yes, under certain circumstances.
20/50 through telescope, 20/50
through carrier/must still have
minimal field of vision 105°
Visual fields Minimum field requirement .........................................................Both eyes 105°
Color vision Is there a color vision requirement? .............................................OPTEC Screening Machine
Road test Type of road test ........................................................................Standardized
Restricted licenses Yes, daylight driving only at physicians’ recommendation—
however must meet minimal visual requirements
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
4 years
In person, and by mail only
if out of state
Yes
No
No
Age-based renewal procedures No
Reporting Procedures
Mandatory medical reporting No
Physician/medical reporting We do encourage unsafe driver’s to be reported to our office.
Immunity No
Legal protection No
DMV follow-up Medical information is reviewed by the director of Driver Control. An appointment is scheduled within 2
weeks of receipt. At that time, a medical form is given to the licensee for completion by a physician. If
the medical exam is favorable, the road test is given.
Other reporting Will accept information from courts, police, other DMVs, and family members.
Anonymity N/A
Medical Advisory Board
Role of the MAB Arkansas has no Medical Advisory Board.
Medical Review contact
information
Unsafe drivers may be referred to Driver Control at the contact above.
Arkansas
75
Name of State & DMV
contact information
Licensing Requiring/Renewal
California Department of Motor Vehicles
2415 First Avenue, Mail station C152
Sacramento, CA 95818-2698
www.dmv.ca.gov/
916-657-6550
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
One eye 20/70 if other is 20/40. This
is a screening standard, if failure then
referral to vision specialist, possible
road test. Not an absolute standard.
20/40. Also a screening standard
20/40 (with road test given unless
stable, long-standing condition
Better than 20/200, best corrected, in
at least one eye. Cannot use bioptic
telescope to meet standard.
Yes, daylight driving only.
Visual fields Minimum field requirement .........................................................75 degrees for a person wearing a
bioptic telescopic lens. No minimum
field exists for any other drivers
Color vision requirement No
Type of road test The Driving Performance Evaluation (DPE) is administered for original licensing and for some experi-
enced impaired drivers (e.g., drivers with vision problems). For other experienced drivers (e.g., drivers
with cognitive deficits), the Supplemental Driving Performance Evaluation (SDPE) is administered.
Restricted licenses Yes, varied restrictions—most commonly to corrective lenses.
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
5 years
In person or, if qualify, mail renewal
for no more than 2 license terms in
sequence.
Yes, at in person, not mail, renewal
At in-person renewal, unless driver
has had 2 and would be eligible for a
3rd sequential mail renewal, if there
were such. These drivers don’t take a
written test.
Not generally, unless evidence of
highly likely impairment for driving.
Age-based renewal procedures No mail renewal at 70+
Reporting Procedures
Mandatory medical reporting Yes, physicians are required to report all patients diagnosed with ‘disorders characterized by lapses of
consciousness’. Law specifies that this definition includes Alzheimer’s ‘and those related disorders that
are severe enough to be likely to impair a person’s ability to operate a motor vehicle.’
Physician reporting laws Physicians are not required to report unsafe drivers. However, they are authorized to report, given their
good faith judgment that it’s in the public interest.
Immunity Yes, if condition is required to be reported. (A physician who has failed to report such a patient may be
held liable for damages.) A physician has immunity from reporting a condition, even if it not required, if
in good faith, the physician believes it will serve the public interest.
Legal protection See above
California
76
California (continued)
DMV follow-up The medical information obtained from physician is reviewed by DMV hearing officers within Driver
Safety Branch. Driver will be reexamined; at conclusion of process DMV may take no action, impose
restrictions, limit license term, order periodic reexaminations, suspend or revoke the driver’s license.
Other reporting Basically anyone—DMV will accept information from driver him or herself, courts, police, other DMVs,
family members and other resources.
Anonymity If so requested, name will not be divulged (unless court order mandates disclosure)
Medical Advisory Board
Role of the MAB Gathers specialists for panels on special driving related topics (e.g., vision). Panels make policy recom-
mendations to DMV for dealing with groups of drivers having a particular type of impairment. No recom-
mendations are made regarding individuals as such.
Medical Review contact information MAB no longer meets as a group. For further information contact:
Post Licensing Policy
California Dept. of Motor Vehicles
2415 First Ave., Mail Station C163
Sacramento, CA 95818-2698
916-657-5691
77
Name of State & DMV
contact information
Colorado Division of Motor Vehicles
Driver’s License Administration
1881 Pierce Street, Room 136
Lakewood, CO 80214
www.colorado.gov/revenue/dmv
303-205-5646
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40*
20/40
20/40
No absolute minimum acuity. Will
license any individual that physician/
optometrist feels is not a danger.
Yes, however we are going to revisit
the issue in the near future.
Visual fields Minimum field requirement ......................................................... Yes, we now test for minimum
horizontal fields.
Color vision requirement No
Restricted licenses Yes: based on the results of the vision screening test and/or doctor’s recommendations.
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
5 years
If eligible, mail in every other cycle
Yes, unless mail-in renewal
Only if point accumulation results in
suspension
No, unless condition has developed
since last renewal that warrants road
test.
Age-based renewal procedures All licenses are valid for 5 years. However, license holders 61 and older cannot renew by mail.
Reporting Procedures
Mandatory medical reporting No
Physician/medical reporting Drivers should self-report medical conditions that may cause a lapse of consciousness, seizures, etc.
Physicians are encouraged but not required to report patients who have a medical condition that may
affect their ability to safely operate a motor vehicle.
Immunity Yes—no civil or criminal action may be brought against a physician or optometrist, licensed to practice
in Colorado, for providing a written medical or optometric opinion.
Legal protection No
DMV follow-up Driver notified in writing of referral. Driver undergoes re-examination. One circumstance for retest:
incident report from law enforcement. Medical clearance may be required from a physician.
Restrictions may be added to license.
Other reporting Will accept information from courts, police, other DMVs and family members.
Anonymity Not confidential
Medical Advisory Board
Role of the MAB Colorado does not currently retain a medical advisory board.
Medical Review contact information Questions about medical review can be referred to 303-205-5788
* Unless the driver is blind in one eye, testing each eye is not typically conducted.
Colorado
78
Name of State & DMV
contact information
Connecticut DMV Medical Review Division
60 State Street
Wethersfield, CT 06161-2510
http://dmvct.org/
860-263-5223
Fax: 860-263-5774
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
20/40
20/70 better eye restricted; some
circumstances allow for license at
20/200 or better
No
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
100° monocular; 140° binocular
OPTEC 1000
Color vision Is there a color vision requirement? .............................................No (only for commercial drivers)
Road test A general on the road skills test with Motor Vehicle instructor or licensing agent. Test for “graduated
license’ conducted by off-site staff who makes and appt. with applicant at residence and conducts test
in State-owned, dual control vehicle. Applicant with specific needs is trained/tested by a Handicapped
Driver Training Unit certified driving instructor.
Restricted licenses Graduated license considerations include applicant’s health problem/condition, accident record and
driving history. Restrictions include: daylight only, corrective lenses, no highway driving, automatic
transmission only, required external mirrors, special controls or equipment, use of hearing aid.
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
6 years
In-person at DMV full-service branch,
mobile units scheduled locations,
satellite offices, license renewal
centers, authorized AAA offices.
Yes, at age 65.
No
Only for new applicants or for
applicants whose license has
expired for two or more years.
Age-based renewal procedures Yes, age 65+ may renew for 2 years; age 65+ may renew by mail upon written application showing
hardship which shall include but not limited to proximity of operator’s residence to DMV renewal facility.
Reporting Procedures
Mandatory medical reporting No
Physician/medical reporting Sec 14-46 states that “physicians may report to the DMV, in writing the name, age, and address of any
person diagnosed by him to have any chronic health problem which in the physicians judgment will
significantly affect the person’s ability to safely operate a motor vehicle.”
Immunity No civil action my be brought against the commissioner, the department or any of its employees, the
board or any if its members or any physician for providing any reports, records, examinations, opinions
or recommendations. Any person acting in good faith, shall be immune from liability.
Legal protection Only the laws regarding immunity apply.
DMV follow-up Driver notified in writing of referral to MAB. If MAB requires additional information for review in order to
make a recommendation, driver is requested to file the additional medical information requested; entire
file is referred back to MAB and driver is notified of such referral.
Connecticut
79
Connecticut (continued)
Other reporting State regulations, require “reliable information’ to be on file for DMV to initiate a medical review case.
This includes a written, signed report from person in medical/law enforcement profession., or a third
party report on the DMV affidavit which requires signing in the presence of a notary public.
Anonymity All information on file in a medical review case is classified as “confidential” but is subject to release to
the person at their representative, upon written authorization from the person to release the data.
Medical Advisory Board
Role of the MAB MAB must be comprised of 8 specialties: general medicine or surgery, internal medicine, cardiovascular,
medicine, neurology, or neurological surgery, ophthalmology, orthopedics, psychiatry or optometrist.
Advise commissioner on health standards relating to safe operation of motor vehicles; recommend
procedures and guidelines for licensing individuals with impaired health; assist in developing
medically acceptable standardized report forms; recommend training course for motor vehicle
examiners on medical aspects of operator licensure; undertake any programs/activities commissioner
may request relating to medical aspects of motor vehicle operator licensure; make recommendations
and offer advice on individual health problem cases referred and establish guidelines for dealing with
such individual cases.
Medical Review contact
information
Department of Motor Vehicles
Medical Review Division
60 State Street
Wethersfield, CT 06161-2510
80
Name of State & DMV
contact information
Delaware Department of Safety
Division of Motor Vehicles
Medical Records
PO Box 698
Dover, DE 19903
www.dmv.de.gov
302-744-2507
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
20/40
20/50 restricted license, beyond
20/50 driving privileges denied
Yes, on a case by case basis:
daytime only
Visual fields Minimum field requirement .........................................................None
Color vision Is there a color vision requirement? .............................................None
Restricted licenses Yes, daytime only
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
5 years
In person
Yes, must pass vision screening
No
No
Age-based renewal procedures No
Reporting Procedures
Mandatory medical reporting Yes. Failure to do so is punishable by a fine of $5 to $50. Physicians should report patients subject to
“losses of consciousness due to disease of the central nervous system.”
Physician/medical reporting Yes
Immunity Yes
Legal protection Unknown
DMV follow-up Driver notified in writing of referral; license suspended and further examination necessary.
Other reporting DMV will accept information from courts, other DMVs, police, and family members.
Anonymity Yes. DMV protects the identity of the reporter.
Medical Advisory Board
Role of the MAB If the DMV receives conflicting or questionable medical reports, they are sent to the MAB for a determi-
nation as to whether or not a person is medically safe to operate a motor vehicle.
Medical Review contact information Medical Records Section - Driver Improvement Unit
PO Box 698
Dover, DE 19903-0698
Phone: 302-744-2507
Fax: 302-739-5667
Delaware
81
Name of State & DMV
contact information
District of Columbia Department of Motor Vehicles
Medical Review Office
301 C Street NW., Room 1033
Washington, DC 20001
http://dmv.washingtondc.gov/
202-727-6244
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/70
20/40
20/40 acuity; 20/70 in better eye
requires 140 E visual field for
restricted license.
No
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
130° both eyes (may be approved by
director at 110°)
Confrontation or perimetry (Binocular)
Color vision requirement New drivers
Type of road test Road test is required for new drivers. Senior citizens may be required to take the read test on an
observational basis. Also, some physical disabilities may require re-testing.
Restricted licenses Yes: acuity not less than 20/70 and daytime, if field of vision is 140°
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
5 years
IDC drivers with clean driver record
and no medical requirements can
now renew driver licenses on-line
Yes
Yes, however drivers are allowed a
6 months grace period
No
Age-based renewal procedures At age 70, the licensee must have the physician complete the certification on the drivers license
application form.
Reporting Procedures
Physician/medical reporting If patient has a medical condition that may impair your ability to safely operate a motor vehicle, even
temporarily, you must provide a Medical and/or Eye Report* from your physician. Some of these condi-
tions include: Alzheimer’s disease: Requires a Medical Report* and the completion of the knowledge
and road skills tests; Seizure Disorder/Loss of Consciousness: Requires a Medical Report* DC regulation
states you must be seizure-free for at least twelvemonths prior to obtaining a driver’s license. If you are
currently licensed and experience a seizure or loss of consciousness, you must report the incident to
DMV within 30 days. Unless your physician indicates the seizure was due to a change in medication,
or strictly nocturnal, DMV will suspend your driving privilege for twelve months from the date of the
last episode; Insulin-dependent Diabetes: Requires a Medical and Eye Report; Vision impairment (i.e.,
glaucoma, cataracts, eye disease, and monocular vision): Requires an Eye Report*
Immunity No
Legal protection No
District of Columbia
82
District of Columbia (continued)
DMV follow-up DMV will use the medical information provided by your physician to determine if a driver’s license may
be issued or issued with restrictions. We may also issue a driver’s license for a shorter duration based
on your physician’s information. Also, if your doctor recommends follow-up Medical and/or Eye Reports,*
we will track this information to ensure compliance. If we do not receive the follow-up reports within the
timeframe specified by your physician, your license will be subject to suspension.
Other reporting A Medical Report* is also required when a law enforcement officer suspects a driver may have a medi-
cal condition that led to a traffic citation or accident. If DMV receives a detailed, written statement from
a family member, law enforcement officer, or physician related to the unsafe driving of a resident, we
will also require the resident to complete a Medical Report.* Driving tests may also be required in any of
these situations, depending on the circumstances.
Anonymity Yes, reporters are allowed to remain anonymous
Medical Advisory Board
Role of the MAB DC-DMV does not currently have a Medical Advisory Board.
Medical Review contact information Referrals can be made to the contact above.
* Available at www.dmv.washingtondc.gov/info/forms/medical_eye_pdf.shtm
83
Name of State & DMV
contact information
Florida Division of Drivers License
Medical Review
Neil Kirkman Building, Room A227-MS 86
Tallahassee, FL 32399-0500
www.hsmv.state.fl.us/ddl/dlfaq_new.html
850-488-8982 phone
850-921-6147 fax
Licensing Requirements
Visual acuity Each eye without correction ........................................................
Both eyes without correction .......................................................
Each eye with correction.............................................................
Both eyes with correction ...........................................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40: 20/50 or worse referred to eye
specialist for possible improvement
20/40: 20/50 or worse referred to eye
specialist for possible improvement
20/70, other eye better than 20/200
20/70, unless one eye 20/200
20/40
20/70
No
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
130° horizontal
None, Goldman by eye specialist if
indicated
Color vision requirement No
Type of road test Standard Road Test
Restricted licenses Yes: Corrective lenses, outside rearview mirror, business &/or employment purposes only, daylight
driving, automatic transmission, power steering, directional signals, grim on steering wheel, hearing
aid, seat cushion, hand control or pedal ext, left foot accelerator, probation interlock device, medical
alert bracelet, educational purposes, graduated license restrictions, other restrictions.
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
4–6 years, depending on driving
history
In-person, every 3
rd
cycle
At in-person renewal only
Depending on driving history and/or
DL supervisor requires on the basis
of observation of physical or mental
impairments
Only if DL supervisor requires on the
basis of observation of physical or
mental impairments
Age-based renewal procedures None
Reporting Procedures
Mandatory medical reporting No
Physician/medical reporting “Any physician, person or agency having knowledge of a licensed driver or applicant’s mental or physi-
cal disability to drive may report the person to the Department of Highway Safety and Motor Vehicles.”
Forms are available on DHSMV Web site, as well as at local driver license offices. Physicians are
“authorized” by law and encouraged to report—DDL Medical Section provides other forms as situation
requires.
Immunity The law provides that no report shall be used as evidence in any civil or criminal trial or in any court
proceeding.
Legal protection Florida law “authorizes” the physician to report unsafe drivers.
DMV follow-up Investigation: Sanction actions if needed, Driver notified in writing.
Other reporting Law authorizes any person, physician or agency.
Anonymity Yes
Florida
84
Florida (continued)
Medical Advisory Board
Role of the MAB To advise the Department on medical criteria and vision standards and to make recommendations on
mental and physical qualifications of individual drivers.
Medical Review contact information MAB Chairperson
DHSMV/DDL/Driver Improvement Medical Section
2900 Apalachee Parkway
Tallahassee, FL 32399-0570
Telephone: 850-488-8982
Fax 850-921-6147

85
Name of State & DMV
contact information
Georgia Department of Public Safety
Attn: Medical Unit
PO Box 1456
Atlanta, GA 30371
www.dds.ga.gov/drivers/index.aspx
678-413-8500 or 678-413-8600
Outside Atlanta metro
866-754-3687
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/60
20/60
20/60
20/60 in either eye with or without
corrective lenses.
Yes, permitted for best acuity as low
as 20/200, with restrictions. 20/60
through telescope; 20/60 through
carrier
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
140° each eye; 140° both eyes
Juno Vision machine
Color vision requirement None
Type of road test N/A
Restricted licenses Yes
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
4 years
In person
Yes
Not required for renewals
Not required for renewals
Age-based renewal procedures None
Reporting Procedures
Mandatory medical reporting Yes. Physicians should report patients with a diagnosed “conditions hazardous to driving”
Physician/medical reporting Yes, physicians may report a person who has a handicap which would render the individual incapable
of safely operating a motor vehicle
Immunity No
Legal protection No
DMV follow-up Medical evaluation and retest
Other reporting Will take information from anyone with knowledge that the driver may be medically or mentally unsafe.
Anonymity No
Medical Advisory Board
Role of the MAB The Medical Advisory Board advises agency personnel on individual medical reports and
assists the agency in the decision making process.
Medical Review contact information Department of Motor Vehicle Safety
C/O Medical Unit
PO Box 80447
Conyers, GA, 30013
Georgia
86
Name of State & DMV
contact information
Honolulu Division of Motor Vehicles & Licensing
Drivers License Branch
1199 Dillingham Boulevard, Bay A-101
Honolulu, HI 96817
www.co.honolulu.hi.us/mvl.index.htm
808-532-7730
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
20/40
20/40 for better eye
Not allowed to meet visual field
requirements, however permitted to
use while driving
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
70° one eye
Eye testing machine or eye specialist
certification
Color vision Is there a color vision requirement? .............................................No
Road test N/A
Restricted licenses Yes
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
2, 4 or 6 years
In person, or by mail
Yes
No
Only if necessary
Age-based renewal procedures After age 72, must renew every 2 years. Age 15 to 17 every 4 years, age 18 to 71 every 6 years
Reporting Procedures
Mandatory medical reporting No
Physician/medical reporting No
Immunity No
Legal protection No
DMV follow-up Driver notified in writing of referral.
Other reporting Will accept information from courts, police, other DMVs, and family members.
Anonymity N/A
Medical Advisory Board
Role of the MAB Action based on recommendation of majority.
Medical Review contact
information
General Information: Department of Transportation 808-692-7656
Case Specific, County of Issue:
Honolulu 808-532-7730
Hawaii: 808-961-2222
Kauai: 808-241-6550
Maui: 808-270-7363
Hawaii
87
Name of State & DMV
contact information
Idaho Transportation Department
Division of Motor Vehicles, Driver Services
PO Box 7129
Boise, ID 83707
http://itd.idaho.gov/dmv/online_services.htm
208-334-8735
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
20/40 in better eye for unrestricted
license; 20/50-20/60 requires annual
testing; 20/70 denied license
Yes, if acuity is 20/40 through lens,
20/60 through carrier
Visual fields Minimum field requirement .........................................................None
Color vision requirement None
Type of road test Annual road test may be required to coincide with vision or medical re-testing requirements
Restricted licenses Available
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
DL expires 5 days after age 18 and
age 21. 4-year renewal age 21 and
older. 8-year renewal for age 21 to 62.
Mail in every other cycle, if 4 year DL,
not CDL’s
Yes
No
Only if requested by examiner, law
Enforcement agency, family member
or DMV. An annual road test may be
required to coincide with vision or
medical re-testing requirements.
Age-based renewal procedures After age 69, no renewal by mail.
Reporting Procedures
Physician/medical reporting Yes (not specified)
Immunity None
Legal protection N/A
DMV follow-up License suspended upon referral.
Other reporting Will accept information from family members, other DMVs, and law enforcement officers.
Anonymity Not anonymous or confidential
Medical Advisory Board
Medical Desk Technician The medical information submitted is initially reviewed by employees within the Driver Support Division
who work specifically with medical cases.
Role of the MAB Idaho does not have an MAB.
Medical Review contact information MVR/Medical Unit Supervisor can be reached at 208-334-8716
Idaho
88
Name of State & DMV
contact information
Illinois Office of the Secretary of State
Driver Services Department–Downstate
2701 S. Dirksen Parkway
Springfield, IL 62723
Driver Services Department–Metro
17 N. State Street, Suite 1100
Chicago, IL 60602
www.sos.state.il.us/departments/drivers/drivers.html
217-785-0963
312-814-2975
Licensing Requirements
Visual acuity Each eye with/without correction ...................................
Both eyes with/without correction .................................
If one eye blind—other with/without correction ..............
Absolute visual acuity minimum ....................................
Are bioptic telescopes allowed? ....................................
20/40
20/40
20/40
20/40 in better eye unrestricted; 20/70 in
better eye daylight only restrictions,
Yes, may have 20/100 in better eye and 20/40
through bioptic telescope.
Visual fields Minimum field requirement ............................................
Visual field testing device ..............................................
105° one eye, 140° both eyes
Stereo optical testing machine
Color vision Is there a color vision requirement? ................................ No
Road test Type of road test ...........................................................On-road driving test
Restricted licenses Yes: daytime, two outside mirrors
License Renewal Procedures
Standard Length of license validation...........................................
Renewal options and conditions ....................................
Vision testing required at time of renewal? ....................
Written test required? ...................................................
Road test required? ......................................................
4 years
Mail in every other cycle for drivers with clean
records and no medical report
At in-person renewal only
Every 8 years unless clean driving record
Only for applicants age 75+
Age-based renewal procedures Age 81–86 every 2 years, at age 87 reduce renewal to 1 year. Age 75+ no renewal by mail, vision test
required, and on-road driving test required.
Reporting Procedures
Mandatory medical reporting Are physicians required/encouraged to report “unsafe”
drivers?
Are physicians required to report patients with certain
medical conditions?
Physicians are encouraged to inform patients
of their responsibility to notify the Secretary
of State of any medical conditions that may
cause a loss of consciousness or affect safe
operation of a motor vehicle within 10 days of
becoming aware of the condition.
No
Physician/medical reporting Are physicians exempt from liability for civil damages
caused by the patient if they report the patient to the
DMV beforehand?
Yes
Immunity Does the State offer the physician legal protection for
breaking the patient’s confidentiality?
N/A. Illinois is not a mandatory reporting State.
Legal protection How does the DMV follow up? Driver notified in writing of referral. Driver
required to submit a favorable medical report.
Determination of further action based on
various scenarios.
Illinois
89
Illinois
DMV follow-up Aside from physicians, who else can report? Will accept information from courts, foreign
State DMVs, law enforcement, member of
the IL Medical Advisory Board, NDR, PDPS,
SOS management employee, FMCSA, driver
rehabilitation specialist, or self-admission.
Other reporting Does the DMV protect the identity of the reporter? Yes
Anonymity Does the DMV protect the identity of the reporter? Yes
Medical Advisory Board
Role of the MAB Review the medical report and make a determination as to the status of the driving privileges of the
driver. Decision of the MAB implemented by the Secretary of State.
Medical Review contact
information
Supervisor, Medical Review Unit
Office of the Secretary of State
Driver Services Department
2701 South Dirksen Parkway
Springfield, IL 62723
217-785-3002
90
Name of State & DMV
contact information
Indiana Bureau of Motor Vehicles
Medical Section
Indiana Government Center North
100 N Senate Avenue. Room N402
Indianapolis, IN 46204
www.mybmv.IN.gov
317-233-6000
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40 minimum each eye without
restrictions. 20/50 each eye with
correction = glasses/contacts restric-
tion required unless vision referral
presented with approval from Medical
Advisory Board specifying that cor-
rective lenses will not improve acuity.
Indiana tests each eye individually
One eye 20/40 other eye 20/50
through blind without correction =
outside rearview mirrors restriction.
One eye 20/40 other eye 20/50
through blind with correction =
glasses/contacts, outside rearview
mirrors restriction.
One eye 20/50 other eye 20/70
through blind with correction =
glasses/contacts, outside rearview
mirrors and daylight driving only
restrictions.
The absolute minimum visual acuity
obtained by a customer service rep-
resentative in order to issue a license
is 20/70 in each eye with correction
= glasses/contacts, outside rearview
mirrors and daylight driving only
restrictions for licensing. The BMV will
license an individual with less acuity
upon the recommendation of the
Medical Advisory Board.
Yes, for acuity as low as 20/200
if 20/40 can be achieved with
telescope = restrictions apply
Visual fields Minimum field requirement .........................................................N/A for standard license renewal,
70° one eye, 120° both eyes
(when required)
Color vision Is there a color vision requirement? .............................................N/A for standard renewal
Road test Type of road test ........................................................................Standardized road tests are
administered by State examiners
Special/courtesy drives tests
(extended) are administered
by a State senior examiner
Restricted licenses A variety of restrictions are available—most common restriction is for corrective lenses
Indiana
* Testing (visual, written or skills) to obtain a 4-year commercial driver license is more stringent per Federal guidelines than for renewal
of a standard operator license as stated here.
91
Indiana (continued)
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
Standard length of license validation
Operator License
June 7th 2007–Dec. 31st 2007:
5 years
Jan. 1st 2008–Dec. 31st 2008:
4 years
Jan. 1st 2009: 6 years
In person
Yes (acuity)
Yes, if new to State, if 6 or more
points appear on the driving record,
if expired more than 2 years or
recommended by the Medical
Advisory Board.
Yes, if new from out of country, if out
of State license is expired more than
1 year, if Indiana license is expired
more than 3 years or in the event the
bureau receives evidence of driving
impairment
Age-based renewal procedures Licenses issued to individuals under the age of 18 expire at midnight on the individuals’ 21st birthday.
Age 75–84, renewal cycle is reduced to 3 years
Age 84 +, renewal cycle is reduced to 2 years.
Reporting Procedures
Mandatory medical reporting None
Physician/medical reporting Drivers should self-report medical conditions that may cause lapse of consciousness, seizure, etc.
Physicians are encouraged but not required to report to the bureau a patient who may have a medical
condition that would adversely affect their ability to operate a motor vehicle safely.
Immunity A physician licensed to practice medicine under IC 25-22.5, an optometrist licensed to practice
optometry under IC 25-24, or an advanced practice nurse licensed under IC 25-23 who has personally
examined the patient not more than thirty (30) days before making a report concerning the patient’s
fitness to operate a motor vehicle is not civilly or criminally liable for a report made in good faith to the:
(1) bureau;
(2) commission; or
(3) driver licensing medical advisory board;
concerning the fitness of a patient of the physician, optometrist, or advanced practice nurse to operate
a motor vehicle in a manner that does not jeopardize the safety of individuals or property.
Legal protection Applicable immunity law only.
DMV follow-up Written notification.
Other reporting Will accept information from courts, law enforcement, family members and other reliable sources
Anonymity The BMV protects the identity of the reporter, unless information is required by a court of law
Medical Advisory Board
Role of the MAB MAB advises the Bureau of Motor Vehicles on medical issues regarding individual drivers. Actions are
based on the recommendation of the majority and/or specialist.
Medical Review contact information Referrals can be faxed to 317-233-3138. Questions should be directed to 317-232-0901
92
Name of State & DMV
contact information
Iowa Department of Motor Vehicles
IA DOT, Park Fair Mall
100 Euclid Avenue, PO Box 9204
Des Moines, IA 50306-9204
www.dot.state.ia.us/mvd/
515-237-3201
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
20/40
20/50 daylight driving only, 20/70
in better eye restricted license for
daylight only up to 35 mph; 20/100
recommendation from vision special-
ist, if worse—recommendation from
MAB; absolute minimum 20/200
No
Visual fields Minimum field requirement .........................................................140° both eyes. With outside mirrors
70°T + 45° N one eye, 115° both
eyes. If less than 95° both eyes and
60°T+35°N one eye need MAB
recommendation
Color vision Is there a color vision requirement? .............................................No
Road test Type of road test ........................................................................Non-fixed Course, general traffic
Restricted licenses Yes
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
2 or 4 years
In-person, extensions available if out
of State for 6 months.
No
No
Yes, If physical or mental condition
present
Age-based renewal procedures At age 70, renewal every 2 years.
Reporting Procedures
Mandatory medical reporting No
Physician/medical reporting A physician may report to the department of motor vehicles “the identity of a person who has been di-
agnosed as having a physical or mental condition which would render the person physically or mentally
incompetent to operate a motor vehicle in a safe manner.
Immunity Yes
Legal protection Yes—321.186 A physician or optometrist making a report shall be immune from any liability, civil or
criminal, which might otherwise be incurred or imposed as a result of the report
DMV follow-up Driver notified in writing of referral. License suspended upon referral.
Other reporting Will accept information from courts, other DMVs, police and family members.
Anonymity Not confidential
Medical Advisory Board
Role of the MAB To review medical/vision reports as requested and advise of their recommendation to a person’s capa-
bility to drive safely.
Medical Review contact
information
Iowa Department of Transportation Des Moines, IA 50306-9204
Office of Driver Services Phone 800-532-1121
PO Box 9204
Iowa
93
Name of State & DMV
contact information
Kansas Division of Motor Vehicles, Driver Control
Docking State Office Building
915 SW Harrison Street 1st Floor
Topeka, Kansas 66625
www.ksrevenue.org/dmvdrlic.htm
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
20/40
20/40 better eye unrestricted, 20/60
better eye with doctor report, worse
than 20/60 must demonstrate ability
to operate a vehicle and safe driving
record for 3 years.
Yes, with eye doctor’s report.
Visual fields Minimum field requirement ......................................................... Worse than 110° with both eyes and
55° monocular
Color vision requirement None
Type of road test Non-fixed course
Restricted licenses Up to 4 restrictions can be added, at doctors/examiners discretion. These can include: corrective
lenses, daylight only, no interstate driving, outside business area, within city limits, mileage restriction
in increments of 5 mi. up to 30, outside mirror, mechanical aid, automatic transmission, prosthetic aid,
licensed driver in front seat.
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
6 years
In person
Yes
Yes
Yes, by examiner challenge or for visual
acuity, or at medical doctor request.
Age-based renewal procedures At age 65, renewal every 4 years. There is no age-based road test.
Reporting Procedures
Mandatory medical reporting No, statutes specify that physicians may not be required to volunteer information to the division or to the
medical advisory board concerning the mental or physical condition of any patient
Physician/medical reporting N/A
Immunity Yes, people reporting in good faith are statutorily immunized from civil actions for damages caused by
such reporting.
Legal protection Patient has to sign a form to show it is ok for M.D. or O.D. to release information to DMV.
DMV follow-up Driver is notified in writing of referral.
Other reporting Will accept information from courts, other DMVs, police and family members, concerned citizens.
Letters must be signed.
Anonymity Yes. Letters of concern are confidential.
Medical Advisory Board
Role of the MAB To help Director of Vehicles and Driver Review interpret conflicting information or action based on
recommendation of specialists. Determine eligibility of hardest or borderline cases.
Medical Review contact information Kansas Driver Review, Medical Advisory Board
915 SW Harrison Room 162 | Topeka, KS 66626
785-296-3601
Kansas
94
Name of State & DMV
contact information
Kentucky Division of Driver Licensing
200 Mero Street
Frankfort, KY 40622
www.kytc.state.ky.us/drlic
502-564-0280
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/60
20/60
20/60
20/60 with corrective lenses
Yes, with distance acuity of 20/60
or better using a bioptic telescopic
device. KRS 186.578(1)c.
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
Binocular horizontal field of vision of
at least 35 degrees to the left and
right side of fixation and a binocular
vertical field of vision of at least 25
degrees above and below fixation.
N/A
Color vision Is there a color vision requirement? .............................................No
Road test Medical Advisory Board may recommend further examination or investigative testing.
Restricted licenses Available
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
4 years
In person
No
No
No
Age-based renewal procedures None
Reporting Procedures
Mandatory medical reporting No
Physician/medical reporting No
Immunity Yes
Legal protection None
DMV follow-up Driver notified in writing of referral to medical advisory board.
Other reporting Will accept information from courts, other DMVs, family members and police.
Anonymity None
Medical Advisory Board
Role of the MAB The medical advisory board identifies drivers with physical or mental impairments that impede their
ability to safely operate a motor vehicle.
Medical Review contact
information
Questions regarding medical review can be directed to 502-564-0280 ext. 2174.
FAQs for medical review can be found at http://transportation.ky.gov/DrLic/mrb/MRB.htm
Kentucky
95
Name of State & DMV
contact information
Louisiana Office of Motor Vehicles
Drivers License Suspension Unit
PO Box 64886
Baton Rouge, LA 70896
www.expresslane.org
225-925-3929
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
20/40
20/40 in better eye unrestricted,
20/50-20/70 better eye with restric-
tions, 20/70-20/100 better eye with
possible restricted license. Less than
20/100 for better eye refer to MAB
No
Visual fields Minimum field requirement .........................................................No
Color vision Is there a color vision requirement? .............................................No
Restricted licenses Yes, daytime only, weather restrictions, radius limitation, no interstate driving
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
4 years
In person or mail in every other cycle,
Internet, interactive voice response,
unless license expired 6 months or
more.
Yes
Yes, if expired one year or more
Yes, if expired 2 years or more
Age-based renewal procedures No renewal by mail for drivers over the age of 70
Reporting Procedures
Mandatory medical reporting No, there is no statutory provision requiring physicians to report patients
Physician/medical reporting N/A
Immunity Yes, a physician who provides such information has statutory immunity from civil or criminal liability
for damages arising out of an accident.
Legal protection Louisiana has statutory protection for good faith reporting of unsafe drivers.
DMV follow-up Driver is notified in writing of referral.
Other reporting DMV employee or agent in performance of duties, law enforcement officer, health care provider,
or family member
Anonymity An order from a court of competent jurisdiction required before identity of reporter can be released.
Medical Advisory Board
Role of the MAB The medical advisory board identifies drivers with physical or mental impairments that impede their
ability to safely operate a motor vehicle.
Medical Review contact
information
Questions regarding medical review can be directed to 502-564-0280 ext. 2174.
FAQs for medical review can be found at http://transportation.ky.gov/DrLic/mrb/MRB.htm
Louisiana
96
Name of State & DMV
contact information
Maine Bureau of Motor Vehicles
Attn: Medical Unit
29 State House Station
Augusta, ME 04333-0029
www.state.me.us/sos/bmv
209-624-9000
Licensing Requirements
Visual acuity Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
20/70 with restrictions
No
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
110° both eyes-Class D only
Keystone View
Color vision requirement None
Type of road test Assesses general driving skills
Restricted licenses Yes: daytime only, radius from home, special equipment
License Renewal Procedures
Standard Length of license validation.........................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
6 years
At age 40, 52, 65 and every 4 years
thereafter
No
No
Age-based renewal procedures At age 65, renew every 4 years.
Reporting Procedures
Mandatory medical reporting Yes
Physician/medical reporting Yes
Immunity Yes
Legal protection Yes
DMV follow-up Requires a medical evaluation form to be completed by a physician at periodic intervals
Other reporting Will accept information from courts, other DMVs, police, family members and other resources
Anonymity Yes, but identity may be revealed at an administrative hearing if requested.
Medical Advisory Board
Role of the MAB The Medical Advisory Board reviews the medical information submitted whenever a person contests a
Division action. Reports received or made by the Board are confidential and may not be disclosed unless
the individual gives written permission
Medical Review contact information The Medical Review Coordinator can be reached at 207-624-9101
Maine

97
Name of State & DMV
contact information
Maryland Motor Vehicle Administration
6601 Ritchie Highway, NE
Glen Burnie, MD 21062
www.marylandmva.com
301-729-4550 or
800-950-1682
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
If one eye blind—other with correction ........................................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
20/40
20/40
20/70 in better eye for restricted;
20/70-20/100 requires special
permission from MAB.
Yes: daytime only, outside mirrors
20/70 through telescope. 20/100
through carrier lens.
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
Continuous field of vision at least
140E in each eye unrestricted; 70°
(+/- 35°)/110°
Stereo Optical Optec 1000
vision screener
Color vision requirement Only for commercial drivers
Type of road test N/A
Restricted licenses Yes: daytime only, outside mirrors for low vision drivers
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
5 year
In-person
Yes (binocular, acuity, peripheral)
No
No
Age-based renewal procedures Are there any age-based license renewal procedures?
Reporting Procedures
Mandatory medical reporting No
Physician/medical reporting Maryland law provides for the discretionary reporting to the Motor Vehicle Administration of people who
have “disorders characterized by lapses of consciousness”
Immunity Yes, a civil or criminal action may not be brought against any person who makes a report to the Medical
Advisory Board and who does not violate any confidential or privileged relationship conferred by law.
Legal protection Action may not be brought against any person who makes a report to the Medical Advisory Board and
does not violate any confidential or privileged relationship conferred by law.
DMV follow-up Driver is notified in writing of referral. License is suspended and further examination is required.
Other reporting Will accept information from court, other DMVs, police, family members and other resources.
Anonymity Yes, if requested
Medical Advisory Board
Role of the MAB The MAB advises the Motor Vehicle Administration regarding medical review for fitness to drive through
its Division of Driver Wellness and Safety.
Medical Review contact information Manager, Driver Wellness & Safety Division, Maryland Motor Vehicle Administration
6601 Ritchie Highway, NE | Glen Burnie, MD 21062
410-424-3644; Fax: 410-768-7627
Maryland
98
Name of State & DMV
contact information
Massachusetts Medical Affairs
PO Box 199100
Boston, MA 02119
www.state.ma.us/rmv/index.htm
617-351-9222
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
N/A
20/40 better eye unrestricted; 20/50-
2070 in better eye results in daylight
only restriction.
Yes. As long as 1) The peripheral
vision is at least 120; 2) Vision is
corrected to 20/40 through the biop-
tic and 20/100 through the carrier
lens. Also, must have at least 20/100
in the other eye. The bioptic must
meet certain requirements: it must
be monocular, fixed focus, no greater
than 3X magnification, and must be
an “integral part of the lens”
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
120°
Optec 1000 Vision Testing Machine
Color vision requirement Yes—distinguish red, green and amber
Type of road test N/A
Restricted licenses Yes: daytime only
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
5 Years
In person, or via Internet.
Yes
No; however DMV reviews on
case-by-case basis and if indicated
will administer test.
No; however DMV reviews on
case-by-case basis and if indicated
will administer test.
Age-based renewal procedures None
Reporting Procedures
Mandatory medical reporting No, MA is a self-reporting State, meaning it is the responsibility of the driver to report to the RMV any
medical condition that may impair driving ability.
Physician/medical reporting Yes, physicians are encouraged to report unfit drivers to the RMV.
Immunity No, the law does not provide any protection from liability, nor does it promise confidentiality due to
“Public Records” law which states simply that a driver is entitled to any information upon receipt of
written approval.
Legal protection No, see “Immunity”
Massachusettes
99
Massachusettes (continued)
DMV follow-up If report comes from family or member of public it must be in writing and signed. If report is accepted,
then driver contacted by mail and asked to obtain medical clearance to certify that he/she is safe to
drive. If DMV does not receive a response within 30 days a second request is mailed. If still no re-
sponse, a license revoked.
If report is from law enforcement or physician, it is considered “immediate threat.” Driver is contacted
by mail and requested to voluntarily surrender license or submit medical clearance within 10 days.
If no response, license revoked.
Other reporting Will accept information from court, other DMVs, police, family members and other resources.
Anonymity No, see “Immunity”
Medical Advisory Board
Role of the MAB The purpose is to provide guidance to the Registry when a medical issue has been raised regarding the
ability of applicants for learner’s permits and licenses to operate a motor vehicle and for those whose
privileges to operate a motor vehicle has been (or should be) restricted, suspended or revoked. One of
our goals in consulting with the MAB on matters requiring medical expertise is to bring consistency to
these decision making processes.
Medical Review contact
information
Registry of Motor Vehicles
Director of Medical Affairs
PO Box 55889
Boston, MA 02205-5889
Attn: Director of Medical Affairs
Fax: 617-351-9223
100
Name of State & DMV
contact information
Michigan Department of State
Driver Assessment and Appeal Unit
PO Box 30196
Lansing, MI 48909-7696
www.michigan.gov/sos
517-335-7051 phone
517-335-2189 fax
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40 to and including 20/50
20/50
Minimum of 20/70 in better eye
with no progressive abnormalities
of the eye, daylight only restriction;
Minimum of 20/60 in better eye if
progressive abnormalities or disease
of the eye, daylight only restriction.
Yes, will require a road test for all
first-time users.
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
110°-140° both eyes; less than 110°
to/including 90° additional condi-
tions and requirements; less than 90
degrees, no driving allowed.
Optic 1000 DMV Vision Tester
Color vision requirement No
Type of road test Standardized course and requirements with various locations throughout the State
Restricted licenses Yes. Restrictions are based on review of medical input and reexamination testing. Examples include
radius driving, daylight only driving, no expressway driving.
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
4 years
Mail in every other cycle, if free of
convictions
Yes
No. A written test is not required
at the time of renewal. It may be
required at driver assessment re-
examinations and to obtain an
original license.
Yes, if license expired more than
4 years.
Age-based renewal procedures No
Reporting Procedures
Mandatory medical reporting No
Physician/medical reporting Physicians are encouraged to report unsafe drivers to the Department of State for evaluation.
Immunity No
Legal protection No
DMV follow-up The driver is notified in writing of the request for evaluation. The Department may require the driver to
submit updated medical information and to appear for reexamination and testing. The testing includes a
vision screening, written exam, and on-road driving evaluation.
Other reporting The Department accepts requests for driver evaluation from family, police, public officials and any other
concerned persons who have knowledge of a driver’s inability to drive safely or health concerns that
may affect his/her driving ability.
Michigan
101
Michigan (continued)
Anonymity The Department of State cannot accept anonymous requests for driver evaluation. The requestor must
include his/her name, address, daytime phone number and signature. The Department would protect
the identity of the author of the request for driver evaluation to the extent allowed by law.
Medical Advisory Board
Role of the MAB Current medical reviews are based on recommendation of specialist. The Department of State is in the
process of reestablishing a Medical Advisory Board. The Department intends for the MAB to review
current Department medical review processes and establish updated guidelines for the medical review
of Michigan drivers.
Medical Review contact
information
Driver Assessment and Appeal Division can be reached at 517-335-7051.

102
Name of State & DMV
contact information
Minnesota Medical Unit
445 Minnesota Street, Suite 170
Town Square Building
St. Paul, MN 55101-5170
www.dps.state.mn.us/dvs/index.html
651-296-2021
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
20/40
20/70 in better eye with speed
limitations, 20/80 referred to a
driver evaluation unit; 20/100 denied
license
No
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
105° unrestricted
Yes, at renewal
Color vision requirement No
Type of road test 20/80, special test with driver exam supervisor
Restricted licenses Yes: daytime, area restriction, speed, no freeway
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
4 years
In person
Yes
Only if driver license expired more
than 1 year
If driver license is expired more than
5 years
Age-based renewal procedures None
Reporting Procedures
Mandatory medical reporting No
Physician/medical reporting Physician reporting is encouraged
Immunity Yes
Legal protection Not addressed in driver licensing laws
DMV follow-up Driver is notified in writing of referral. License is suspended upon referral and further examination is
conducted.
Other reporting Will accept information from court, other DMVs, police, family members and other resources.
Anonymity Yes, unless court subpoenas record
Medical Advisory Board
Role of the MAB Action is based on recommendation of majority.
Medical Review contact
information
Minnesota Department of Public Safety
Medical Unit
445 Minnesota Street, Suite 170
St. Paul, MN 55101-5170
651-296-2021
Minnesota
103
Name of State & DMV
contact information
Mississippi Driver Improvement
PO Box 958
Jackson, MS 39205
www.dps.state.ms.us
601-987-1231
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
20/70 daytime
Yes, 20/70 with telescope
Visual fields Minimum field requirement ......................................................... 140° unrestricted; one eye T 70°; N
35° with 2 outside mirrors
Color vision requirement No
Type of road test
Restricted licenses Yes
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
4 years
In person
No
No
No (an exception can be made if
examiner feels testing is warranted)
Age-based renewal procedures Those 71 and older are not allowed to do on-line renewal.
Reporting Procedures
Mandatory medical reporting No
Physician/medical reporting
Immunity No
Legal protection
DMV follow-up Patient is called into DMV office for road and vision test when they receive a report from any source.
Other reporting Will accept information from court, other DMVs, police and family members.
Anonymity Yes, granted for all reporters.
Medical Advisory Board
Role of the MAB In situations where the DMV is unsure, cases are reviewed by an external medical panel convened by
the State medical board.
Medical Review contact
information
The medical board can be reached at 601-853-6733
Questions about referrals to the DMV should go to 601-987-1231
Mississippi
104
Name of State & DMV
contact information
Missouri Drivers License Bureau
Attn: Medical Review
PO Box 200
Jefferson City, MO 65105
http://dor.mo.gov/mvdl/drivers/
573-751-2730
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
20/50
20/160 for restricted
Not for meeting vision requirements
but can be used for skills tests and
while driving
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
55° or better in both eyes; 85° in one
eye with restrictions
Objective/Quantitative
Color vision requirement No
Restricted licenses Yes. As long as they meet the vision requirements, we have restrictions for equipment, speed,
radius, (location of driving) time of day and/or length of time driving. Virtually any restriction a doctor
or examiner recommends.
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
6 years
In person, or renewal by mail if out
of State.
Yes
Only if license is expired for more
than 6 months (184 days) or if an
individual is cited and after the review
process a written test could be
required.
See written test requirement above.
Age-based renewal procedures At age 70, reduction in renewal cycle to 3 years. Also, any school bus driver 70 or older must renew
their School Bus Permit annually. Below 70, renewal is every 3 years.
Reporting Procedures
Mandatory medical reporting Not mandatory but encouraged for any condition that could impair or limit a person’s driving ability.
A form is available (form 1528, Physician’s Statement) but not required. Forms are available at the
Department of Revenue, P.O. Box 200 Jefferson City, Mo 65105-0200. Attention Medical Review.
Physician/medical reporting Medical professionals will not be prevented from making a report because of their physician-patient
relationships 302.291.
Immunity Yes, an individual is immune from civil liability when they have made a report in good faith.
Legal protection See Physician Reporting Laws above.
DMV follow-up Depending on the information received, we may ask for additional information, add restrictions, require a
written exam, skills test, vision exam, physical exam or deny the privilege.
Other reporting Will accept information from court, DMV clerks, peace officers, social workers and family members
within three degrees of consanguinity.
Anonymity Yes
Missouri
105
Missouri (continued)
Medical Advisory Board
Role of the MAB The Medical Advisory Board evaluates each case on an individual basis. The medical information
is reviewed by staff personnel of the Driver’s License Bureau. The MAB relies on the person’s
physician’s opinion on whether the applicant or licensee can drive safely. Action is based on
recommendation of majority.
Medical Review contact information Attention Medical Review
Department of Revenue
P.O. Box 200
Jefferson City, Mo 65105-0200
573-751-2730
Fax: 573-522-8174
http://dor.mo.gov/mvdl/drivers/faq/doctor.htm
106
Name of State & DMV
contact information
Montana Motor Vehicles Division
Medical Unit
PO Box 201430
Helena, MT 59620-1430
www.doj.mt.gov/driving/default.asp
406-444-4536
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
20/40
20/70 in better eye with restrictions
on daylight and speed; 20/100 in
better eye, with possible restricted
license.
Yes, 20/100 through carrier lens
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
Only for commercial drivers
Optic 1000
Color vision requirement Commercial only
Type of road test Figure-8, 3 left and 3 right turns, 2 stop signs, through intersection and parallel parking.
Restricted licenses Yes
License Renewal Procedures
Standard Length of license validation.........................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
8 years; if renewing by mail a 4 year
license is issued—next renewal
requires a personal appearance by
the applicant. Commercial licenses
are now only good for 5 years.
Yes
Discretion of examiner if safe
operation of the motor vehicle is in
question.
Same as written requirement
Age-based renewal procedures For ages 68 to 74, renewal cycle reduced to 1–6 years. At age 75, renewal cycle is reduced to 4 years.
Reporting Procedures
Mandatory medical reporting No
Physician/medical reporting Physicians are encouraged to report
Immunity Yes, There is a statute giving the physician immunity from liability for reporting in good faith any patient
whom the physician diagnoses as having a condition that will significantly impair the patient’s ability to
safely operate a motor vehicle. No action may be brought against a physician for not making such a report.
Other reporting Will accept information from court, other DMVs, police, family members, and other resources.
Anonymity State is required to tell person who reported them, if asked.
Medical Advisory Board
Role of the MAB Montana does not have a Medical Advisory Board
Medical Review contact information Supervisor
Records and Control Bureau
303 North Roberts
Helena, Montana 59620
Montana
107
Name of State & DMV
contact information
Nebraska Department of Motor Vehicles
Driver License Examining Division
PO Box 94726
Lincoln, NE 68509
www.dmv.state.ne.us
402-471-3861
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
20/40
20/70, the other eye not blind;
17 restrictions are used, depending
on vision in each eye
Yes, 20/70 minimum through
telescope
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
Less than 100° denied, 140° both eyes
Vision Machine
Color vision requirement Commercial only
Type of road test On the road test that includes requirements such as emergency stop, right turns, left turns, etc.
Restricted licenses Yes, Nebraska offers restricted licenses.
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
5 years
Must apply in person before a driver
license employee. Individuals who re-
side out-of-state during their renewal
time may renew via mail.
Yes
Only if license is expired over 1 year
or license is suspended, revoked or
cancelled.
Only if license is expired over 1 year
or license is suspended, revoked or
cancelled.
Age-based renewal procedures No. Nebraska does not have age-based renewal regulations.
Reporting Procedures
Mandatory medical reporting No
Physician/medical reporting Yes, encouraged but not required.
Immunity No
Legal protection No
DMV Follow-up Drivers are notified by certified mail that they must appear for retesting. Drivers are also required to bring
in a vision and medical statement that has been completed by their physicians within the last 90 days.
Other reporting Will accept information from law enforcement and other concerned parties.
Anonymity Yes, unless the driver appeals the denial or cancellation of their license to District Court.
Nebraska
108
Nebraska (continued)
Medical Advisory Board
Role of the MAB To provide advice to the Department concerning the physical a mental ability of an applicant or holder of
an operator’s license to operate a motor vehicle.
Medical Review contact information Driver’s License Administrator
Nebraska Department of Motor Vehicles
P.O. Box 94789,
301 Centennial Mall South
Lincoln, NE 68509
109
Name of State & DMV
contact information
Nevada Department of Motor Vehicles
Management Services and Programs Division
555 Write Way
Carson City, NV 89711
www.dmvnv.com
775-684-4717
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
20/40
20/50, other eye no worse than
20/60 daylight driving only.
Yes, 20/40 through telescope, 20/120
through carrier, 130 E visual field.
Visual fields Minimum field requirement ......................................................... Binocular 140° unrestricted
Binocular 110°-140° restricted
Color vision requirement None
Type of road test Yes, if the vision specialist’s report does not meet the 20/40 standard but within the minimum (restrict-
ed) acuity levels for licensing.
Restricted licenses Yes; daytime only
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
4 years
Mail-in or Internet every other cycle.
Yes
Only if license classification
has changed
Only if license classification
has changed
Age-based renewal procedures Vision test and medical report required to renew by mail at age 70.
Reporting Procedures
Mandatory medical reporting Yes. Physicians are required to report patients diagnosed with epilepsy or any seizure disorder or lapse
of consciousness
Physician/medical reporting Yes
Immunity Yes
Legal protection Yes
DMV follow-up Letters and suspensions
Other reporting Court, other DMVs, police and family members.
Anonymity Yes
Medical Advisory Board
Role of the MAB Advisory role to DMV. Developing medical and health standards. Advisory role regarding medical reports
submitted to determine the mental or physical condition of the applicant. The department has the
authority to have a Medical Advisory Board due to Nevada Administrative Code 483.380. However, due
to the cost, Nevada has been unable to have such an advisory board in place.
Medical Review contact information Questions about medical review can be directed to 775-684-4717.
Nevada
110
Name of State & DMV
contact information
New Hampshire Department of Motor Vehicles
Directors Office
10 Hazen Drive
Concord, NH 03305
www.state.nh.us/dmv
603-271-2371
Licensing Requirements
Visual acuity Vision in both eyes .....................................................................
Vision in one eye ........................................................................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/30
20/70, restricted to daytime only
Yes
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
No
Snellen Eye chart or Stereo Optical
Viewer
Color vision requirement No
Type of road test Yes, on road practical
Restricted licenses Yes, daytime only
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
4 years
In-person
Yes
No
No
Age-based renewal procedures No special requirements for age.
Reporting Procedures
Mandatory medical reporting No
Physician/medical reporting Physicians are encouraged to report
Immunity N/A
Legal protection No, as reporting is not a requirement
DMV follow-up Full re-examination and in some cases an administrative hearing
Other reporting Will accept information from court, other DMVs, police, and family members.
Anonymity Not confidential
Medical Advisory Board
Role of the MAB None
Medical Review contact
information
Department of Safety
Division of Motor Vehicles
Driver Licensing
23 Hazen Drive
Concord NH 03305
603-271-2371
New Hampshire
111
Name of State & DMV
contact information
New Jersey Division of Motor Vehicles
Medical Division
PO Box 173
Trenton, NJ 08666
www.njmvc.gov
609-292-4035
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/50
20/50
20/50
20/50
Yes, 20/50 through telescope
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
No
N/A
Color vision requirement Yes—new drivers (not cause for denial)
Type of road test Standardized
Restricted licenses Yes
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
4 years
In-person digitized photos were
implemented in 2003.
Only if recommended.
If recommended by examiner
If recommended by examiner
Age-based renewal procedures No
Reporting Procedures
Mandatory medical reporting Yes. Only for cases of recurrent loss of consciousness
Physician/medical reporting Physicians are required to report patients who experience convulsive, seizures, recurrent periods of
unconsciousness, impairment or loss or loss of motor coordination.
Immunity Yes
Legal protection No
DMV follow-up A medical review is generated. Results of the medical review may result in suspension of license; the
driver may request an appeal.
Other reporting Will accept information from police, family, other agencies, courts, and other concerned persons. MVC
will not generate a letter based on an anonymous letter.
Anonymity No
Medical Advisory Board
Role of the MAB New Jersey has forms for each type of medical condition that may be cause for concern. Form is com-
pleted by driver’s physician. In problem cases, then passed on to the Medical Advisory Board. MAB is a
multidisciplinary group of physicians who then make licensing recommendations based on information.
Medical Review contact
information
New Jersey Division of Motor Vehicles
609-292-7500 ext. 5032
Medical Division
PO Box 173
Trenton, NJ 08666
New Jersey
112
Name of State & DMV
contact information
New Mexico Motor Vehicles Division
Driver Services, Attn: Medical
PO Box 1028
Santa Fe, NM 87504-1028
www.state.nm.us/
505-827-2296
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
20/40
20/80 better eye with restrictions
No
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
120°E, 30° in nasal field of one eye
Normal Ophthalmic Procedures
Color vision requirement No
Type of road test
Restricted licenses Yes
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
4 or 8 years
Yes
May be required
May be required
Age-based renewal procedures Drivers may not apply for 8-year renewal, if they turn 75 during the last 4 years of the 8-year period.
Becomes 1-year renewal after age 75.
Reporting Procedures
Mandatory medical reporting No
Physician/medical reporting Yes
Immunity Yes
Legal protection No
DMV follow-up By notice, drivers are informed that their licenses will be cancelled in 30 days unless they provide a
medical report clearing them to drive. If they do not provide reports, their licenses are cancelled.
Other reporting Will accept information from court, other DMVs, police, and family members.
Anonymity Not confidential
Medical Advisory Board
Role of the MAB Periodic medical updates required by drivers with certain medical conditions including epilepsy,
diabetes, and certain heart conditions. The DMV learns of an individual’s condition through questions
asked on the application
Medical Review contact information New Mexico MVD Driver Services Bureau can be reached at 505-827-2296.
New Mexico
113
Name of State & DMV
contact information
New York Department of Motor Vehicles
Attn: Driver Improvement Bureau
6 Empire State Plaza
Albany, NY 12228
www.nydmv.state.ny.us
518-474-0841
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
20/40
For applicants with visual acuity less
than 20/40 but not less than 20/70,
can complete form MV-80L and
submit for licensing consideration.
Yes
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
20/40-20/70 best corrected requires
140 E horizontal visual fields; 20/80-
20/1000 best corrected requires
minimum 140 E horizontal visual field
plus 20/40 through bioptic telescope
lens
Eye chart
Color vision requirement No
Type of road test Standard road test, includes basic maneuvers needed for everyday driving.
Restricted licenses Yes: daytime only, radius from home, annual vision update
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
8 years
Mail or in person
Yes
No
No
Age-based renewal procedures No
Reporting Procedures
Mandatory medical reporting No
Physician/medical reporting No
Immunity No
Legal protection N/A
DMV follow-up If a physician reports a condition that can affect the driving skills of a patient, the DMV can suspend the
driver license. The DMV suspends the driver license until a physician provides a certification that the
condition has been treated or controlled and does not affect driving skills If the DMV receives a report
from a source who is not a physician the DMV decides each case separately.
Other reporting Will accept information from court, other DMVs, police, family members and other resources.
Letters must be signed.
Anonymity If a person in a professional or official position (i.e., physician), the DMV does disclose the name of the
person who sent the report however if the reporter does not fall under this category, under the Freedom
of Information Law, the identity is protected.
New York
114
New York (continued)
Medical Advisory Board
Role of the MAB The medical advisory board advises the commissioner on medical criteria and vision standards for the
licensing of drivers.
Medical Review contact information Referrals for reexamination must be made in writing to:
New York State
Department of Motor Vehicles
Medical Review Unit Room 220
6 Empire State Plaza
Albany, NY 12228-0220
Information about the forms and procedures can be found at
www.nydmv.state.ny.us/license.htm#drivermed
115
North Carolina
Name of State & DMV
contact information
North Carolina Division of Motor Vehicles
Driver License Medical Division
1100 New Bern Ave.
Raleigh, NC 27697
www.dmv.dot.state.nc.us
919-861-3809
Licensing Requirements
Visual acuity Each eye without correction ........................................................
Both eyes without correction .......................................................
Each eye with correction.............................................................
Both eyes with correction ...........................................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
20/50
20/50
20/30 or better
20/100; 20/70 if one eye blind
No. However, there is a medical
appeal process if requested.
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
60° in one eye (30° on each side
Keystone; Stereo Optic 1000
Color vision requirement No
Type of road test Standardized road test, certain tasks must be completed to pass.
Restricted licenses Yes: daytime, speed restrictions, no interstate driving.
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
5 years
In person
Yes
Yes
No
Age-based renewal procedures 60+ are not required to parallel park on road test.
Reporting Procedures
Mandatory medical reporting No
Physician/medical reporting Physicians are encouraged to report unsafe drivers.
Immunity Yes, North Carolina statutes protect the physician who reports an unsafe driver.
Legal protection No
DMV follow-up Driver is notified in writing of referral.
Other reporting Will accept information from court, other DMVs, police, family members, and other resources, as long as
they are signed.
Anonymity No, however must request records in writing.
Medical Advisory Board
Role of the MAB Action is based on majority and/or opinion of specialist. Medical physicians review all medical
information that is submitted to the DMV. If more information is necessary, can issue a request.
Board decides what action should be taken. This action can be appealed.
Medical Review contact information Medical Review Unit
3112 Mail Service Center
Raleigh, NC 27697
Fax 919-733-9569
116
Name of State & DMV
contact information
North Dakota Department of Transportation
Drivers License and Traffic Safety Division
Attn: Chief Examiner
608 East Boulevard Avenue
Bismarck, ND 58505
www.dot.nd.gov/
701-328-2601
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
20/40
20/80 better eye if 20/100 in other
eye
Yes: 20/130 in carrier, 20/40 in
telescope, full peripheral field
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
Both eyes 105°
OPTEC 1000 Vision Tester
Color vision requirement No
Type of road test N/A
Restricted licenses Yes: daytime, pending a sight-related road test, area and distance restriction
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
4 years
N/A
Yes
No
No
Age-based renewal procedures No
Reporting Procedures
Mandatory medical reporting No, physicians may report. Submit letter to the Drivers License and Traffic Safety Division
Physician/medical reporting There is a law giving physicians permission to report to the ND Department of Transportation in writing,
the name, date of birth, and address of every patient over the age of 14 whom they have reasonable
cause to believe is incapable, due to physical or mental reason, of safely operating a motor vehicle
Immunity Yes, physicians who in good faith make a report or give an opinion or recommendation or participate in
any proceeding pursuant to this law, are immune from liability.
Legal protection ND Century Code addresses medical advice provided by physicians.
DMV follow-up Vision and/or medical reports
Other reporting Will accept information from court, other DMVs, police and family members.
Anonymity No
Medical Advisory Board
Role of the MAB Action based on recommendation of majority and/or specialist. MAB is used when drafting
Administrative rules.
Medical Review contact information Drivers License and Traffic Safety Division staff can be reached at 701-328-2070
North Dakota
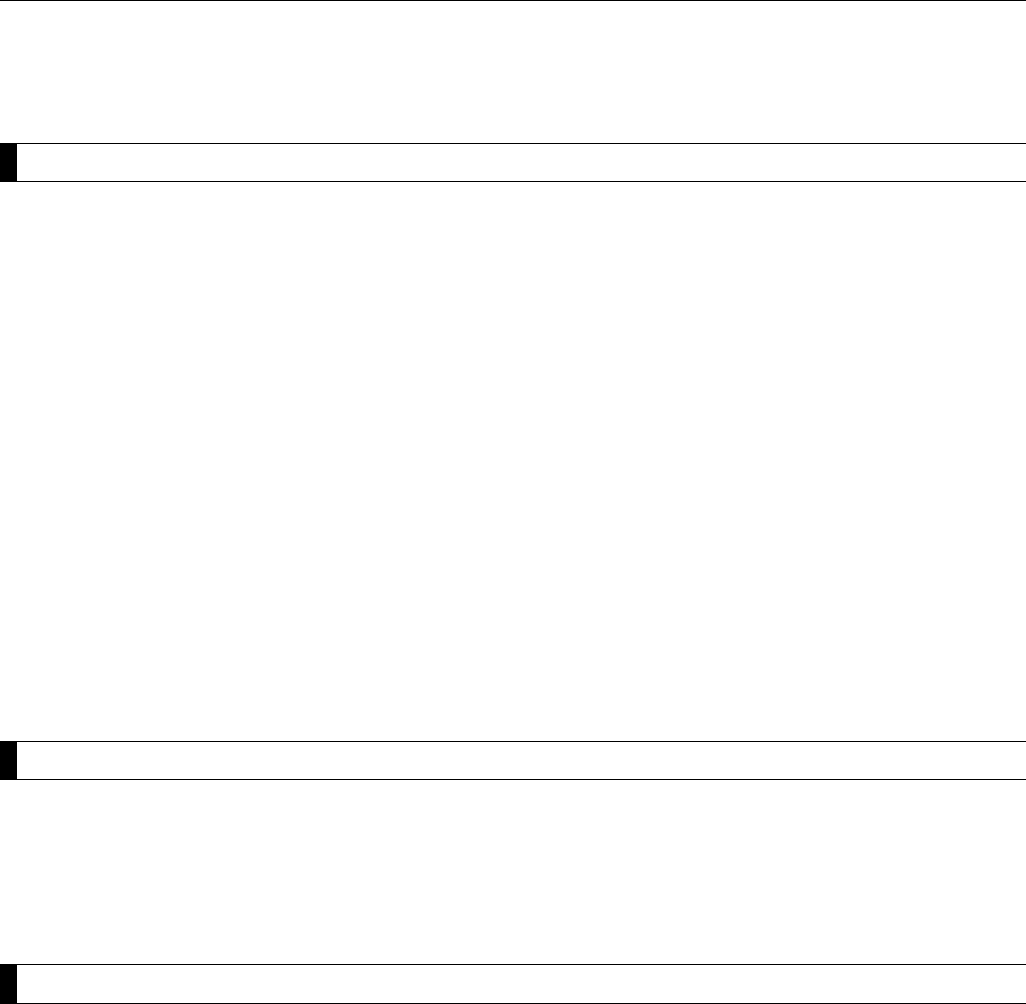
117
Name of State & DMV
contact information
Ohio Driver License Information Unit
Ohio Bureau of Motor Vehicles, Attn: Medical Unit
PO Box 16784
Columbus, OH 43216-6784
www.bmv.ohio.gov
614-752-7500
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Both eyes with/without correction when one eye is blind ...............
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/200 or better
20/40 or Better: Unrestricted Driving
20/50 – 20/70: Daylight Driving Only
Worse than 20/70: No Driving Privileges
Primary eye no worse than 20/200
Deficient eye: Worse than 20/300
20/30 or Better: Unrestricted Driving
20/40 – 20/60: Daylight Driving Only
Worse than 20/60: No Driving Privileges
20/70 through telescope, 20/200
through carrier lens.
Yes: 20/70 through telescope,
20/200 through carrier lens.
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
Each eye must have 70° temporal
reading
Keystone Vision II
Color vision requirement Yes
Type of road test Standardized course
Restricted licenses Right or left outside mirror restrictions for persons who are unable to obtain the required minimum
Temporal field requirement of 70 degrees in each eye but has a visual field of 70∞ Temporal and 45∞
nasal readings (mirror required on the side that does not have 70 ∞ Temporal). Persons with certain
medical or physical conditions may be required to furnish periodic medical statements or take periodic
drivers license examinations.
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
4 years
In person or renewal by mail only if
out of State.
Yes
No
No
Age-based renewal procedures No
Reporting Procedures
Mandatory medical reporting No
Physician/medical reporting No, however we will accept and take action on information submitted by a physician on an unsafe driver.
The doctor must agree to be our source of information and allow us to divulge this information to the driver.
Immunity No
Legal protection No
DMV follow-up Letter is sent requiring driver to submit a medical statement and/or take a driver license examination.
Driver is given 30 days to comply.
Other reporting Will accept information regarding unsafe drivers from courts, law enforcement agencies, hospitals,
rehabilitation facilities, family and friends. The person or facility making the report must agree to be our
source of information and allow us to divulge this information to the driver.
Anonymity Not confidential
Ohio
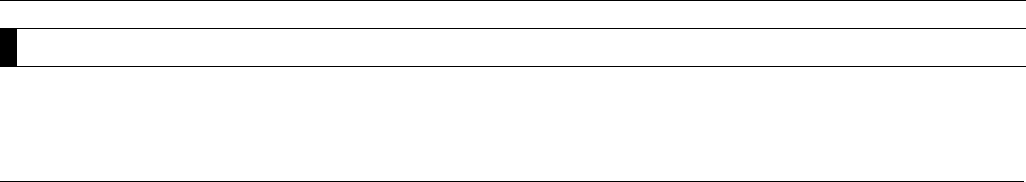
118
Ohio (continued)
Medical Advisory Board
Role of the MAB No medical advisory board. Ohio has a medical consultant to contact for assistance with difficult cases
or policy-making assistance.
Medical Review contact information Information on making referrals can be obtained through the contacts above.

119
Name of State & DMV
contact information
Oklahoma Driver Improvement Division Department
of Public Safety
Attn: Medical
PO Box 11415
Oklahoma City, OK 73136
www.dps.state.ok.us/dls/
405-425-2059
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/60
20/60
20/50
20/100 for better eye with
restrictions
Not permitted. Laws will not allow
for consideration of licensing or
restrictions.
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
Both eyes, 70° in the horizontal
meridian.
Yes
Color vision requirement No
Type of road test Non-fixed course
Restricted licenses Yes, physician recommendations such as daylight driving only, speed limitations, or local driving only
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
4 years
In-person
No
No
No
Age-based renewal procedures No
Reporting Procedures
Mandatory medical reporting No
Physician/medical reporting Yes, any physician participating in good faith and without malicious intent in making a report of an
unsafe driver shall have immunity from civil liability that might otherwise be incurred.
Immunity Yes
Legal protection By statute the physician has full immunity.
DMV follow-up Driver is notified in writing of referral, required to appear for an interview at the Department. Requires a
current medical evaluation from qualified practitioner as determined a full review examination.
Other reporting Will accept information from any verifiable source with direct knowledge of the medical condition that
would render the driver unsafe.
Anonymity No
Medical Advisory Board
Role of the MAB Action is based on the recommendation of the majority and/or specialist.
Medical Review contact information Department of Public Safety
Executive Medical Secretary
PO Box 11415
Oklahoma City, OK 73136
Oklahoma
120
Name of State & DMV
contact information
Oregon Department of Motor Vehicles
Attn: Driver Programs Section, Medical Program Coordinator
1905 Lana Avenue NE
Salem, OR 97314
www.oregon.gov/ODOT/DMV/ATRISK/index.shtml
503-945-5000
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
20/40
20/70 better eye with restrictions
Bioptic-telescopic lenses are not
permitted to meet acuity standards;
however, may be used while driving.
Must pass vision test with carrier
lens only.
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
110° in horizontal (one or both eyes
Both Keystone Driver Vision Screen-
ing System & OPTEC Vision Screening
Instruments are used.
Color vision requirement No
Type of road test Standardized course
Restricted licenses Yes. Daytime driving only for vision between 20/40 and 20/70
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
8 years
In person renewal. A “valid without
photograph” license may be issued if
the person is temporarily out of State
at the time of license renewal.
After age 50
No
No
Age-based renewal procedures After age 50, vision screening every 8 years.
Reporting Procedures
Mandatory medical reporting Oregon’s mandatory medical reporting system is not based solely on diagnosis or medical condition.
Physicians and health care providers meeting the definition of “primary care provider” are required to
report persons presenting functional and/or cognitive impairments that are severe and cannot be cor-
rected/controlled by surgery, medication, therapy or driving device or technique.
Physician/medical reporting ORS 807.710 addresses mandatory reporting by physicians and other health care providers.
Oregon also has a voluntary reporting system that can be utilized by physicians and other medical
providers. This reporting system is not required by law.
Immunity Under the mandatory reporting system, the law provides the primary care provider with immunity from
civil liability.
Legal protection By Oregon law, a report filed under the mandatory reporting system is confidential and may not be
admitted as evidence in any civil or criminal action.
Oregon
121
Oregon (continued)
DMV follow-up In most cases, drivers reported under the mandatory system have their driving privileges immediately
suspended. A driver may request the opportunity to demonstrate ability to safely operate a motor vehicle
via knowledge and drive tests. For cognitive impairments (and for specific functional impairments),
medical file and driving record is sent to the State Health Office for determination of whether or not it is
safe at this point in time.
The majority of reports received under the voluntary reporting system will not result in an immediate
suspension action. Instead, these drivers will be given 30–60 days to pass DMV tests and/or submit
medical information before a suspension action is taken.
Other reporting Under the voluntary system, DMV will accept information from court, other DMVs, law enforcement,
physicians, family members and other sources.
Anonymity Under the mandatory system, only the medical information being reported is confidential. Under the
voluntary system, DMV will make every attempt to hold the reporter’s name confidential if requested.
Medical Advisory Board
Role of the MAB Oregon does not have a Medical Advisory Board. DMV’s Medical Determination Officer reviews medical
cases and makes determination on an individual’s medical condition and ability to drive. Cases can be
referred to the Health Department for advice.
Medical Review contact information DMV-Driver Programs Section
503-945-5295
Attn: Medical Program Coordinator
1905 Lana Avenue NE
Salem, OR 97314
122
Name of State & DMV
contact information
Pennsylvania Department of Transportation
Attn: Medical Unit
PO Box 68682
Harrisburg, PA 17106
www.dmv.state.pa.us/centers/olderDriverCenter.shtml
717-787-9662
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
20/40
20/40 in better eye unrestricted, up
to 20/100 combined vision restricted
Not permitted to meet acuity stan-
dards; however, are permitted for
driving. Must pass vision test with
carrier lens only: 20/100.
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
120° both eyes
PENNDOT does not regulate the kind
of testing devise used to measure this
Color vision requirement No
Type of road test Standardized road test, same as those used for the first-time permit application drivers.
Restricted licenses Yes: daytime driving only, area restrictions, dual mirrors, class restriction—all vision related
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
4 years
Internet, mail, in-person
No
No
No
Age-based renewal procedures Drivers 65+ renew every 2 years instead of 4; all drivers 45+ requested to submit physical and vision
exam prior to renewing (random mailing of 1,650 per month)
Reporting Procedures
Mandatory medical reporting Any person qualified to make a medical diagnosis is required to report any patient they feel exhibits
unsafe driving behaviors.
Physician/medical reporting Required, “All physicians and other persons authorized to diagnose or treat disorders and disabilities
defined by the Medical Advisory Board shall report to PENNDOT in writing the full name, DOB, and ad-
dress of every person 15 years of age and older, diagnosed as having any specified disorder or disability
within 10 days.”
Immunity Yes—see 1518 (f)—“No civil or criminal action may be brought against any person or agency for
providing the information required under this system.”
Legal protection Yes
DMV follow-up PENNDOT then sends out appropriate correspondence to drivers asking them to have necessary forms
completed and/or test performed.
Other reporting Will accept information from court, other DMVs, police, emergency personnel, and family members/
neighbors/caregivers, so long as reports are signed with a way to confirm reporter facts.
Anonymity Yes
Pennsylvania
123
Pennsylvania (continued)
Medical Advisory Board
Role of the MAB The board advises PENNDOT and reviews regulations proposed by PENNDOT concerning physical and
mental criteria including vision standards relating to the licensing of drivers. It meets, typically, once
every 2 years or as needed.
Medical Review contact information Bureau of Driver Licensing
Driver Qualifications Section
PO Box 68682
Harrisburg, PA 17106-8682
717-787-9662
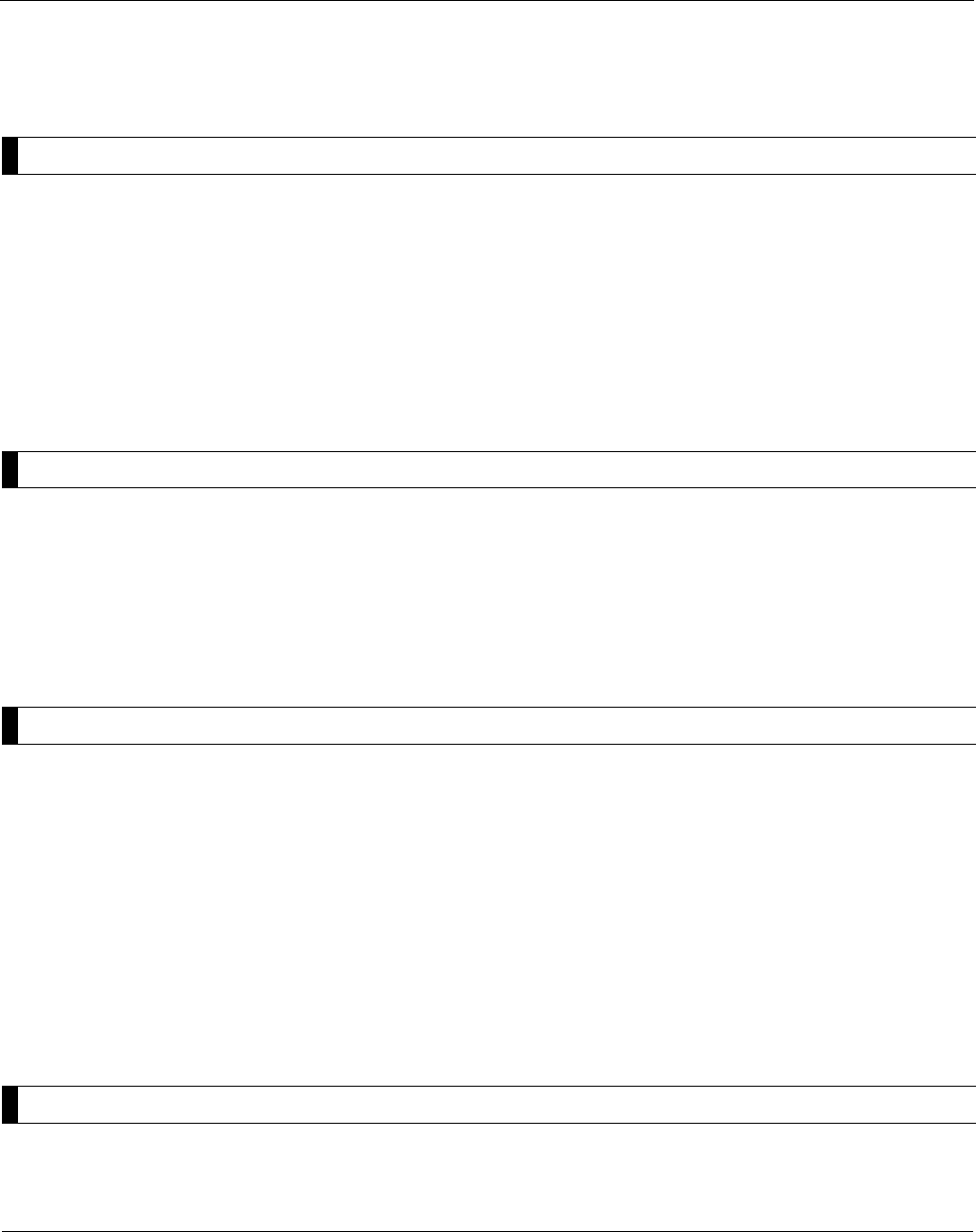
124
Name of State & DMV
contact information
Rhode Island Department of Motor Vehicles
Division of Motor Vehicles Services
286 Main Street
Pawtucket, RI 02860
www.dmv.state.ri.us/
401-588-3020
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
20/40
20/40 better eye.
Not mentioned in the regulations
Visual fields Minimum field requirement .........................................................115° in horizontal meridian, for one
eye 40° nasally
Color vision requirement No
Type of road test
Restricted licenses No
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
5 years
If license has been expired three
years or more, it cannot be renewed
Yes
No, only if license has been expired 3
years or more
No, only if license has been expired 3
years or more
Age-based renewal procedures Age 75, renewal cycle reduced to 2 years.
Reporting Procedures
Mandatory medical reporting No
Physician/medical reporting Yes, Any physician who diagnoses a physical or mental condition which in the physician’s judgment
will significantly impair the person’s ability to safely operate a motor vehicle may voluntarily report the
person’s name and other information relevant to the condition to the Medical Advisory Board within the
Registry of Motor Vehicles.
Immunity Yes, Any physician reporting in good faith and exercising due care shall have immunity from any liability,
civil or criminal, that otherwise might result by reason of his actions pursuant to the section. No cause
of action may be brought against any physician for not making a report pursuant to this section.
Legal protection
DMV follow-up Driver is notified in writing of referral.
Other reporting Will accept information from court, other DMVs, police, and family members.
Anonymity
Medical Advisory Board
Role of the MAB Action is based on the recommendation of the majority.
Medical Review contact information Information related to medical review can be obtained by calling 401-588-3020
Rhode Island
125
Name of State & DMV
contact information
Department of Motor Vehicles
PO Box 1498
Blythewood, SC 29016
www.scdmvonline.org
803-896-5000
Licensing Requirements
Visual acuity Each eye without correction ........................................................
Both eyes without correction .......................................................
Each eye with correction.............................................................
Both eyes with correction ...........................................................
If one eye blind—other without correction ...................................
If one eye blind—other with correction ........................................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
20/40
20/40
20/40
20/40—must have outside mirror
20/40 better eye unrestricted, 20/70
in better eye if worse eye is 20/200
or better; if not then 20/40.
Not permitted to meet acuity standard
(must meet acuity standard through
carrier lens); however, permitted to
use while driving.
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
No
Not specified.
Color vision requirement No
Type of road test Not specified.
Restricted licenses Yes: corrective lens, outside mirrors, daylight driving only
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
5 years
Renewal by mail if no violations in
past 2 years, no suspension, revoca-
tions or cancellations.
Only if 5+ points on record
Only if 5+ points on record
Only if there appears to be a need.
Age-based renewal procedures No
Reporting Procedures
Mandatory medical reporting No
Physician/medical reporting No
Immunity No
Legal protection N/A
DMV follow-up License is suspended upon referral and further examination is conducted.
Other reporting Will accept information from court, other DMVs, and police.
Anonymity N/A
Medical Advisory Board
Role of the MAB The Medical Advisory Board determines the mental of physical fitness of license applicants through a
medical evaluation process, and makes recommendations to the department’s director or designee on
the handling of impaired drivers.
Medical Review contact information South Carolina Driver Improvement Office
PO Box 1498
Columbia, SC 29216
803-896-9925
South Carolina
126
Name of State & DMV
contact information
South Dakota Driver Licensing
118 West Capitol Avenue
Pierre, SD 57501
www.state.sd.us/dps/dl
800-952-3696 or
605-773-6883
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
N/A
20/40
20/40
20/60 both eyes with/without
correction
Yes (skill test required)
Visual fields Minimum field requirement .........................................................No
Color vision requirement No
Type of road test Standardized course
Restricted licenses Yes: daylight only, outside rearview mirrors; corrective lenses, 50 mile radius from home, no driving
outside of town
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
5 years
In person; renewal by mail for military
and military dependents only.
Yes
No (unless expired more than 30 days)
No
Age-based renewal procedures No
Reporting Procedures
Mandatory medical reporting No
Physician/medical reporting Yes, physicians may report unsafe drivers if they so choose. The form to be used is a request
re-evaluation form. It can be found on our Web site or by calling our office.
Immunity No
DMV follow-up An appointment is scheduled and the driver is notified to appear for an interview, written and road test
may be included.
Other reporting Will accept information from court, other DMVs, police, family members, and other resources.
Anonymity No
Medical Advisory Board
Role of the MAB Medical information is reviewed by Department of Public Safety personnel. Upon having good cause
to believe that a licensed operator is not qualified to be licensed, may upon written notice of at least 5
days to the licensee, require him or her to submit to an examination or interview. The department shall
take action as may be appropriate and may withdraw/cancel the license of such person or permit him or
her to retain such license, or may issue a license subject to restrictions.
Medical Review contact information Information on making referrals can be obtained through the contacts above.
South Dakota
127
Name of State & DMV
contact information
Tennessee Department of Safety
Driver License Division
1150 Foster Avenue
Nashville, TN 37249-1000
http://state.tn.us/safety/driverservices.shtml
615-741-3954
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
20/40
20/40 better eye with/without
correction, minimum 20/60
each/both eye with restrictions
Yes, for 20/200 better eye, 20/60
through scope; visual field 150° or
larger, telescope no greater than 4X
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
For professional drivers only
Stereo Optic
Color vision requirement Yes, commercial only
Type of road test Standardized, certain requirements in course.
Restricted licenses Yes: with area limitations
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
5 years
Mail in every other cycle, by mail,
in person and by Internet
No
No (except in case of
hazardous material )
No
Age-based renewal procedures No
Reporting Procedures
Mandatory medical reporting No
Physician/medical reporting No
Immunity Yes
Legal protection No
DMV follow-up Driver is notified in writing of referral.
Other reporting Will accept information from court, other DMVs, police, family members, and other resources.
Anonymity No
Medical Advisory Board
Role of the MAB Paid physicians make recommendations upon review of medical report. Action is based upon recom-
mendation of the majority.
Medical Review contact information Driver Improvement Office can be reached at 615-251-5193
http://state.tn.us/safety/forms/medical.pdf
Tennessee

128
Name of State & DMV
contact information
Texas Department of Public Safety
Driver License Division
PO Box 4087
Austin, TX 78773-0001
www.txdps.state.tx.us/
512-424-2600
Licensing Requirements
Visual acuity Each/both eyes without correction ...............................................
Each/both eyes with correction ...................................................
If one eye blind—other without correction ...................................
If one eye blind—other with correction ........................................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/50
20/50 with eye specialist statement
20/50 with eye specialist statement
20/40 in better eye for unrestricted
license; 20/70 in better eye with
restrictions.
Yes, provided that the client has
acuity of 20/40 through the telescope
and passes road test.
Visual fields Minimum field requirement .........................................................None
Color vision requirement There is a requirement for all new drivers (not specified)
Type of road test Standardized Course
Restricted licenses Yes, restrictions applied per medical advisory direction (daytime only, speed limit <45 mph;
no expressway driving) Restrictions are based on medical advice and may include daytime driving
only where the speed limit <45 mph and no expressway driving.
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
6 years
In person; every second renewal
period may be eligible for alternate
renewal by Internet, telephone, or mail.
At in-person renewal
May be required based upon
evaluation of medical, physical,
or mental impairments.
May be required based upon
evaluation of medical, physical,
or mental impairments.
Age-based renewal procedures No. Effective 9/1/2007, drivers 79 or older must renew in person; renewal is required every 2 years for
drivers 85 or older.
Reporting Procedures
Physician/medical reporting Any physician licensed to practice medicine in Texas may inform the Department of Public Safety.
This release of information is an exception to the patient-physician privilege. There is no special
reporting form; a letter from the physician will suffice.
Immunity Yes
DMV follow-up The driver is notified in writing of the referral and required to provide medical information from his/her
personal physician.
Legal Protection Yes
Other reporting Will accept information from court, other DMVs, police, family members, and other resources.
Anonymity Not anonymous or confidential. However, an attempt is made to protect the identity of the reporter. If
the client requests an administrative hearing to contest enforcement action, the identity of the reporter
may be revealed at that time.
Texas
129
Texas (continued)
Medical Advisory Board
Role of the MAB The MAB advises the Department of Public Safety on medical issues regarding individual drivers.
The Department bases its actions on the recommendation of the physician who reviews the case.
Medical Review contact information Texas Department of Public Safety
Medical Advisory Board
PO Box 4087
Austin, TX 78773
512-424-7120
130
Name of State & DMV
contact information
Utah Department of Public Safet
Driver License Division
PO Box 144501
Salt Lake City, UT 84114-4501
www.driverlicense.utah.gov
801-965-4437
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
20/40
20/100 in better eye with restrictions.
No
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
120° horizontal, 20° vertical, 90°
with restrictions
Stereo Optical (DMV2000)
Color vision requirement No
Type of road test In applicant’s own car, with examiner. Certain driving tasks required to complete.
Restricted licenses Yes: daytime only, speed limit <45 mph, radius limit.
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
5 years
Mail in every other cycle if no sus-
pensions, revocations, convictions,
and not more that 4 violations.
Yes, for age 65+. All drivers are
required to take the vision test when
renewing in person. The age-based
vision-testing requirement pertaining
to those 65 and over applies only to
the renewal by mail program.
No
No, unless examiner feels the appli-
cant’s ability to drive is in question
Age-based renewal procedures No
Reporting Procedures
Mandatory medical reporting No
Physician/medical reporting Yes
Immunity Yes, any physician or other person who becomes aware of a physical, mental or emotional impair-
ment which appears to present an imminent threat to driving safety and reports this information to the
Department of Public Safety, through its agents, in good faith shall have immunity from any damages
claimed as a result of so doing.
Legal protection No
DMV follow-up Driver is notified in writing of referral. License is suspended upon referral
Other reporting Will accept information from court, other DMVs, police, family members, and other resources.
Anonymity Not confidential
Utah
131
Utah (continued)
Medical Advisory Board
Role of the MAB A Driver License Medical Advisory Board was created to advise the Director of the Driver License
Division and to recommend written guidelines and standards for determining the physical, mental,
and emotional capabilities appropriate to various types of driving in an effort to minimize the conflict
between the individual’s desire to drive and the community’s desire for safety.
Medical Review contact information Program Coordinator, Utah Driver License Division
PO Box 144501
Salt Lake City, Utah 84114-4501
Phone: 801/965-3819
Fax: 801/965-4084
http://publicsafety.utah.gov/dld/med_standards.html
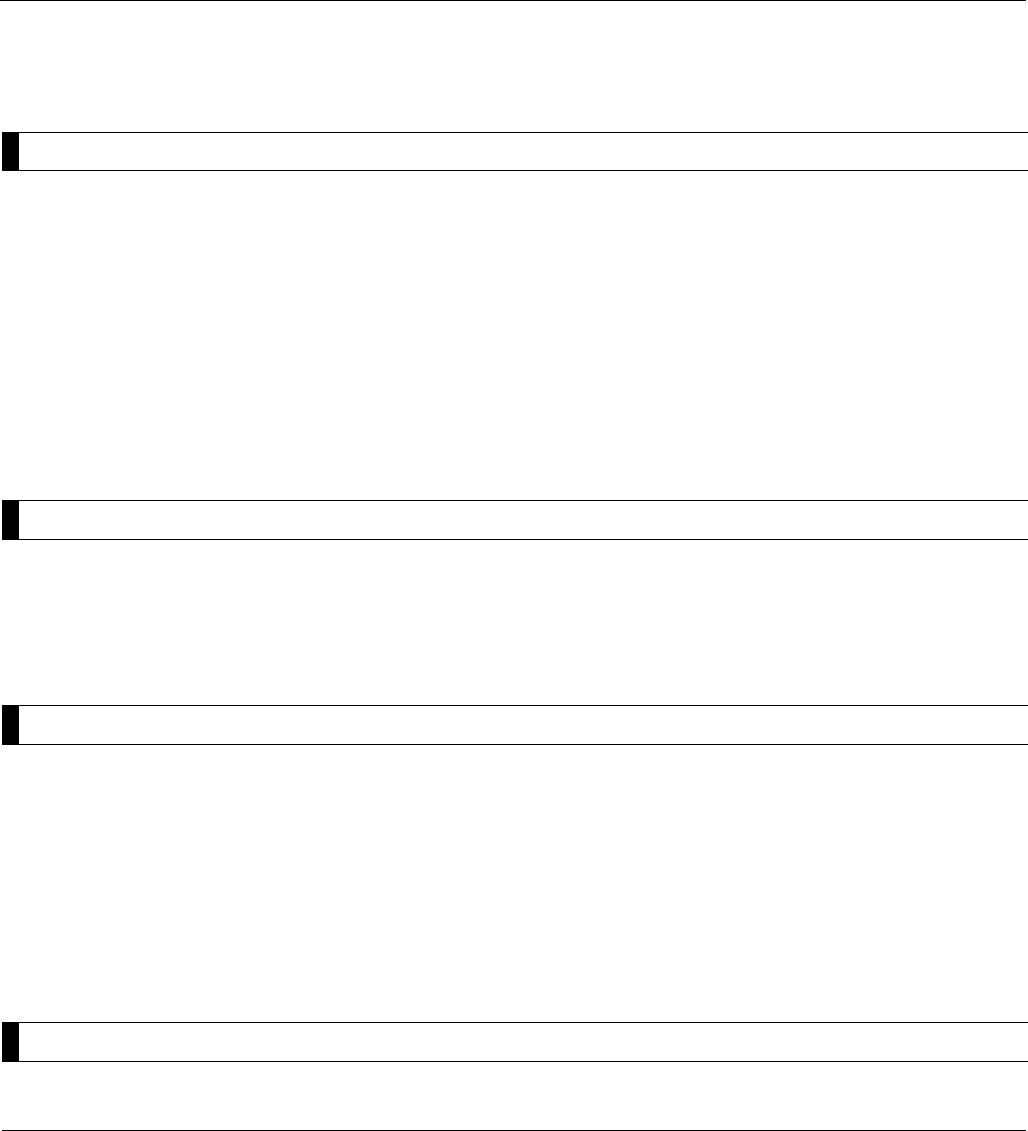
132
Name of State & DMV
contact information
Vermont Department of Motor Vehicles
120 State Street
Montpelier, VT 05603
www.dmv.state.vt.us/dmvhp.htm
802-828-2000
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
20/40
20/40 in better eye.
Yes, and must pass road test, daytime
only under 10,000 lbs.
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
Each eye 60° External binocular, 60°
external and 60° nasal monocular
Yes
Color vision requirement No
Type of road test Standard
Restricted licenses Yes, for glasses or contact lenses
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
2 to 4 years
Mail and in person
No
No
No
Age-based renewal procedures No
Reporting Procedures
Mandatory medical reporting No
Physician/medical reporting Doctors may only provide information to the DMV with the permission of the patient
Immunity No
Legal protection No
DMV follow-up Driver is notified of referral by mail.
Other reporting Will accept information from court, other DMVs, police, concerned citizens, or family members, provided
the complaint is signed.
Anonymity Only up until a hearing is requested.
Medical Advisory Board
Role of the MAB Vermont no longer has a Medical Advisory Board.
Vermont
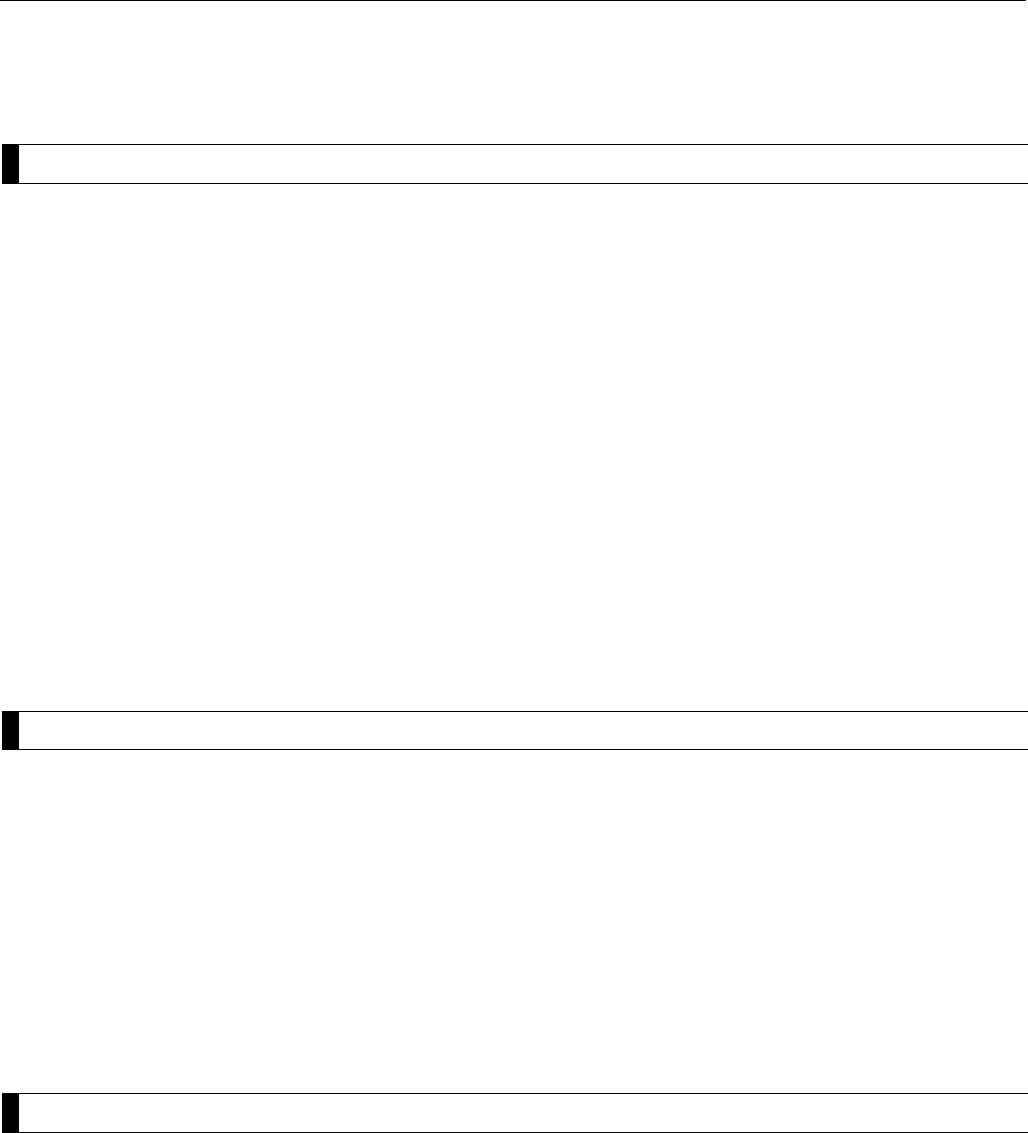
133
Name of State & DMV
contact information
Virginia Department of Motor Vehicles
Attn: Medical Review Center
PO Box 27412
Richmond, VA 23269-0001
www.dmv.state.va.us/
804-367-0531 or 804-367-6203
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
20/40
20/40 better eye, 20/70 daylight only,
20/200 better eye with restrictions.
Yes, with 20/200 through carrier,
20/70 through telescope—test
required.
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
100° monocular and binocular;
70° monocular and binocular—
daylight only. 40 ° or better temporal
and 30° or better nasal—vision in
one eye only.
Stereo Optical/Titmus 10mm W
@333 mm.
Color vision requirement No
Type of road test Behind-the-wheel test is administered with the DMV examiner instructing and evaluating the person on
specific driving maneuvers.
Restricted licenses Yes. A person can obtain a restricted license with a variety of restrictions if authorized by Virginia
law and granted by DMV (based on performance on road test, for medical reasons, or for violation
of probation) or by the court (based on conviction). The restrictions range from corrective lenses,
hand controls, and 5-mile radius of residence, to daylight driving only, ignition interlock device,
and to and from work/school.
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
5 years
Customers may use alternative
method of renewing driver’s license
applications every other cycle unless
suspended or revoked, 2+ violations,
DMV medical review indicator on
license, failed vision test. Alternative
methods include mail-in, Internet,
touch-tone telephone, fax, and
ExtraTeller.
Yes
Only if 2+ violations in 5 years
No
Age-based renewal procedures No
Reporting Procedures
Mandatory medical reporting No
Physician/medical reporting Physicians are not required to report unsafe drivers. However, for physicians who do report unsafe
drivers, laws have been enacted to prohibit release of the physician’s name as the source of the report.
Immunity No
Legal protection
DMV follow-up
Virginia
134
Virginia (continued)
Other reporting DMV relies upon information from courts, other DMVs, law enforcement officers, physicians and other
medical professionals, relatives and concerned citizens to help identify drivers who may be impaired.
Anonymity Virginia law provides confidentiality, only for relatives and physicians.
Medical Advisory Board
Role of the MAB The board enables the Department of Motor Vehicles (DMV) to comply with its responsibilities of
monitoring drivers throughout the State who may have physical or mental problems. The board assists
the commissioner through the development of medical and health standards for use in the issuance of
driver’s licenses. The board helps the department avoid the issuance of licenses to persons suffering
from any physical or mental disability or disease that will prevent their exercising reasonable and ordi-
nary control over a motor vehicle while driving it on the highways. They review the more complex cases
and cases referred for administrative hearings and provide recommendations for medical review action.
Medical Review contact information Questions about medical review can be directed to 804-497-7188
www.dmv.state.va.us/webdoc/citizen/medical/index.asp
135
Name of State & DMV
contact information
Washington Department of Licensing
Driver Services
PO Box 9030
Olympia, WA 98507-9030
www.dol.wa.gov/
360-902-3900
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
20/40
20/40 in better eye; 20/70 in better
eye with restriction. Person must
have vision better than 20/200.
20/50 or worse with both eyes person
must take standard drive test.
Yes: training and test required. Training
is not required but encouraged.
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
110° in horizontal meridian for
binocular and monocular.
OPTEC 1000; Keystone Telebinocular;
Keystone DVSII
Color vision requirement Yes, for new and professional drivers.
Type of road test Standardized scoring using approved test routes at each licensing office.
Restricted licenses Yes, depending on circumstances. Corrective lenses to meet minimum acuity; daytime driving only
based on eye care practitioner’s report, or after failed night time driving test; also if needed to compen-
sate for visual or physical impairment-equipment restrictions, route, distance, or geographic area limits
depending on outcome of testing driver’s ability. We no longer give night drives or have route, distance,
or geographic area limits. We do still have equipment restrictions.
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
5 years
In-State renewal—in person only. Out
of State, can renew by mail once.
Yes, both eyes together only. Full eye
test anytime we issue a new license.
Waived unless warranted by vision,
health or medical screening.
Waived unless warranted by vision,
health or medical screening.
Age-based renewal procedures None
Reporting Procedures
Mandatory medical reporting No
Physician/medical reporting No
Immunity No
Legal protection No
DMV follow-up Letter to the driver with information detailing due process and action following any failure to respond.
Other reporting Will accept information from court, other DMVs, police, family members, and other competent
sources. If in doubt, the reporting party may be required to establish firsthand knowledge and
standing for making a report.
Washington
136
Anonymity Not confidential
Medical Advisory Board
Role of the MAB Washington does not have an MAB.
Medical Review contact information Information on referrals can be found at www.dol.wa.gov/driverslicense/reportunsafe.html
or by writing to
Driver Records
Department of Licensing
PO Box 9030
Olympia, WA 98507-9030
Washington (continued)
137
West Virginia
Name of State & DMV
contact information
West Virginia Department of Transportation
Division of Motor Vehicles
Building 3, Room 1240
1800 Kanawha Boulevard East
Charleston, WV 25317
www.wvdmv.gov
800-642-9066 or 304-558-3900
Licensing Requirements
Visual acuity Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40
20/40
20/60 better eye; if less then optom-
etrist or ophthalmologist must declare
ability to be safe.
No
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
None
No
Color vision requirement No
Type of road test Standard Road Skills Exam
Restricted licenses None
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
5 years
5 years, no examinations required
No
No
No
Age-based renewal procedures None
Reporting Procedures
Mandatory medical reporting No
Physician/medical reporting Physicians are encouraged to report and may do so.
Immunity No
Legal protection No
DMV follow-up A medical report is sent to the driver, to be completed by his/her physician. Failure to comply—the driv-
ers license is revoked.
Anonymity Not confidential
Medical Advisory Board
Role of the MAB To review medical cases and advise the Division on the condition of the driver and how their condition
might affect their ability to drive. If the MAB comes to the conclusion that the driver is unsafe they make
a recommendation to the Commissioner of Motor Vehicles and it is the Commissioner that has the final
say as to revoke the driver.
Medical Review contact information Questions about medical review can go to 304-558-0238
138
Name of State & DMV
contact information
Wisconsin Driver Services, Medical Division
Medical Review Section
PO Box 7918
Madison, WI 53707
www.dot.wisconsin.gov/drivers/index.htm
608-266-2327
Licensing Requirements
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
20/40 to 20/100 in better eye
Not acceptable
20/40 to 20/100 in better eye
20/100 in better eye with or without
correction
Not to meet vision standards but can
use to drive
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
20° better eye for regular license
Stereo optical machines
Color vision requirement Yes
Type of road test Knowledge and sign test, prior to road test. Limited area test is non-fixed, otherwise standardized.
Restricted licenses Yes, restrictions can be recommended by physician, vision specialist or determined by road test (day-
time driving only, mileage radius, road posted and/or freeway restriction).
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
8 years
In person
By mail if person is out of State
Yes
Determined by DOT, vision specialist,
or physician.
Determined by DOT, vision specialist,
or physician
Age-based renewal procedures None
Reporting Procedures
Mandatory medical reporting None
Physician/medical reporting Physicians are not required but encouraged to report. They can report by submitting form MV3141
Driver Condition or Behavior Report or by letter on stationary letterhead.
Immunity Yes
Legal protection Yes
DMV follow-up Driver is notified in writing requirements and depending on requirements given 15, 30, or 60 days to
comply. If do not comply within the time period given, driver’s license is cancelled. They are notified in
writing of cancellation
Other reporting Will accept information from court, other DMVs, police, family members, and other resources.
Anonymity WI has open records law; however, individuals can submit acceptable pledge of confidentiality form
MV3454
Wisconsin
139
Wisconsin (continued)
Medical Advisory Board
Role of the MAB Action is taken based on recommendation of the majority, the individuals driver record, medical informa-
tion provided from physician and, if appropriate, driving examination results. Wisconsin has 2 types of
Medical Review Boards:
1. By-mailboard: paper file is mailed to 3 physicians (specialists, i.e., neurologists, endocrinologists) for
recommendation, based on medical condition.
2. In-person board: interview with 3 physicians (psychiatrist, neurologist, and internal medicine).
The final step in the review process is judicial review which goes through a court process.
Medical Review contact information Information about the medical review program can be obtained through the following:
E-mail: [email protected]
Phone: 608-266-2327
FAX: 608-267-0518
www.dot.wisconsin.gov/drivers/drivers/aging/impaired.htm
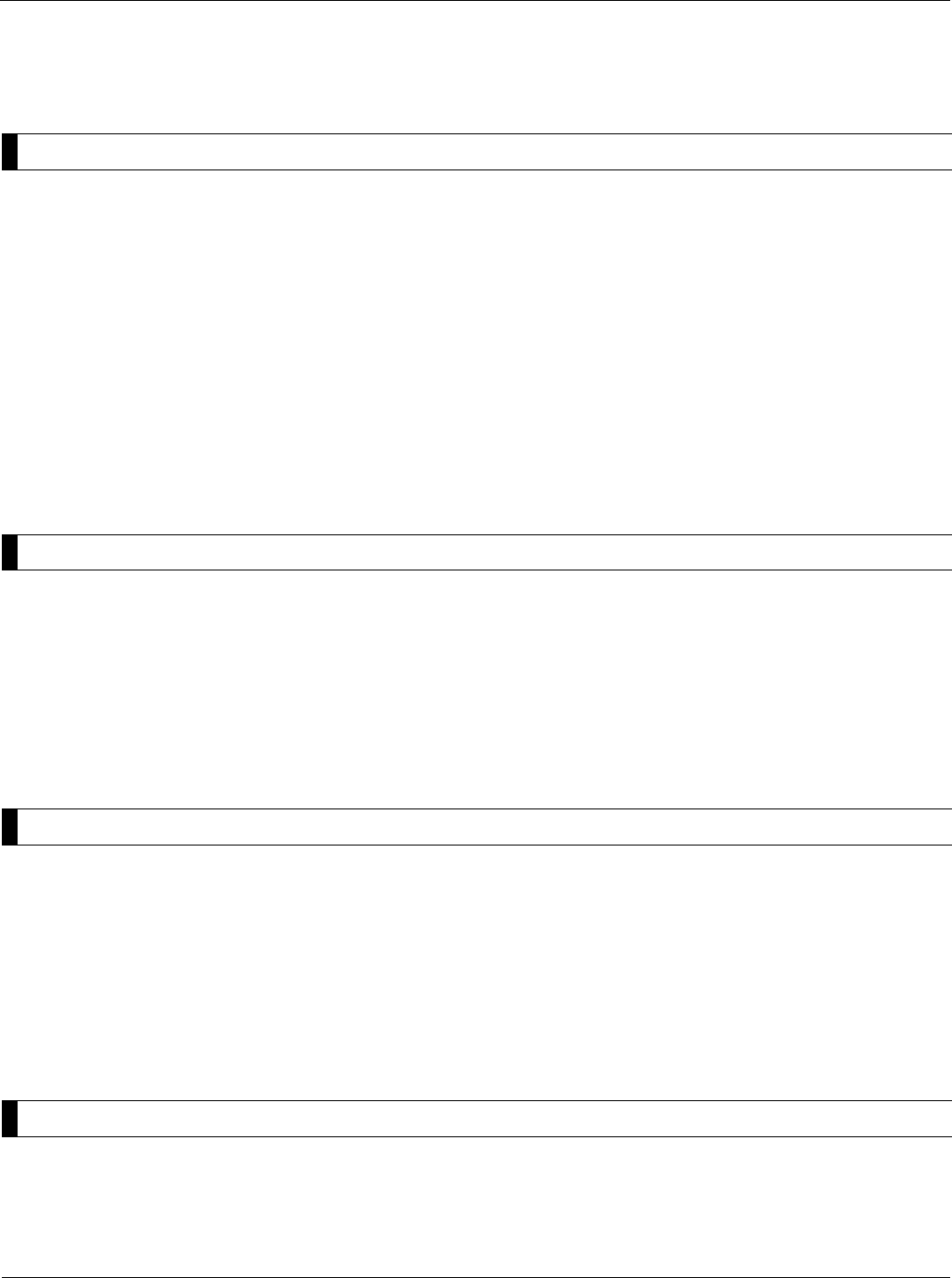
140
Name of State & DMV
contact information
Wyoming Dept. of Transportation
Driver Services Program
5300 Bishop Blvd
Cheyenne, WY 82009-3340
http://dot.state.wy.us
307-777-4871
Licensing Requirements: Must meet minimum of 20/100 with both eyes, with or without correction.
Visual acuity Each eye with/without correction .................................................
Both eyes with/without correction ...............................................
If one eye blind—other with/without correction ............................
Absolute visual acuity minimum ..................................................
Are bioptic telescopes allowed? ..................................................
None
Minimum of 20/100
Minimum of 20/100 with both eyes
20/100
Yes, but the person must meet the
minimum visual acuity & visual field
levels with the lenses–generally
restricted to “no interstate driving”, as
well as restrictions to speed and area.
Visual fields Minimum field requirement .........................................................
Visual field testing device ...........................................................
120°
Keystone Machine
Color vision requirement N/A
Type of road test Driving skills test with an examiner.
Restricted licenses B = glasses required, F = left & right outside rearview mirrors required
G = Daylight driving only, I = limited other (such as distance, speed, etc.)
License Renewal Procedures
Standard Length of license validation.........................................................
Renewal options and conditions ..................................................
Vision testing required at time of renewal? ..................................
Written test required? .................................................................
Road test required? ....................................................................
4 years
Vision screening required for each
renewal.
Yes
No
No—dependent upon vision special-
ist recommendation and/or decrease
in visual acuity level (i.e., 20/50 or
worse visual acuity)
Age-based renewal procedures Are there any age-based license renewal procedures? No
Reporting Procedures
Mandatory medical reporting No
Physician/medical reporting No
Immunity No
Legal protection No
DMV follow-up Re-examinations are performed upon request from family, medical specialists, law enforcement agen-
cies, and examiner observation.
Other reporting Law enforcement, family member, medical specialist, vision specialist, etc.
Anonymity N/A
Medical Advisory Board
Role of the MAB Wyoming does not have a Medical Advisory Board.
Medical Review contact information Requests for review must be made in writing to:
Driver Services - Medical Review
5300 Bishop Blvd.
Cheyenne, WY 82009
Wyoming
141Chapter 8—State Licensing and Reporting Laws
Coley, M. J., Coughlin, J. F. (2001,
Summer). State Driving Regulations.
Adapted from National Academy on an
Aging Society. The Public Policy and
Aging Report, Volume 11, Number 4.
Washington, DC: The Gerontological
Society of America.
Epilepsy Foundation. Driver information
by State. www.epilepsyfoundation.org/living
/wellness/transportation/drivinglaws.cfm.
Accessed November 21, 2007.
Insurance Institute for Highway Safety.
(2007). U.S. driver licensing procedures
for older drivers. www.iihs.org/laws/
olderdrivers.aspx. Accessed November
31, 2007.
Insurance Information Institute. (2007).
Older Drivers. New York. www.iii.org/
media/hottopics/insurance/olderdrivers/?p
rinterfriendly=yes. Accessed November
21, 2007.
NHTSA. (2003). Older Drivers: State
Reporting Practices. DOT HS 809 301,
2003. Washington, DC: National
Highway Trafc and Safety Administra-
tion www.nhtsa.dot.gov/people/injury/
olddrive/FamilynFriends/state.htm.
Accessed November 21, 2007.
Staplin, L. (2003). Model Driver
Screening and Evaluation Program:
Guidelines for Motor Vehicle Ad-
ministrators. Washington, DC: Na-
tional Highway Trafc and Safety
Administration www.nhtsa.com/people/
injury/olddrive/modeldriver/guidelines.
htm#Table%20of%20Contents.
Accessed November 22, 2007.
Resources

CHAPTER 9
Medical Conditions and
Medications That May
Affect Driving
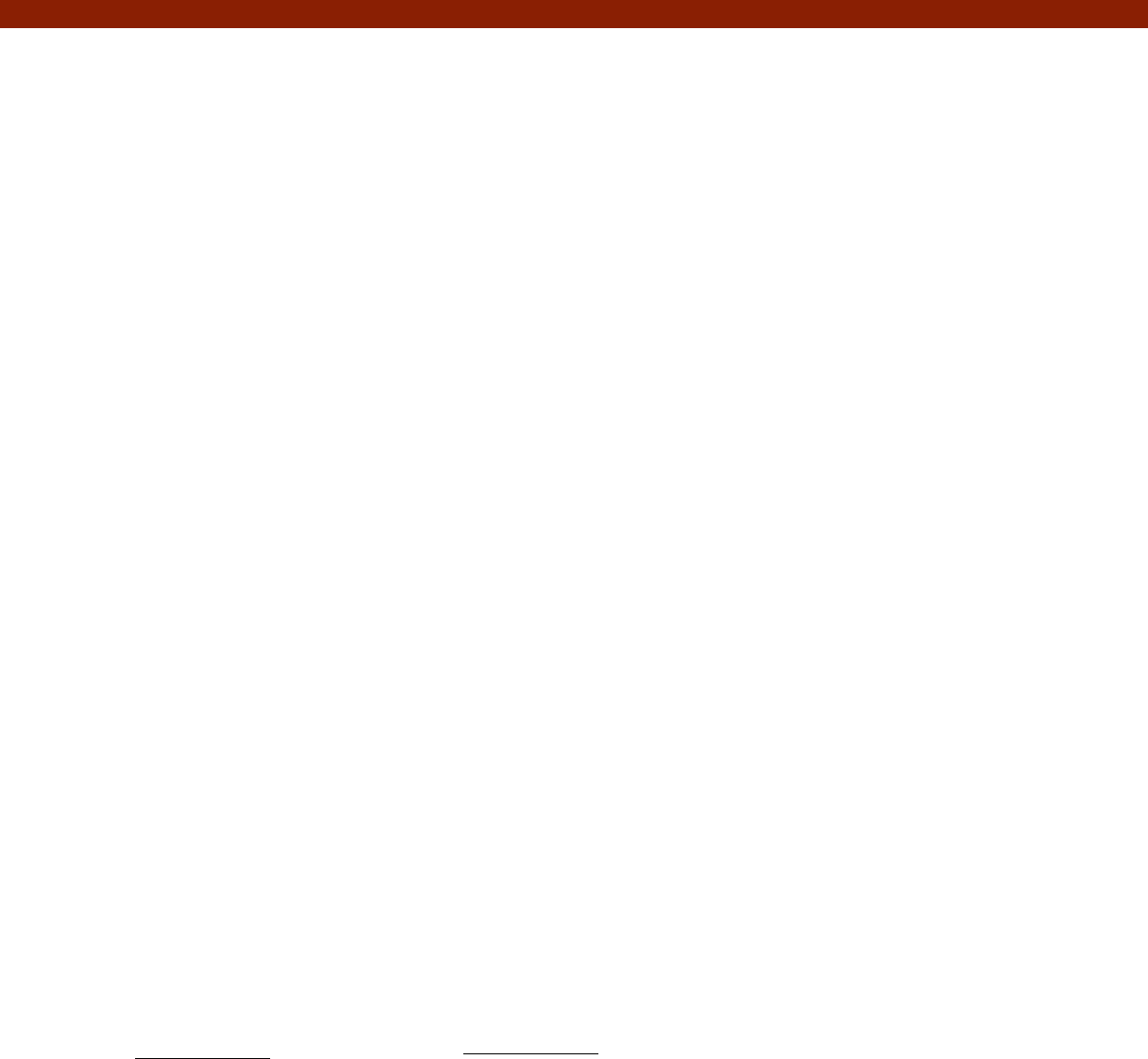
145
cognition, or motor function) that may
affect his/her driving safety, the physi-
cian may base interventions for driving
safety on this chapter’s guidelines. We
make the following recommendations:
• Treat the underlying medical condi-
tion to correct functional decits and
prevent further functional decline.
• If the functional decit is due to an
offending agent (e.g., medication
with impairing side effects), remove
the offending agent or reduce the
dose, if possible.
• Advise the patient about the risks to
his/her driving safety, and recommend
driving restrictions or driving cessa-
tion as needed.
• For acute or episodic illnesses (e.g.,
seizure disorder and/or diabetics with
hypoglycemia), clinical judgment and
subspecialist input is recommended,
in addition to following specic State
statutes.
If further evaluation is required or the
functional decits are not medically
correctable, refer the patient to a driver
rehabilitation specialist for a driv-
ing evaluation (including an on-road
assessment) for a chronic condition
whenever possible. The driver rehabili-
tation specialist may prescribe adaptive
techniques and devices to compensate
for these decits, and train the patient
in their use. (See Chapter 5 for a further
discussion of driver rehabilitation
services.)
Physicians should advise patients
against driving if they report symptoms
Australia,
190
the United Kingdom,
191
and New Zealand.
192
Although the corresponding recom-
mendations are based on scientic
evidence whenever possible, please note
that use of these recommendations has
not yet been proven to reduce crash
risk,
193
except for a few medical condi-
tions (e.g., treating obstructive sleep
apnea, performing cataract surgery,
and discontinuing a benzodiazepine).
As such, these recommendations are
provided to physicians as a tool to guide
the decision-making process. They are
not intended to substitute for the physi-
cian’s clinical judgment.
How to use this chapter
Physicians may consult this chapter if
they have questions on specic medical
conditions and their effect on driving.
If a patient presents with a particular
medical condition and/or related func-
tional decits (e.g., decits in vision,
190. Austroads. Assessing Fitness to Drive for
Commercial and Private Vehicle Drivers.
Medical Standards for Licensing and Clinical
Management Guidelines. A Resource for Health
Professionals in Australia; 2003.
191. Driver Medical Group DVLA Swansea for
Medical Practitioners. At a Glance Guide to the
Current Medical Standards of Fitness to Drive.
(2003). Swansea, UK.
192. Land Transport Safety Authority. (2002).
Medical Aspect of Fitness to Drive. Wellington,
New Zealand.
193. Although scientic evidence links certain
medical conditions and levels of functional im-
pairment with crash risk, more research is needed
to establish that driving restrictions based on
these medical conditions and levels of functional
impairment signicantly reduce crash risk.
This chapter contains a reference table
of medical conditions and medications
that may affect driving skills, with
consensus recommendations for each.
Whenever scientic evidence supports
the recommendations, it is included.
These recommendations apply only
to drivers of private motor vehicles, and
should not be applied to commercial
drivers. Although many of the listed
medical conditions are more prevalent
in the older population, these recom-
mendations apply to all drivers with
medical impairments, regardless of age.
The medical conditions were chosen
for their relevance to clinical practice
and/or because there is some evidenced-
based literature indicating a correlation
with driving impairment. The inter-
ested clinician is referred to two recent
reviews that comprehensively covered
many of these conditions.
187
188
In addi-
tion, several other countries have pub-
lished guidelines, including Canada,
189
187. Charlton, J., Koppel, S., O’Hare, M., et al.
(2004). Inuence of Chronic Illness on Crash
Involvement of Motor Vehicle Drivers. Monash
University. Accident Research Centre. Report
#213. Supported by Swedish National Road
Administration. Melbourna, Australia: Monash
University.
188. Dobbs, B. M. (2002). Medical Conditions and
Driving: Current Knowledge, Final Report As-
sociation for the Advancement of Automotive
Medicine. NHTSA Publication DOT HS 809
690. Washington, DC: National Highway Traf-
c Safety Administration. www.nhtsa.dot.gov/
people/injury/research/Medical_Condition_Driving/
pages/TRD.html.
189. Canadian Medical Association. Determining
Medical Fitness to Drive: A Guide for Physicians,
6th ed. Ottawa; 2000.
CHAPTER 9
Medical Conditions and
Medications That May
Affect Driving

146 Chapter 9—Medical Conditions and Medications That May Affect Driving
Section 1:
Vision and hearing loss
Vision is the primary sense employed
in driving when compared to hearing
and proprioception, and is responsible
for 95 percent of driving-related sensory
inputs.
194
Age- and disease-related
changes of the eye and brain may affect
visual acuity, visual elds, night vision,
contrast sensitivity, and other aspects
of vision. External obstruction of view
(e.g., blepharoptosis) should not be
overlooked, as it may signicantly limit
visual elds. The literature that is avail-
able on eye disease suggests that driving
impairment is likely mediated by im-
pairment in contrast sensitivity,
195
visual
elds,
196
or visual processing speed.
Whenever possible, vision decits
should be managed and corrected.
Recent data suggest that intervention
with current treatments for common
eye diseases such as age-related macular
degeneration,
197
glaucoma,
198
and cata-
racts
199
have the potential to improve
or stabilize the condition, and in some
cases these interventions have been
noted to reduce crash risk.
200
Patients
with persistent vision decits may
reduce their impact on driving safety by
restricting travel to low-risk areas and
conditions, such as familiar surround-
194. Shinar, D., & Schieber, F. (1991). Visual
requirements for safety and mobility of older
drivers. Hum Factors. 33(5):507–519.
195. Mabtyjari, M., & Tuppurainen, K. (1999). Cata-
ract in trafc. Graefes Arch Clin Exp Ophthalmal.
237:278–282.
196. Szlyk, J. P., Mahler, C. L., Seiple, W., et al.
(2005). Driving performance of glaucoma
patients correlates with peripheral visual eld
loss. J Glaucoma. 14:145–150.
197. Smith, B.T., Joseph, D.P., & Grand,
M.G.(2007). Treatment of neovascular age-
related macular degeneration: past, present,
and future directions. Curr Opin Ophthalmol.
18:240–244.
198. Leske, M.C., Hejl, A., Hussein, M., et al.
(2003). Factors for glaucoma progression and
the effect of treatment: the Early Manifest
Glaucoma Trial. Arch Ophthamol. 121:48–56.
199. Van Den Berg, T., Van Rijn, L.J., Rene, M.,
Michael, R., Heine, C., et al. (2007). Straylight
effects with aging and lens extraction. Am J
Ophthalmol. 144(3):358–363.
200. Owsley, C., McGwin, G. Jr., Sloane, M., et al.
(2002). Impact of cataract surgery on motor
vehicle crash involvement by older adults.
JAMA. 288:841–849.
Medical conditions and medi-
cations that may affect driving
Table of contents
Contents .......................................Page
Section 1 .......................................126
Vision and Hearing Loss
Section 2 .......................................130
Cardiovascular Diseases
Section 3 .......................................134
Cerebrovascular Diseases
Section 4 .......................................136
Neurologic Diseases
Section 5 .......................................142
Psychiatric Disorders
Section 6 .......................................144
Metabolic Disorders
Section 7 .......................................146
Musculoskeletal Disabilities
Section 8 .......................................150
Peripheral Vascular Diseases
Section 9 .......................................151
Renal Disease
Section 10 .....................................152
Respiratory Diseases
Section 11 .....................................154
Effects of Anesthesia and Surgery
Section 12 .....................................156
Miscellaneous Conditions
Section 13 .....................................157
Medications
that are irreversible and incompatible
with safe driving (e.g., visual changes,
syncope or pre-syncope, vertigo, severe
pain, etc.). If despite extensive medi-
cal work-up these symptoms continue,
such patients should be strongly urged
to seek alternate forms of transporta-
tion, including taxis, rides from family
and friends, and medical transportation
services.
In the inpatient and emergency depart-
ment, driving should be routinely ad-
dressed prior to the patient’s discharge
whenever appropriate, especially when
prescribing new sedating medications.
Even for the patient whose symptom
or treatment clearly precludes driv-
ing, it should not be assumed that the
patient is aware that he/she should not
drive. The physician should counsel the
patient regarding driving, and discuss a
future plan (e.g., resumption of driving
upon resolution of symptoms, driver
rehabilitation upon stabilization of
symptoms, and so forth.).
Keep in mind that an individual’s driv-
ing purposes (e.g., responsible for taking
grandchildren to day care) and/or need
to drive for a vocation (e.g., salesperson
who has increased exposure or miles
driven per year) may inuence the
extent of the interventions or advice in
regard to an evaluation. For example,
more restriction or a performance-based
road test may be more aggressively pur-
sued for a patient who frequently drives
long distances over unfamiliar roads
in comparison to a patient who drives
short, familiar routes.
147Chapter 9—Medical Conditions and Medications That May Affect Driving
Section 1: Sensory deprivation
ings, low speed areas, non-rush hour
trafc, daytime, and good weather con-
ditions. This has been noted for certain
eye diseases, especially glaucoma.
201
201. Adler, G., Bauer, M. J., Rottunda, S., et al.
(2005). Driving habits and patterns in older
men with glaucoma. Social Work Health Care.
40(3):75–87.
Sensory Deprivation
1. Visual acuity
a. Cataracts
b. Retinopathy
(diabetic or hypertensive)
c. Keratoconus
d. Macular degeneration
e. Nystagmus
f. Telescopic lens
2. Visual eld
a. Glaucoma
b. Hemianopia/quadrantanopia
c. Monocular vision
d. Ptosis or upper lid redundancy
e. Retinitis pigmentosa
3. Contrast sensitivity
4. Defective color vision
5. Poor night vision and glare recovery
6. Diplopia
7. Hearing loss
Please note that the recommendations stated below are subject to your particular
State’s licensing requirements. (See Chapter 8 for a State-by-State reference list of
licensing requirements.) Many States require far visual acuity of 20/40 for licensure;
however, recent studies indicate that there may be no basis for this requirement.3
State driver licensing agencies are urged to base their visual acuity requirements
on the most current data, as appropriate. However, referral to an ophthalmologist
is recommended since common causes for visual impairment (cataracts, macular
degeneration, glaucoma) can improve and/or stabilize with treatment.
Visual acuity may be measured with both eyes open or with the best eye open, as
the patient prefers. The patient should wear any corrective lenses usually worn for
driving.
Patients with decreased far visual acuity may lessen its impact on driving safety
by restricting driving to low-risk areas and conditions (e.g., familiar surroundings,
non-rush hour trafc, low speed areas, daytime, and good weather conditions).
For best-corrected far visual acuity less than 20/70, the physician should recom-
mend an on-road assessment performed by a driver rehabilitation specialist (where
it is permitted and available) to evaluate the patient’s performance in the actual
driving task.
For best-corrected far visual acuity less than 20/100, the physician should recom-
mend that the patient not drive unless safe driving ability can be demonstrated in
an on-road assessment, where permitted and available. (See also Telescopic lens in
this section.)
No restrictions if standards for visual acuity and visual elds are met, either with or
without cataract removal.
Patients who require increased illumination or who experience difculty with glare
recovery should avoid driving at night and under low-light conditions, such as
adverse weather conditions.
No restrictions if standards for visual acuity and visual elds are met.
It is recommended that diabetic patients have annual eye examinations.
Visual acuity
Cataracts
Diabetic or hypertensive retinopathy
148
Patients with severe keratoconus correctable with hard contact lenses should drive
only when the lenses are in place. If lenses cannot be tolerated, patients with severe
keratoconus should not drive even if they meet standards for visual acuity, as their
acuity dramatically declines outside their foveal vision, rendering their peripheral
vision useless.
No restrictions if standards for visual acuity and visual elds are met.
Patients who experience difculty with glare recovery should avoid driving at
night. Patients with the neovascular “wet” form of the disease may require frequent
assessment due to the rapid progression of the disease.
No restrictions if standards for visual acuity and visual elds are met.
A bioptic telescope is an optical telescope mounted on the lens of eyeglasses. Dur-
ing normal use, the wearer can view the environment through the regular lens.
When extra magnication is needed, a slight downward tilt of the head brings the
object of interest into the view of the telescope.
202
The specialist who prescribes a
telescopic lens should ensure that the patient is properly trained in its use.
It has not been established whether telescopes enhance the safety of low-vision
drivers. As stated in the American Academy of Ophthalmology’s Policy Statement,
Vision Requirements for Driving (approved by Board of Trustees, October 2001):
“More than half the States allow drivers to use bioptic telescopes mounted on
glasses, through which they spot trafc lights and highway signs. It has not yet
been demonstrated whether the estimated 2,500 bioptic drivers in the United
States drive more safely with their telescopes than they would without them. The
ability to drive safely using bioptic telescopes should be demonstrated in a road
test in all cases.”
Please note that the statement above is subject to your particular State’s licensing
requirements. A road test should be administered only in those States that permit
the use of bioptic telescopes in driving.
While it is acknowledged that an adequate visual eld is important for safe driving,
there is no conclusive evidence to dene what is meant by “adequate” nor any con-
sistent standard as to how visual elds are tested. Visual eld requirements vary be-
tween States, with many States requiring a visual eld of 100 degrees or more along
the horizontal plane, and other States having a lesser requirement or none at all.
203
(See Chapter 8 for a State-by-State reference list of visual eld requirements.)
If the primary care physician has any reason to suspect a visual eld defect (e.g.,
through patient report, medical history, or confrontation testing), he/she should
refer the patient to an ophthalmologist or optometrist for further evaluation. The
primary care physician and specialist should be aware of their particular State’s
visual eld requirements, if any, and adhere to them.
202. Peli, E., & Peli, D. (2002). Driving With Condence: A Practical Guide to Driving with Low Vision.
Singapore: World Scientic Publishing Co. Pte. Ltd.; p.100–101.
203. Peli, E., & Peli, D. (2002). Driving With Condence: A Practical Guide to Driving with Low Vision. Singa-
pore: World Scientic Publishing Co. Pte. Ltd.; p.20–22.
Keratoconus
Macular degeneration
Nystagmus
Telescopic lens
Visual eld
Chapter 9—Medical Conditions and Medications That May Affect Driving
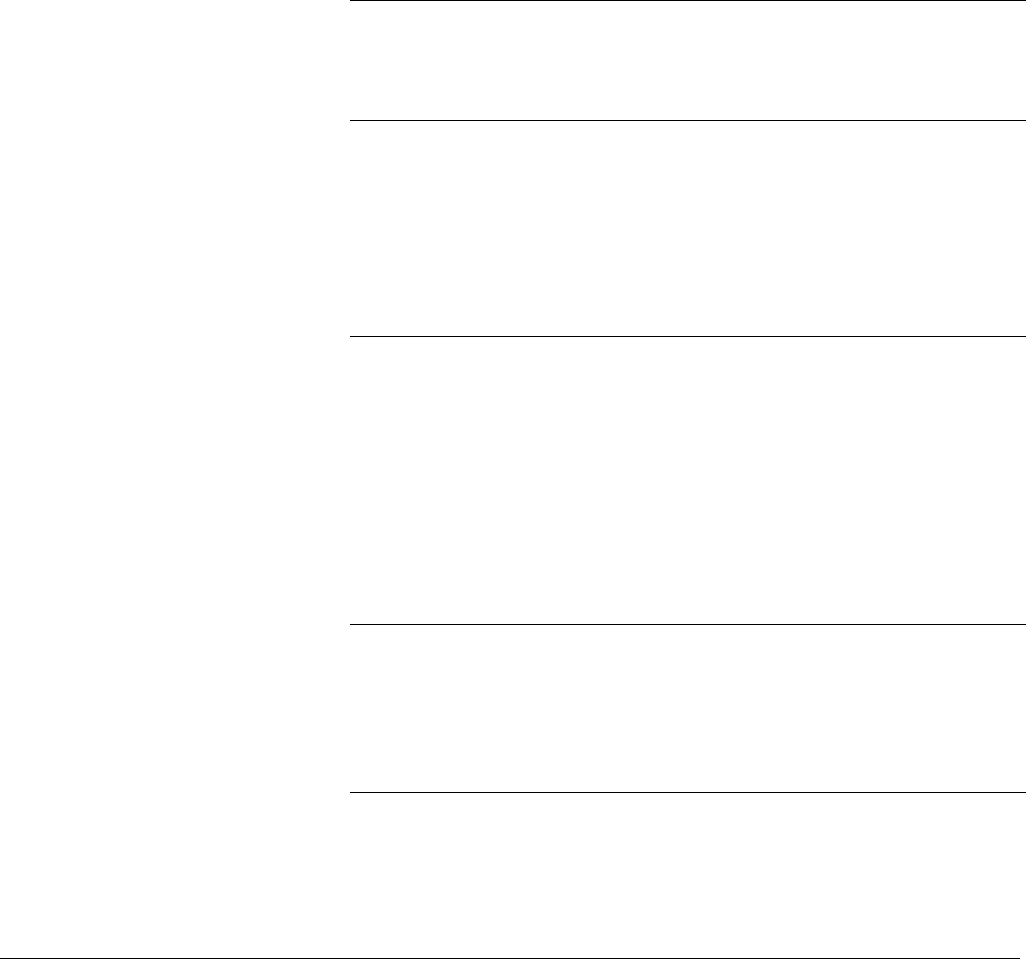
149
For binocular visual eld at or near the State minimum requirement or of question-
able adequacy (as deemed by clinical judgment), a driver evaluation (including
on-road assessment) performed by a driver rehabilitation specialist is strongly rec-
ommended. Through driving rehabilitation, the patient may learn how to compen-
sate for decreased visual elds, although not hemi-neglect. In addition, the driver
rehabilitation specialist may prescribe enlarged side and rear view mirrors as needed
and train the patient in their use.
No restrictions if standards for visual acuity and visual elds are met. Continued
follow-up with an ophthalmologist and monitoring of visual elds and intraocular
pressure are recommended.
The physician may choose to refer the patient to a driver rehabilitation special-
ist for assessment and rehabilitation. With or without rehabilitation, the patient
should drive only if he/she demonstrates safe driving ability in an on-road assess-
ment performed by a driver rehabilitation specialist.
Please note that the recommendations stated above are subject to your particular
State’s licensing restrictions, if any, for hemianopia and quadrantanopia.
Patients with acquired monocularity may need time to adjust to the lack of depth
perception and reduction in total visual eld. This period of adjustment varies
among individuals, but it is reasonable to recommend temporary driving cessation
for several weeks.
Following this period, there are no restrictions if standards for visual acuity and
visual elds are met. Upon resumption of driving, patients should be advised to
assess their comfort level by driving in familiar, trafc-free areas before advancing
to heavy trafc. Again, use of larger mirrors and evaluation and training by a driver
rehabilitation specialist is encouraged.
Individuals with xed ptosis or lid redundancy may drive without restrictions
if their eyelids do not obscure the visual axis of either eye, and they are able to
meet standards for visual acuity and visual elds without holding their head in an
extreme position. Blepharospasms should be controlled so there is no interference
with vision.
No restrictions if standards for visual acuity and visual elds are met.
Patients who require increased illumination or who experience difculty adapting
to changes in light should not drive at night or under low-light conditions, such as
during storms.
Glaucoma
Hemianopia/Quadrantanopia
Monocular vision
Ptosis or lid redundancy, blepharospasm
Retinitis pigmentosa
Visual eld (continued)
Chapter 9—Medical Conditions and Medications That May Affect Driving
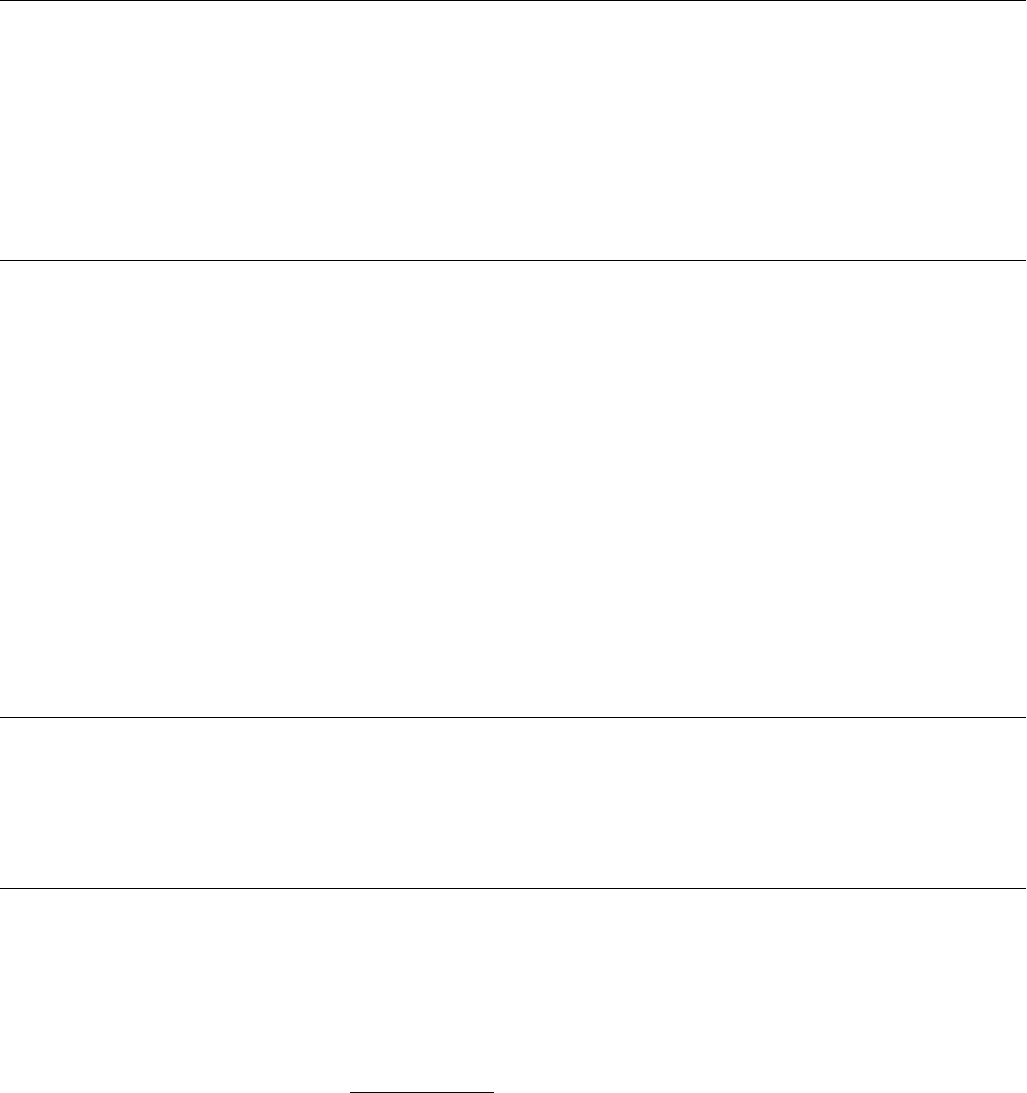
150
Contrast sensitivity is a measure of an individual’s ability to perceive visual stimuli
that differ in contrast and spatial frequency. Contrast sensitivity tends to decline
with age; accordingly, decits in contrast sensitivity are much greater in older indi-
viduals compared to their younger counterparts.
204
Among older drivers, binocular measures of contrast sensitivity have been found
to be a valid predictor of crash risk in patients with cataracts.
205
However, there are
presently no standardized cut-off points for contrast sensitivity and safe driving,
and it is not routinely measured in eye examinations.
No restrictions if standards for visual acuity and visual elds are met.
Decits in color vision are common (especially in the male population) and
usually mild.
There appears to be no correlation between defective color vision and crash
rates.
206
Only 19 States require prospective drivers to undergo color vision screen-
ing, and most of these States require screening for commercial drivers only.
207
Despite reported difculties with color vision discrimination while driving (dif-
culty distinguishing the color of trafc signals, confusing trafc lights with street
lights, and difculty detecting brake lights), it is unlikely that color vision impair-
ments represent a signicant driving hazard.
208
With the standardization of trafc
signal positions, color blind individuals are able to interpret trafc signals correctly
because they can identify the trafc signal by its position. Physicians may wish to
advise patients that the order of signals in the less commonly used horizontal place-
ment is (from left to right) red, yellow, green.
If the patient reports poor visibility at night, the physician should recommend
optometric and/or ophthalmologic evaluation. If the evaluation does not reveal a
treatable cause for poor night vision, the physician should recommend that the pa-
tient not drive at night or under other low-light conditions, such as during storms
or at dusk.
Patients with double vision in the central aspect of vision (20 degrees above and
below, left and right of xation) should not drive. Patients with uncorrected diplo-
pia should be referred to an ophthalmologist or optometrist for further assessment
to determine if the defect can be corrected with prisms or a patch and meet stan-
dards for driving. There should be a three-month adjustment period, after which
specialists can determine if adequate adjustment has occurred.
209
204. Dobbs, B. M. (2002, February). Medical Conditions and Driving: Current Knowledge, p. 15. DTNH22-
94-G-05297. Submitted to the Association for the Advancement of Automotive Medicine under
contract with the Washington, DC: National Highway Trafc Safety Administration.
205. Owsley, C., Stalvey, B. T., Wells, J., et al. (2001). Visual risk factors for crash involvement in older drivers
with cataract. Arch Opthalmol. 119: 881–887.
206. Policy Statement. American Association of Ophthalmology, 2006. www.aao.org/about/policy/upload/
AAODrivingPolicyWebcopy.pdf. Accessed December 12, 2007.
207. Peli, E., & Peli, D. (2002). Driving With Condence: A Practical Guide to Driving with Low Vision.
Singapore: World Scientic Publishing Co. Pte. Ltd.; p.25.
208. Dobbs, B. M. (2002, February). Medical Conditions and Driving: Current Knowledge. DTNH22-
94-G-05297. Submitted to the Association for the Advancement of Automotive Medicine under
contract with NHTSA, p. 15. Washington, DC: National Highway Trafc Safety Administration.
209. Canadian Ophthalmological Society. Vision Standards for Driving in Canada, 2000. http://eyesite.ca/
english/program-and-services/policy-Statements-guidelines/drivingstd.html. Accessed December 12, 2007.
Contrast sensitivity
Defective color vision
Poor night vision
Diplopia
Chapter 9—Medical Conditions and Medications That May Affect Driving
151
No restrictions.
Relatively few studies have examined the relationship between hearing
impairment and risk of motor vehicle crash. Of these, none have shown a
signicant relationship between hearing impairment and risk of crash.
210
210. Dobbs, B. M. (2002, February). Medical Conditions and Driving: Current Knowledge. DTNH22-
94-G-05297. Submitted to the Association for the Advancement of Automotive Medicine under
contract with NHTSA, p. 37-38. Washington, DC: National Highway Trafc Safety Administration.
Hearing loss
Section 2:
Cardiovascular diseases
1. Unstable coronary syndrome
(unstable angina or myocardial
infarction)
2. Cardiac conditions that may cause a
sudden, unpredictable loss of
consciousness
a. Atrial utter/brillation with
bradycardia or rapid ventricular
response
b. Paroxysmal supraventricular
tachycardia (PSVT), including
Wolf-Parkinson-White (WPW)
syndrome
c. Prolonged, nonsustained
ventricular tachycardia (VT)
d. Sustained ventricular
tachycardia
e. Cardiac arrest
f. High grade atrio-ventricular
(AV) block
g. Sick sinus syndrome/sinus
bradycardia/sinus exit block/
sinus arrest
3. Cardiac disease resulting from struc-
tural or functional abnormalities
a. Congestive heart failure (CHF)
with low output syndrome
b. Hypertrophic obstructive
cardiomyopathy
c. Valvular disease
(especially aortic stenosis)
4. Time-limited restrictions: cardiac
procedures
a. Percutaneous transluminal coro-
nary angioplasty (PTCA)
b. Pacemaker insertion or revision
c. Cardiac surgery involving
median sternotomy
d. Coronary artery bypass graft
(CABG)
e. Valve repair or replacement
f. Heart transplant
5. Internal cardioverter debrillator
(ICD)
Although the data are still unclear
in regard to a denitive relationship
between crash risk and cardiovascu-
lar diseases, a recent study did note a
modest increase in total crash risk and
at-fault risk for older adults with cardiac
disease.
211
For the patient with known
cardiac disease, the physician should
strongly and repeatedly caution him/
her to seek help immediately upon
experiencing any symptoms—including
prolonged chest discomfort, acute short-
ness of breath, syncope, pre-syncope,
palpitations, lightheadedness—that may
indicate an unstable cardiac situation.
Under no circumstances should the
patient drive to seek help.
While hypertension is not included
in this section, physicians should
always be alert to any potential impair-
ment in driving skills resulting from
hypertensive end-organ damage or
antihypertensive medications.
211. McGwin, G., Sims, R. V., Pulley, L., &
Roseman, J. M. (2000). Relations among
chronic medical conditions, medications,
and automobile crashes in the elderly: a
population-based case-control study.
Am J Epidemiol. 152,424–431.
Chapter 9—Medical Conditions and Medications That May Affect Driving
152
Patients should not drive if they experience symptoms at rest or at the wheel.
Patients may resume driving when they have been stable and asymptomatic for
one to four weeks, as determined by the cardiologist, following treatment of the
underlying coronary disease. Driving may usually resume within one week after
successful revascularization by percutaneous transluminal coronary angioplasty
(PTCA) and by four weeks after coronary artery bypass grafting (CABG).
212
(See also recommendations for CABG below [4.c in this section].)
A main consideration in determining medical tness to drive for patients with
cardiac conditions is the risk of pre-syncope or syncope due to a brady- or ta-
chyarrhythmia.
213
For the patient with a known arrhythmia, the physician should
identify and treat the underlying cause of arrhythmia, if possible, and recommend
temporary driving cessation until control of symptoms has been achieved.
No further restrictions once control of heart rate and symptoms have been
achieved.
No restrictions if the patient is asymptomatic during documented episodes.
Patients with a history of symptomatic tachycardia may resume driving after they
have been asymptomatic for six months on antiarrhythmic therapy.
Patients who undergo radio frequency ablation may resume driving after six months
if there is no recurrence of symptoms, or sooner if no pre-excitation or arrhythmias
are induced at repeat electrophysiologic testing.
No restrictions if the patient is asymptomatic during documented episodes.
Patients with symptomatic VT may resume driving after three months if they are
on antiarrhythmic therapy (with or without an ICD) guided by invasive electro-
physiologic (EP) testing, and VT is noninducible at repeat EP testing. They may
resume driving after six months without arrhythmia events if they are on empiric
antiarrhythmic therapy (with or without an ICD), or have an ICD alone without
additional antiarrythmic therapy.
214
Patients may resume driving after three months if they are on antiarrhythmic
therapy (with or without an ICD) guided by invasive electrophysiologic (EP)
testing, and VT is noninducible at repeat EP testing.
Patients may resume driving after six months without arrhythmia events if they are
on empiric antiarrythmic therapy (with or without an ICD), or have an ICD alone
without additional antiarrythmic therapy.
215
212. Petch, M. C. (1998). European Society of Cardiology Task Force Report: Driving and Heart Disease.
Eur Heart J. 19(8):1165–1177.
213. Binns, H., & Camm, J. (2002). Driving and arrhythmias. Br Med J. 324:927–928.
214. Epstein, A. I., Miles, W. M., Benditt, D. G., et al. (1996). Personal and public safety issues related to
arrhythmias that may affect consciousness: implications for regulation and physician recommendations.
Circulation. 94:1147–1166.
215. Ibid.
Section 2: Cardiovascular diseases
Unstable coronary syndrome
(unstable angina or myocardial
infarction)
Cardiac conditions that may cause
a sudden, unpredictable loss of
consciousness
Atrial utter/brillation with bradycardia
or rapid ventricular response
Paroxysmal supraventricular tachycardia
(PSVT), including Wolf-Parkinson-White
(WPW) syndrome
Prolonged, nonsustained ventricular
tachycardia (VT)
Sustained ventricular tachycardia (VT)
Chapter 9—Medical Conditions and Medications That May Affect Driving
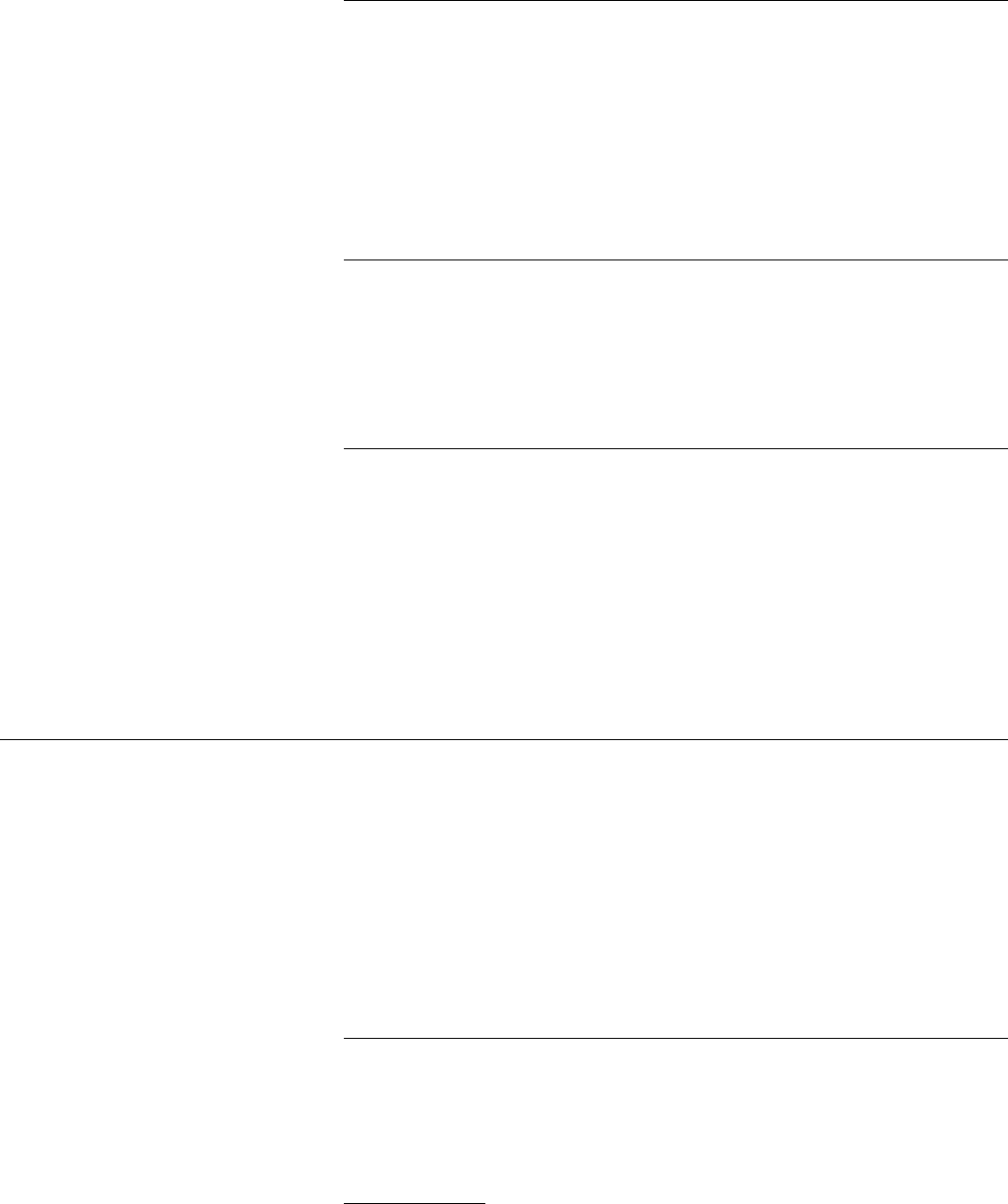
153
When long-distance or sustained high-speed travel is anticipated, patients should
be encouraged to have an adult companion perform the driving. Patients should
avoid the use of cruise-control.
216
Please refer to the recommendations for sustained ventricular tachycardia.
If the patient experiences a seizure, please refer to the recommendations for seizure
disorder in Section 4, Neurological Diseases.
If clinically signicant cognitive changes persist following the patient’s physical re-
covery, cognitive testing is recommended before the patient is permitted to resume
driving. In addition, on-road testing performed by a driver rehabilitation specialist
may be useful in assessing the patient’s tness to drive.
For symptomatic block managed with pacemaker implantation, please see
pacemaker recommendations in this section.
For symptomatic block corrected without a pacemaker (e.g., by withdrawal of medi-
cations that caused the block), the patient may resume driving after he/she has been
asymptomatic for four weeks and EKG documentation shows resolution of the block.
No restrictions if patient is asymptomatic. Regular medical follow-up is recom-
mended to monitor progression.
For symptomatic disease managed with pacemaker implantation, please see
pacemaker recommendations in this section.
Physicians should be alert to possible cognitive decits due to chronic cerebral
ischemia. Physicians may refer patients with clinically signicant cognitive
changes to a driver rehabilitation specialist for a driver evaluation (including
on-road assessment) to evaluate the patient’s driving safety.
A main consideration in determining medical tness to drive for patients with
abnormalities of cardiac structure or function is the risk of pre-syncope or syncope
due to low cardiac output, and of cognitive decits due to chronic cerebral ischemia.
Patients who experience pre-syncope, syncope, extreme fatigue, or dyspnea at rest
or at the wheel should cease driving.
Cognitive testing is recommended for those patients with a history of cognitive
impairment that may impair the patient’s driving ability. Physicians may refer
patients with clinically signicant cognitive changes to a driver rehabilitation
specialist for a driver evaluation (including on-road assessment) to evaluate the
patient’s driving safety.
216. Ibid.
Sustained ventricular tachycardia (VT)
(Continued)
Cardiac arrest
High grade atrio-ventricular (AV) block
Sick sinus syndrome/sinus bradycardia/
sinus exit block/ sinus arrest
Cardiac disease resulting from
structural or functional abnormalities
Chapter 9—Medical Conditions and Medications That May Affect Driving
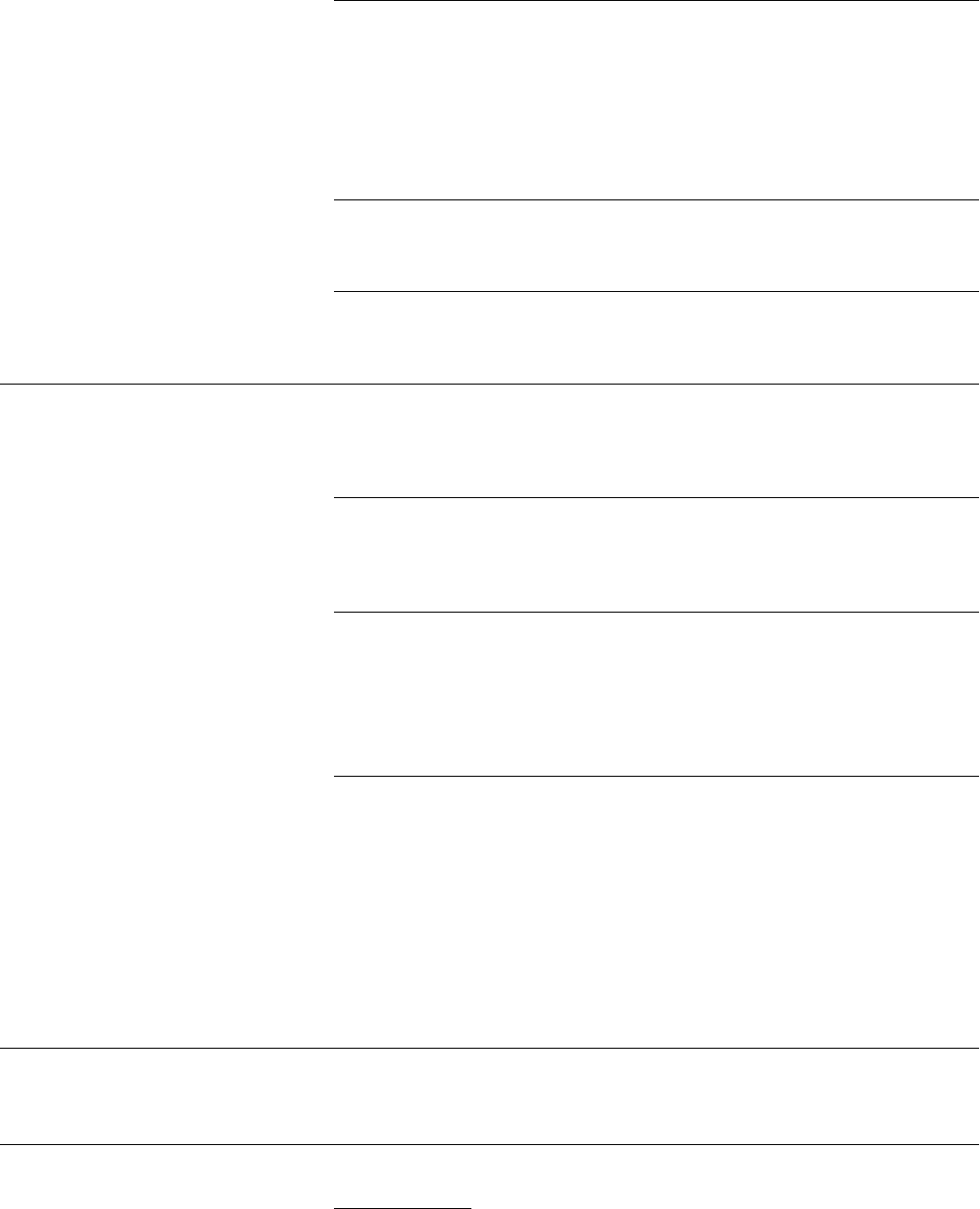
154
Patients should not drive if they experience symptoms at rest or while operating a
motor vehicle.
Physicians should reassess patients for driving tness every six months to two years
as needed, depending on clinical course and control of symptoms. Patients with
functional class III CHF (marked limitation of activity but no symptoms at rest,
working capacity 2 to 4 METS) should be reassessed at least every six months.
Patients who experience syncope or pre-syncope should not drive until they have
been successfully treated.
Patients who experience syncope or pre-syncope or unstable angina should not
drive until the underlying disease is corrected.
Driving restrictions for the following cardiac procedures are based on the patient’s
recovery from the procedure itself and from the underlying disease for which the
procedure was performed.
The patient may resume driving 48 hours to one week after successful PTCA and/
or stenting procedures, depending on the patient’s baseline condition and course of
recovery from the procedure and underlying coronary disease.
217, 218
The patient may resume driving one week after pacemaker implantation if:
The patient no longer experiences pre-syncope or syncope
a. EKG shows normal sensing and capture; and
b. Pacemaker performs within manufacturer’s specications.
219
Driving may usually resume four weeks following coronary artery bypass grafting
(CABG) and/or valve replacement surgery, and within eight weeks following heart
transplant, depending on resolution of cardiac symptoms and the patient’s course of
recovery. In the absence of surgical or post-surgical complications, the main limita-
tion to driving is the risk of sternal disruption following median sternotomy.
If cognitive changes persist following the patient’s physical recovery, cognitive
testing is recommended before the patient is permitted to resume driving. In addi-
tion, on-road testing performed by a driver rehabilitation specialist may be useful in
assessing the patient’s tness to drive.
Please see the recommendations for nonsustained and sustained ventricular tachy-
cardia (2.c and 2.d in this section).
217. Petch, M. C. (1998) European Society of Cardiology Task Force Report: Driving and Heart Disease.
Eur Heart J. 19(8):1165–1177.
218. Consensus Conference, Canadian Cardiovascular Society: Assessment of the cardiac patient for tness to
drive. (1992). Can J Cardiol. 8:406–412.
219. Ibid.
Congestive heart failure (CHF)
with low output syndrome
Hypertrophic obstructive cardiomyopathy
Valvular disease (especially aortic stenosis)
Time-limited restrictions:
cardiac procedures
Percutaneous transluminal coronary
angioplasty (PTCA)
Pacemaker insertion or revision
Cardiac surgery involving median
sternotomy
Internal cardioverter debrillator
Chapter 9—Medical Conditions and Medications That May Affect Driving
155
Section 3:
Cerebrovascular disorders
1. Post intracranial surgery
2. Stroke
3. Transient ischemic attacks (TIA)
4. Subarachnoid hemorrhage
5. Vascular malformation
6. Syncope
Strokes and other insults to the cerebral
vascular system may cause a wide variety
of symptoms, including sensory decits
(e.g., numbness or loss of sensation),
motor decits (e.g., weakness), and
cognitive impairment (e.g., memory,
hemispatial inattention). These symp-
toms range from mild to severe and may
resolve almost immediately or persist for
years. Because each patient is affected
uniquely, the physician must take into
account the individual patient’s constel-
lation of symptoms, severity of symptoms,
course of recovery, and baseline function
when making recommendations con-
cerning driving. Studies have indicated
that a signicant number (>40%) of
community dwelling stroke patients
continue to drive a car.
220
However, the
majority of stroke patients (87 %) may
not receive any type of formal driving
220. Legh-Smith, J., Wade, D. T., & Langton
Hewer, R. L. (1986). Driving after stroke.
J R Soc Med. 79: 200–203.
evaluation, but simply resume the
operation of a motor vehicle.
221
The
larger the presence of a homonymous
visual eld defect, the more likely it is
that the patient will lose his/her driver’s
license. Unfortunately, many patients
may not be aware of this decit.
222
Driving should always be discussed
prior to the patient’s discharge from
the hospital or rehabilitation center.
Patients with residual decits who wish
to resume driving should be referred to a
driver rehabilitation specialist whenever
possible. Although the time frame for
this evaluation will depend on the
severity and extent of the decits, many
evaluations for cognitive and motor
defects will occur somewhere between
three to six months. Upon stabilization
of symptoms, the DRS assesses the
patient for tness-to-drive through
clinical and on-road evaluations. After
assessment, the DRS may recommend
adaptive techniques or adaptive devices
(e.g., wide rear view mirror, spinner
knob for the steering wheel, left foot
accelerator) and provide training for
221. Fisk, G.D., Owsley, C., & Vonne Pulley, L.
(1997). Driving after stroke: driving exposure,
advice, and evaluations. Arch Phys Med Rehabil.
78:1338–1345.
222. Poole, D., Chaudry, F., & Jay, W. M. (2008).
Stroke and driving. Topics Stroke Rehab.
15:37–41.
their proper use. Even patients with
mild decits should undergo driver
evaluation prior to resuming driving, if
possible. Research indicates that a post-
stroke determination of driving safety
made on a medical basis alone may be
inadequate.
223
More recent studies note
associations with impairment on road
tests with measures of perception, visual
selective attention, mental speed, work-
ing memory, executive function and
complex visual-perception/attention
information.
224, 225, 226
For the patient whose symptoms
clearly preclude driving, it should
not be assumed that the patient is
aware that he/she should not drive.
In such cases, the physician should
counsel the patient on driving
cessation.
223. Wilson, T., Smith, T. (1983). Driving after
stroke. Int Rehab Med. 5(4):170–177.
224. Engrum, E.S., Lambert, E. W., & Scott, K.
(1990). Criterion-related validity of the
cognitive behavioral driver’s inventory:
brain injured patients versus normal controls.
Cogn Rehabil. 1990;8:20–26.
225. Lundberg, C., Caneman G.,, Sven-Marten S.,,
et al. (2003). Scand J Psychol. 44:23–30.
226. Nouri F. M., & Lincoln N. B. (1993). Predicting
driving performance after stroke. Br Med J.
307;482–483.
Section 3: Cerebrovascular diseases
The patient should not drive until stabilization or resolution of disease and surgery
symptoms. See also stroke recommendations below (Section 3.2).
Patients with acute, severe motor, sensory, or cognitive decits should refrain from
driving. Depending on the severity of residual symptoms and the degree of recovery,
this restriction may be permanent or temporary.
Upon the patient’s discharge from the hospital or rehabilitation center, the
physician may recommend temporary driving cessation until further neurological
recovery has occurred. Once neurological symptoms have stabilized, physicians
should refer appropriate patients with residual sensory loss, cognitive impairment,
visual eld defects, and/or motor decits to a driver rehabilitation specialist for
driver assessment and rehabilitation. The specialist may prescribe vehicle adaptive
devices and train the patient in their use.
Post intracranial surgery
Stroke
Chapter 9—Medical Conditions and Medications That May Affect Driving
156
Patients with neglect or inattention should be counseled not to drive until
symptoms have resolved and safe driving ability has been demonstrated through
assessment by a driver rehabilitation specialist.
All patients with moderate to severe residual hemiparesis should undergo driver
assessment before resumption of driving. Even if symptoms improve to the extent
that they are mild or completely resolved, patients should still undergo driver
assessment, if available, as reaction time may continue to be affected and other
comorbid conditions could further increase risk.
Patients with aphasia who demonstrate safe driving ability may fail in their efforts
to renew their license due to difculties with the written examination. In these
cases, the physician should urge the licensing authority to make reasonable accom-
modations for the patient’s language decit. A driving rehabilitation specialist may
be able to determine whether the decit is expressive in nature and thus may allow
for interpretation of written (e.g., trafc signs) stimuli. However, trafc signs may
still be interpreted based on color, shape, and symbol recognition.
Patients with residual cognitive decits should be assessed and treated as described in
section 4 on Dementia. Periodic re-evaluation of these patients is recommended, as
some patients may recover sufciently over time to permit safe driving.
Patients who have experienced a single TIA or recurrent TIAs should refrain from
driving until they have undergone medical assessment and appropriate treatment.
Patients should not drive until symptoms have stabilized or resolved. Driving may
resume following medical assessment and, if deemed necessary by the physician,
driver evaluation performed by a driver rehabilitation specialist (including on-road
assessment).
Following the detection of a brain aneurysm or arterio-venous (AV) malformation,
the patient should not drive until he/she has been assessed by a neurosurgeon. The
patient may resume driving if the risk of a bleed is small; an embolization procedure
has been successfully completed; and/or the patient is free of other medical con-
traindications to driving, such as uncontrolled seizures or signicant perceptual or
cognitive impairments.
Syncope usually results from various cardiovascular causes, and is recurrent in up to
30 percent of cases. Cardiac arrhythmias are the most common cause of syncope.
227
(See Section 2 for causes of cardiac syncope.)
Driving restrictions for neurally mediated syncope should be based on the severity
of the presenting event and the anticipant likelihood of recurrence. No driving
restrictions are necessary for infrequent syncope that occurs with warning and with
clear precipitating causes. Patients with severe syncope may resume driving after
adequate control of the arrhythmia has been documented and/or pacemaker follow-
up criteria have been met (see 4 in Section 2).
228
For patients who continue
to experience unpredictable symptoms after treatment with medications and
pacemaker insertion, driving cessation is recommended.
227. Beers, M. H., & Berkow, R. (eds). (1999). The Merck Manual of Diagnosis and Therapy, 17thed.
Whitehouse Station, NJ: Merck and Co., Inc. Section 6, Chapter 200.
228. North American Society of Pacing and Electrophysiology/American Heart Association: Personal and
Public Safety Issues Related to Arrhythmias That May Affect Consciousness: Implications for Regulation
and Physician Recommendations (Part 3 of 4). September 1, 1996.
Stroke (continued)
Transient ischemic attacks (TIA)
Subarachnoid hemorrhage
Vascular malformation
Syncope
Chapter 9—Medical Conditions and Medications That May Affect Driving
157
This is encouraging information that
supports the feasibility and utility of
using this guide.
While it is optimal to initiate discus-
sions of driving safety with the patient
and family members before driving
becomes unsafe, dementia may be unde-
tected and undiagnosed until late in the
course of the disease. Initially, family
members and physicians may assume
that the patient’s decline in cognitive
function is a part of the “normal” aging
process. Physicians may also hesitate
to screen for and diagnose dementia
because they feel that it is futile—in
other words, that nothing can be done
to improve the patient’s situation or
slow disease progression. In addition,
physicians may be concerned about the
amount of time required to effectively
diagnose dementia and educate patients
and their families.
239
However, some pa-
tients are able to achieve cognitive sta-
bility, at least for a period of time, with
cholinesterace inhibitors or N-methyl
d-aspartate (NMDA) receptor block-
ers. In addition, patients are now being
diagnosed on the “cusp” of the disease
in the very early stages. A diagnosis of
dementia by itself should not preclude
driving.
Physician reluctance to screen for
dementia is unfortunate because early
diagnosis is the rst step in promoting
the driving safety of these patients.
The second step is intervention, which
includes medications to slow or stabilize
the course of the disease, counseling to
prepare the patient and family for even-
tual driving cessation, and serial assess-
ment of the patient’s driving abilities.
When assessment shows that driving
may pose a signicant safety risk to the
patient, driving cessation is a neces-
sary third step. With early planning,
patients and their families can make a
more seamless transition from driving to
nondriving status.
239. Valcour, V. G., Masaki, K. H., Curb, J. D., &
Blanchette, P. L. (2000). The detection of
dementia in the primary care setting. Arch
Intern Med. 160:2964–2968.
dementia rating of 1.0).
231
Furthermore,
most patients with Alzhiemer’s disease
will eventually fail subsequent road tests
when followed longitudinally, indicating
that repeat testing at six to twelve months
should be strongly considered.
232
Some
of these studies have led the American
Academy of Neurology to conclude that
patients with a mild level of dementia
severity or greater should no longer
operate an automobile.
233
However,
this recommendation has recently been
challenged by a longitudinal study that
found that some mildly demented drivers
not only passed a performance-based
road test, but also had an acceptable
crash risk prospectively.
234
Furthermore,
recent studies indicate that physician
evaluation in the ofce cannot replace
the on-the-road assessment;
235
however,
tests of working memory and executive
function are improving classication
rates.
236,
237
Finally, a dementia and
driving curriculum modeled after this
AMA guide has been shown to improve
knowledge, attitudes, condence, and
behaviors for health professionals who
deal with older adults with dementia.
238
231. Hunt L., Murphy C., Carr D., Duchek J.,
Buckles V., & Morris, J. (1997). The reliability
of the Washington University Road Test. Arch
Neurol. 54:707–712.
232. Duchek, J. M., Carr DB., Hunt L., et al. (2003).
Longitudinal driving performance in early stage
dementia of the Alzheimer type. J Am Geriatr
Soc. 51:1342–1347.
233. Dubinsky, RM., Stein, AC., Lyons, K. (2000).
Practice parameter: risk of driving and
Alzheimer’s disease (an evidence-based review)
–Report of the Quality Standards Subcommittee
of the American Academy of Neurology.
Neurology. 54, 2205–2211.
234. Ott, BR., Heindel, WC., Papandonatos, GD.,
et al. (2008). Longitudinal study of drivers with
Alzheimer’s disease. Neurology. 70:1171–1178.
235. Ott, B. R., Anthony, D., Papandonatos, G. D.,
D’Abreu, A., Burock, J., Curtin, A., Wu, C. K.,
& Morris, J. C. (2005) Clinician assessment
of the driving competence of patients with
dementia. J Am Geriatr Soc. 53(5):829–833.
236. Grace, J., Amick, M. M., D’Abreu, A., Festa,
E. K., Heindel,W. C., & Ott, B. R. (2005). Neu-
ropsychological decits associated with driving
performance in Parkinson’s and Alzheimer’s
disease. J Int Neuropsychol Soc. 11(6):766–775.
237. Brown, L. B., Stern, R. A., Cahn-Weiner, D.
A., et al. (2005). Driving scenes test of the
Neuropsychological Assessment Battery and on-
road driving performance in aging and very mild
dementia. Arch Clin Neuropsychol. 20:209–215
238. Meuser, T. M., Carr, D. B., Berg-Weger, M.,
Niewoehner, P., & Morris, J. C. (2006). Driving
and dementia in older adults: implementation
and evaluation of a continuing education
project. Gerontologist. 46:680–687.
Section 4:
Neurologic diseases
1. Brain tumor
2. Closed head injury
3. Dementia
4. Migraine and other recurrent
headache syndromes
5. Movement disorders
6. Multiple sclerosis
7. Paraplegia and quadriplegia
8. Parkinson’s disease
9. Peripheral neuropathy
10. Seizure disorder
a. Single unprovoked seizure
b. Withdrawal or change of anti-
epileptic drug therapy
11. Sleep disorders
a. Narcolepsy
b. Sleep apnea
12. Stroke
13. Tourette’s syndrome
14. Vertigo
Dementia deserves special emphasis
in this section because it presents a
signicant challenge to driving safety.
With progressive dementia, patients
ultimately lose the ability to drive safely
and lack insight. Therefore, dementia
patients may be more likely than drivers
with visual or motor decits (who tend
to self-restrict their driving to accom-
modate their declining abilities) to
drive even when it is highly unsafe
for them to be on the road. It becomes
the responsibility of family members
and other caregivers to protect the
safety of these patients by enforcing
driving cessation.
Several recent reviews on this topic
may be of interest to physicians.
229,
230
Fitness-to-drive studies in patients
with dementia indicate that 90 percent
may be able to pass a road test in the
very mild stages of the disease (clinical
dementia rating of 0.5), whereas 40
percent may fail at a mild level of
cognitive impairment (clinical
229. Dobbs, B., Carr, D. B., & Morris, J. C. (2002).
Management and assessment of the demented
driver. Neurologist. 8:61–70.
230. Brown, L. B., & Ott, B. R. (2004). Driving and
dementia: a review of the literature. J Geriatr
Psychiatry Neurol. 17:232–240.
Chapter 9—Medical Conditions and Medications That May Affect Driving
158
Section 4: Neurologic diseases
Driving recommendations should be based on the type of tumor; location; rate of
growth; type of treatment; presence of seizures; and presence of cognitive or percep-
tual impairments. Due to the progressive nature of some tumors, the physician may
need to evaluate the patient’s tness to drive serially.
See also the stroke recommendations in Section 3.2.
If the patient experiences seizure(s), please see the seizure disorder recommendations
below (4.10 in this section).
Patients should not drive until symptoms or signs have stabilized or resolved.
For patients whose symptoms or signs resolve, driving may resume following
medical assessment and, if deemed necessary by the physician, driver evaluation
(including on-road assessment) performed by a driver rehabilitation specialist.
Patients with residual neurological or cognitive decits should be managed as
described in Section 3.
If the patient experiences seizure(s), please see the seizure disorder
recommendations below.
The following recommendations are adapted from the Canadian Consensus
Conference on Dementia and the Alzheimer’s Association Policy Statement on
Driving and Dementia (approved 10/20/01):
• A diagnosis of dementia is not, on its own, a sufcient reason to withdraw
driving privileges. A signicant number of drivers with dementia are found to
be competent to drive in the early states of their illness.
240
Therefore, the
determining factor in withdrawing driving privileges should be the individual’s
driving ability. When the individual poses a heightened risk to self or others,
driving privileges must be withheld.
• Physicians should consider the risks associated with driving for all of their
patients with dementia, and they are encouraged to address the issue of driving
safety with these patients and their families. When appropriate, patients should
be included in decisions about current or future driving restrictions and cessa-
tion; otherwise, physicians and families must decide in the best interests of the
patient whose decision-making capacity is impaired.
• Physicians are recommended to perform a focused medical assessment that includes
a history of any new impaired driving behaviors (e.g., new motor vehicle crashes)
from a family member or caregiver and an evaluation of cognitive abilities, includ-
ing memory, attention, judgment, and visuospatial abilities. Physicians should be
aware that patients with a progressive dementia who are initially believed to be safe
to drive will require serial assessment, and they should familiarize themselves with
their State reporting laws and procedures for dementia (if any). (See Chapter 8 for
a reference list of State reporting laws.)
If concern exists that an individual with dementia has impaired driving ability, and
the individual would like to continue driving, a formal assessment of driving
skills should be administered. One type of assessment is an on-road driving assess-
ment performed by a driver rehabilitation specialist.
240. Carr, D. B., Duchek, J., & Morris, J. C. (2000). Characteristics of motor vehicle crashes with dementia of
the Alzheimer type. J Am Geriatr Soc. 48(1):18–22.
Closed head injury
Brain tumor
Dementia
Chapter 9—Medical Conditions and Medications That May Affect Driving

159
• Physicians should encourage patients with progressive dementia to plan early
for eventual cessation of driving privileges by developing alternative transpor-
tation options. The patient should be encouraged to coordinate these efforts
with his/her family members and caregivers, and to seek assistance (as needed)
from the local Area Agency on Aging.
Patients with recurrent severe headaches should be cautioned against driving
when experiencing neurologic manifestations (e.g., visual disturbances or
dizziness); when distracted by pain; and while on any barbiturate, narcotic,
or narcotic-like analgesic. (See Section 13 for further recommendations
regarding narcotic analgesics.) Patients without a typical aura preceding the
acute attack may be at higher risk.
If the physician elicits complaints of interference with driving tasks or is
concerned that the patient’s symptoms compromise his/her driving safety,
referral to a driver rehabilitation specialist for a driver evaluation (including
on-road assessment) is recommended.
Driving recommendations should be based on the type of symptoms and level
of symptom involvement. Physicians should be alert to decits that may be
subtle (e.g., muscle weakness, sensory loss, fatigue, cognitive or perceptual
decits, symptoms of optic neuritis) but have a strong potential to impair
driving performance.
A driver evaluation (including on-road assessment) performed by a driver
rehabilitation specialist may be useful in determining the patient’s safety to drive.
Serial evaluations may be required as the patient’s symptoms evolve or progress.
Referral to a driver rehabilitation specialist is necessary if the patient wishes to
resume driving and/or requires a vehicle modied to accommodate him/her as a
passenger. The specialist can recommend an appropriate vehicle and prescribe
vehicle adaptive devices (such as low-resistance power steering and hand
controls) and train the patient in their use. In addition, the specialist can assist
the patient with access to the vehicle, including opening and closing car doors,
transfer to the car seat, and independent wheelchair stowage, through vehicle
adaptations and training.
Driving should be restricted until the patient demonstrates safe driving ability in
the adapted vehicle.
Patients with advanced Parkinson’s disease may be at increased risk for motor
vehicle crashes due to both motor and cognitive dysfunction.
241
Physicians
should base their driving recommendations on the level of both motor and
cognitive symptom involvement, patient’s response to treatment, and presence
and extent of any medication side effects. (See Section 13 for specic recom-
mendations on antiparkinsonian medications.) Serial physical and cognitive
evaluations are recommended every six to twelve months due to the progressive
nature of the disease.
241. Zesiewicz, T. A., Cimino, C. R., Malek, A. R., Gardner, N., Leaverton, P. L., Dunne, P. B., & Hauser,
R. A. (2002). Driving safety in Parkinson’s disease. Neurology. 59:1787–1788.
Dementia (continued)
Migraine and other recurrent
headache syndromes
Movement disorders
(e.g., parkinsonism, dyskinesias)
Multiple sclerosis
Paraplegia and quadriplegia
Parkinson’s disease
Chapter 9—Medical Conditions and Medications That May Affect Driving
160
If the physician is concerned that dementia and/or motor impairments may affect
the patient’s driving skills, a driver evaluation (including on-road assessment)
performed by a driver rehabilitation specialist may be useful in determining the
patient’s tness to drive.
Lower extremity decits in sensation and proprioception may be exceedingly
dangerous for driving, as the driver may be unable to control the foot pedals.
If decits in sensation and proprioception are identied, referral to a driver
rehabilitation specialist is recommended. The specialist may prescribe vehicle
adaptive devices (e.g., hand controls in place of the foot pedals) and train the
patient in their use.
The recommendations below (in this section only) are adapted from the Consensus
Statements on Driver Licensing in Epilepsy, crafted and agreed upon by the Ameri-
can Academy of Neurology, American Epilepsy Society, and Epilepsy Foundation of
America in March 1992.
242
Please note that these recommendations are subject to
each particular State’s licensing requirements and reporting laws.
A patient with seizure disorder should not drive until he/she has been seizure-
free for three months. This recommendation appears consistent with recent data.
243
This three-month interval may be lengthened or shortened based on the following
favorable and unfavorable modiers:
Favorable modiers:
• Seizures occurred during medically directed medication changes
• Patient experiences only simple partial seizures that do not interfere with
consciousness and/or motor control
• Seizures have consistent and prolonged aura, giving enough warning to
refrain from driving
• There is an established pattern of purely nocturnal seizures
• Seizures are secondary to acute metabolic or toxic states that are not likely
to recur
• Seizures were caused by sleep deprivation, and sleep deprivation is unlikely
to recur
• Seizures are related to reversible acute illness
242. American Academy of Neurology, American Epilepsy Society, and Epilepsy Foundation of America.
(1994). Consensus Statements, Sample Statutory Provisions, and Model Regulations Regarding Driver
Licensing and Epilepsy. Epilepsia. 35(3):696-705.
243. Drazkowski, J. F., Fisher, R. S., Sirven, J. I., et al. (2003). Seizure-related motor vehicle crashes in Arizona
before and after reducing the driving restriction from 12 to 3 months. Mayo Clin Proc. 78:819-825.
Parkinson’s disease (continued)
Peripheral neuropathy
Seizure disorder
Chapter 9—Medical Conditions and Medications That May Affect Driving
161
Unfavorable modiers:
• Noncompliance with medication or medical visits and/or lack of credibility
• Alcohol and/or drug abuse in the past three months
• Increased number of seizures in the past year
• Impaired driving record
• Structural brain lesion
• Noncorrectable brain functional or metabolic condition
• Frequent seizures after seizure-free interval
• Prior crashes due to seizures in the past ve years
• Single unprovoked seizure
The patient should not drive until he/she has been seizure-free for three months.
This time period may be shortened with physician approval. Predictors of recurrent
seizures that may preclude shortening of this time period include:
• The seizure was focal in origin
• Focal or neurologic decits predated the seizure
• The seizure was associated with chronic diffuse brain dysfunction
• The patient has a positive family history for epilepsy
• Generalized spike waves or focal spikes are present on EEG recordings
The patient should temporarily cease driving during the time of medication
withdrawal or change due to the risk of recurrent seizure and potential medication
side effects that may impair driving ability.
If there is signicant risk of recurrent seizure during medication withdrawal or
change, the patient should cease driving during this time and for at least three
months thereafter.
If the patient experiences a seizure after medication withdrawal or change, he/she
should not drive for one month after resuming a previously effective medication
regimen. Alternatively, the patient should not drive for six months if he/she refuses
to resume this medication regimen, but is seizure-free during this period.
The patient should cease driving upon diagnosis. The patient may resume driving
upon treatment when he/she no longer suffers excessive daytime drowsiness or cata-
plexy. Physicians may consider using scoring tools such as the Epworth Sleepiness
Scale
to assess the patient’s level of daytime drowsiness.
244
See Section 10.
See Section 3.
244. Johns, M. W. (1991). A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale.
Sleep. 14:540–545.
Seizure disorder (continued)
Single unprovoked seizure
Withdrawal or change of
anti-epileptic drug therapy
Sleep disorders
Narcolepsy
Sleep apnea
Stroke
Chapter 9—Medical Conditions and Medications That May Affect Driving
162
In evaluating the patient’s tness to drive, the physician should consider any
comorbid disorders (including attention decit hyperactivity disorder, learning
disabilities, and anxiety disorder) in addition to the patient’s motor tics. (For
specic recommendations on these disorders, see Section 5, Psychiatric Disorders).
If the physician is concerned that the patient’s symptoms compromise his/her
driving safety, referral to a driver rehabilitation specialist for on-road assessment
is recommended.
Physicians should be aware that certain medications used in the treatment
of Tourette’s syndrome have the potential to impair driving performance.
(See Section 13 for more information on medication side effects.)
Vertigo and the medications commonly used to treat vertigo have a signicant
potential to impair driving skills.
For acute vertigo, the patient should cease driving until symptoms have fully
resolved. Under no circumstances should the patient drive to seek medical
attention.
Patients with a chronic vertiginous disorder are strongly recommended to
undergo on-road assessment performed by a driver rehabilitation specialist
prior to resuming driving.
Tourette’s syndrome
Vertigo
Chapter 9—Medical Conditions and Medications That May Affect Driving
163
Section 5:
Psychiatric disorders
1. Affective disorders
a. Depression
b. Bipolar disorder
2. Anxiety disorders
3. Psychotic illness
a. Acute episodes
b. Chronic illness
4. Personality disorders
5. Substance abuse
6. Attention decit disorder (ADD)/
Attention decit hyperactivity
disorder (ADHD)
7. Tourette’s syndrome
Patients in the acute phase of a psy-
chiatric illness need to be aware that
driving skills could be affected. In
general, driving is safe when the condi-
tion is stable, although side effects from
medications and compliance with the
medication regimen may need to be
taken into consideration. (For recom-
mendations on medications and driving,
see Section 13, Medications.)
Psychiatrists may wish to consult the
American Psychiatric Association’s
Position Statement on the Role of Psy-
chiatrists in Assessing Driving Ability
(American Journal of Psychiatry. 1995.
1S2(5):819; also at www.psych.org/
pract_of_psych/driving_pstate.cfm).
Section 5: Psychiatric disorders
Physicians should advise the patient not to drive during the acute phase of illness.
Physicians should also be aware that certain medications used in the treatment of
affective disorders have the potential to impair driving performance. (See Section
13 for more information on medication side effects.)
No restrictions if condition is mild and stable. The physician should always speci-
cally ask about suicidal ideation and cognitive and motor symptoms.
Patients should not drive if they are actively suicidal or experiencing signi-
cant mental or physical slowness, agitation psychosis, impaired attention, and/
or impaired concentration. Patients who seek care for these conditions should be
counseled not to drive themselves to the clinic or hospital.
No restrictions if condition is stable.
Patients should not drive if they are actively suicidal, depressed as in 1.a (above) or
in an acute phase of mania. Patients who seek care for these conditions should be
counseled not to drive themselves to the clinic or hospital.
Patients should not drive during severe episodes of anxiety. Otherwise, there are no
restrictions if the condition is stable.
Physicians should also be aware that certain medications used in the treatment of
anxiety disorders have the potential to impair driving performance. (See Section
13 for more information on medication side effects.)
Affective disorders
Depression
Bipolar disorder
Anxiety disorders
Chapter 9—Medical Conditions and Medications That May Affect Driving
164
Physicians should advise the patient not to drive during the acute phase(s) of
illness. Physicians should also be aware that medications used in the treatment of
psychotic illness have the potential to impair driving performance. (See Section 13
for more information on medication side effects.)
Patients should not drive during acute episodes of psychosis. Patients who seek care
for acute psychosis should be counseled not to drive themselves to the clinic or
hospital.
No restrictions if the condition is stable and there are no other factors
(e.g., medication side effects) that can affect driving performance.
No restrictions unless the patient has a history of driving violations and his/her psy-
chiatric review is unfavorable. This includes—but is not limited to—uncontrolled
erratic, violent, aggressive or irresponsible behavior.
Due to the high comorbidity of substance abuse with personality disorders,
physicians are urged to be alert to substance abuse in these patients and counsel
them accordingly (see recommendations for substance abuse below).
Driving while intoxicated is not only highly dangerous to the driver, passengers,
and other road users, but it is also illegal. Drunk driving is the most common crime
in the United States, and it is responsible for thousands of trafc deaths each year.
Alcohol is not the only cause of intoxicated driving. Substances including, but not
limited to, marijuana, cocaine, amphetamines (including amphetamine analogs),
opiates, and benzodiazepines may also impair driving skills.
Physicians should follow up all positive screens with appropriate interventions, in-
cluding brief interventions or referral to support groups, counseling, and substance
abuse treatment centers. Physicians should strongly urge substance abusers to tem-
porarily cease driving while they seek treatment, and to refrain from driving while
under the inuence of intoxicating substances. A nonjudgmental and supportive
attitude and frequent follow-up may aid substance abusers in their efforts to achieve
and maintain sobriety.
Physicians should also familiarize themselves with any State laws holding them
responsible for detaining intoxicated patients who have driven to the hospital or
clinic until they are legally unimpaired.
A recent review noted increased risk of driving behaviors and a positive effect
of stimulant medications on driving performance.
245
Physicians should educate
their patients about the increased risk associated with the disease and the potential
benets of treatment.
See Section 4.
245. Barkley, R. A., & Cox, D. (2007). A review of driving risks and impairments associated with
attention-decit/hyperactivity disorder and the effects of stimulant medication on driving
performance. Journal of Safety Research. 38(1):113–28.
Psychotic illness
Acute episodes
Chronic illness
Personality disorders
Substance abuse
Attention Decit Disorder/Attention
Decit Hyperactivity Disorder
Tourette’s syndrome
Chapter 9—Medical Conditions and Medications That May Affect Driving
165
Section 6: Metabolic disorders
1. Diabetes mellitus
a. Insulin dependent diabetes
mellitus (IDDM)
b. Non-insulin dependent diabetes
mellitus (NIDDM)
2. Hypothyroidism
3. Hyperthyroidism
Individuals in the acute phase of a
metabolic disorder (e.g., diabetes,
Cushing’s disease, Addison’s disease,
hyperfunction of the adrenal medulla,
and thyroid disorders) may experience
signs and symptoms that are incompat-
ible with safe driving. Physicians should
advise these individuals to refrain from
driving (including driving to seek
medical attention) until the symptoms
have abated. There are data that suggest
that older diabetic patients may be at
increased risk for impaired driving, but
the literature is not consistent in this
area. Concern has been raised that the
trend in the medical profession has
been toward tighter control, which
could result in hypoglycemia and
possibly increased crash risk.
Section 6: Metabolic disorders
No restrictions if the patient demonstrates satisfactory control of his/her
diabetes, recognizes the warning symptoms of hypoglycemia, and meets
required visual standards.
The major concerns with insulin dependent diabetics are hypoglycemia unawareness.
There are several studies that have noted that patients with type 1 IDDM had
impaired driving performance during episodes of hypoglycemia and were unaware
of their low blood sugars at the time of driving assessment.
246, 247
It is apparent from these studies that many drivers did not take appropriate action
even when they recognized the symptoms of hypoglycemia. Diabetic patients who
use insulin should be evaluated for hypoglycemia and should consider checking
their blood sugar before driving or on prolonged trips. This is especially the case
for individuals who have exhibited hypoglycemia unawareness (e.g., documented
blood sugars below 60 mg/dL without symptoms).
Patients should be counseled not to drive during acute hypoglycemic or hypergly-
cemic episodes. In addition, patients are advised to keep candy or glucose tablets
within reach in their car at all times, in the event of a hypoglycemic attack.
For peripheral neuropathy, see Section 4.
Patients who experience recurrent hypoglycemic or hyperglycemic attacks should
not drive until they have been free of signicant hypoglycemic or hyperglycemic
attacks for three months.
Patients who are managed by lifestyle changes and/or oral medications have no
restrictions unless they develop relevant disabilities (e.g., diabetic retinopathy).
If the physician prescribes an oral medication that has a signicant potential to
cause hypoglycemia, he/she should counsel the patient as above. Oral medications
may also increase the likelihood of hypoglycemia, which should be managed as in
1.a in this section.
246. Weinger, I., Kinsley, B. T., Levy, C. J., et al. (1999). The perception of safe driving ability during
hypoglycemia in patients with type I diabetes. Am J Med. 107:246–253.
247. Cox, D. J., Gonder-Frederick, L. A., Kovatchev, B. P., et al. (2000). Progressive hypoglycemia’s impact on
driving simulation performance: occurrence, awareness, and correction. Diabetes Care. 23:163–170.
Diabetes mellitus
Insulin dependent diabetes mellitus
(IDDM)
Non-insulin dependent diabetes mellitus
(NIDDM)
Chapter 9—Medical Conditions and Medications That May Affect Driving
166
Patients who experience symptoms (e.g., cognitive impairment, drowsiness, and
fatigue) that may compromise safe driving should be counseled not to drive until
their hypothyroidism has been satisfactorily treated. If residual cognitive decits
are apparent despite treatment, a driver evaluation (including on-road assessment)
performed by a driver rehabilitation specialist may be useful in determining the
patient’s ability to drive safely.
Patients who experience symptoms (e.g., anxiety, tachycardia, palpitations, etc.)
should be counseled not to drive until their hyperthyroidism has been satisfactorily
treated and symptoms have resolved.
Hypothyroidism
Hyperthyroidism
Chapter 9—Medical Conditions and Medications That May Affect Driving
167
at-fault crash risk in a recent study.
256
Similarly, an examination of medically
impaired drivers in Utah found an
increased crash risk for drivers with
musculoskeletal disorders, but not for
those with muscle or motor weakness.
257
Conversely, patients with a specic
diagnosis of osteoarthritis
258
were no
more at risk for a crash than controls in
one study. Also reassuring was a recent
study noting no increase in crash risk of
drivers with cars that had been adapted
for their musculoskeletal restrictions.
259
Thus, physicians can play a role in
diagnosing, managing, and referring
their patients with musculoskeletal
disorders and, ideally, play a role in
maintaining driving privileges and
improving trafc safety.
Rehabilitative therapies such as physical
or occupational therapy and/or a con-
sistent regimen of physical activity may
improve the patient’s ability to drive
and overall level of physical tness.
Whenever possible, the use of narcotics,
barbiturates, and muscle relaxants
should be avoided or minimized in
those patients with musculoskeletal
disabilities who wish to continue
driving. See Section 13 for
recommendations on specic
classes of medications.
256. McGwin, G., Sims, R. V., Pulley, L., et al.
(2000). Relations among chronic medical
conditions, medications, and automobile crashes
in the elderly: a population-based case-control
study. Am J Epidemiol. 152: 424-431.
257. Vernon, D. D., Diller, E. M., Cook, L. J., et
al. (2002). Evaluating the crash and citations
rates of Utah drivers licensed with medical
conditions, 1992-1996. Accid Anal Prev. 34:
237-246.s
258. Koepsell, T., Wolf, M. , & McCloskey, L.
(1994). Medical conditions and motor vehicle
collision injuries in older adults. J Am Geriatr
Soc. 42,695-700.
259. Henriskkson, P. (2001). Drivers with Dis-
abilities: A Survey of Adapted Cars, Driving
Habits and Safety. VTI rapport 466. Linkoping,
Sweden: Swedish National Road and Transport
Research Institute.
pedal.
248
Driving impairment has been
correlated with the inability to reach
above the shoulder.
249
Older adults with
physical frailty or disabilities may be at
increased risk for a crash,
250,
251
and are
more likely to be injured.
252
Presence
of foot abnormalities, walking less
than one block a day, and impaired left
knee exion have been associated with
adverse driving events.
253
In one study,
older crash-involved subjects were
more likely to have difculty walking
one-quarter mile than controls; and the
authors also noted an increased crash
risk for drivers with a history of falls.
254
Diminished cervical range of motion
and a slowed rapid pace walk have
also been recently associated with an
increased crash risk.
255
The use of nonsteroidal anti-inamma-
tory agents (NSAIDs) and a diagnosis of
arthritis were associated with increased
248. Jones, J. G., McCann, J., & Lassere, M. N.
(1991). Driving and arthritis. Br J Rheumatol.
1991;30:361-364.
249. Hu, PS., Trumble, DA., Foley, DJ., et al. (1998).
Crash risks of older drivers: a panel data analysis
Accid Anal Prev. 30:569-581.
250. Sims, R. V., McGwin, G., Allman, R. M., et al.
(2000). Exploratory study of incident vehicle
crashes among older drivers. J Gerontol Series A
Bio Sci Med Sci. 55:M22-27.
251. Marottoli, R. A., Wagner, D. R., Cooney, L. M.,
& Tinetti, M. E. (1994). Predictors of crashes
and moving violations among elderly drivers.
Ann Intern Med. 1994;121:842-846.
252. Kent, R., Funk, J., &Crandall, J. (2003). How
future trends in societal aging, air bag avail-
ability, seat belt use, and eet composition will
affect serious injury risk and occurrence in the
United States. Traff Inj Prev. 4:24-32.
253. Marottoli, R. A., Wagner, D. R., Cooney, L. M.,
& Tinetti, M. E. (1994). Predictors of Crashes
and Moving Violations Among Elderly Drivers.
Ann Int Med 121: 842-846.
254. Sims, R. V., McGwin, G., Pulley, L., et al.
(2001). Mobility impairments in crash-involved
drivers. J Aging Health. 12:430.s.
255. Ball, K. K., Roenker, D. L., Wadley, V. G., et al.
(2006). Can high-risk older drivers be identied
through performance-based measures in a
Department of Motor Vehicles setting? J Am
Geriatr Soc. 54:77-84.
Section 7:
Musculoskeletal disabilities
1. Arthritis
2. Foot abnormalities
3. Limitation of cervical movement
4. Limitation of thoracic and
lumbar spine
5. Loss of extremities or loss of use
of extremities
6. Muscle disorders
7. Orthopedic procedures/surgeries
a. Amputation
b. Anterior cruciate ligament
(ACL) reconstruction
c. Limb fractures and treatment
involving splints and casts
d. Rotator cuff repair—open or
arthroscopic
e. Shoulder reconstruction
f. Total hip replacement
g. Total knee arthroplasty (TKA)
The pain, decrease in motor strength,
and compromised range of motion
associated with musculoskeletal disabili-
ties can affect an individual’s ability to
drive. Physicians should encourage their
patients with musculoskeletal disabilities
to drive a vehicle with power steering
and automatic transmission, if they do
not already do so. Such vehicles require
the least amount of motor ability for
operation among all standard vehicles.
If the physician is concerned that the
patient’s musculoskeletal disabilities im-
pair his/her driving performance, referral
to a driver rehabilitation specialist for
a driver evaluation (including on-road
assessment) is also recommended. In
addition to assessing the patient’s driving
skills, the specialist can prescribe adap-
tive techniques and devices and train the
patient in their use.
Patients with musculoskeletal disorders,
typically have problems with seat belt
and ignition key use, adjusting mirrors
and seats, in steering, in transferring in
and out of the car, in driving in reverse,
and in using the controls like the foot
Chapter 9—Medical Conditions and Medications That May Affect Driving
168
If symptoms of arthritis compromise the patient’s driving safety, referral to a
physical or occupational therapist for rehabilitative therapy and/or to a driver
rehabilitation specialist for driver evaluation (including on-road assessment)
is recommended. The specialist may prescribe vehicle adaptive devices and train
the patient in their use.
See below for specic recommendations on limitation of cervical movement or
limitation of the thoracic or lumbar spine.
Foot abnormalities (e.g., bunions, hammer toes, long toe nails, and calluses) that
affect the patient’s dorsiexion, plantar exion and/or contact with vehicle foot
pedals should be addressed and treated, if possible. Consideration should be given
to referral to a podiatrist. The physician may also refer the patient to a driver
rehabilitation specialist, who can prescribe vehicle adaptive devices and train the
patient in their use.
Some loss of head and neck movement is acceptable if the patient has sufcient
combined rotation and peripheral vision to accomplish driving tasks (e.g., turning,
crossing intersections, parking, backing up) safely. The physician may also refer the
patient to physical or occupational therapist for rehabilitative therapy, and/or to a
driver rehabilitation specialist, who can prescribe wide-angled mirrors and train the
patient in their use.
Patients with marked deformity, who wear braces or body casts, or who have pain-
fully restricted motion in their thoracic or lumbar regions should be referred to a
driver rehabilitation specialist. The specialist can prescribe vehicle adaptive devices
such as raised seats and wide-angled mirrors, and train the patient in their use. The
specialist can also prescribe seat belt adaptations as needed to improve the patient’s
safety and comfort, and ensure that the patient is seated at least 10 inches from the
vehicle air bags.
Patients with acute spinal fractures, including compression fractures, should not
drive until the fracture has been stabilized and painful symptoms cease to interfere
with control of the motor vehicle. These types of fractures can be extremely painful
and require large doses of narcotics for control of pain, which also can increase risk.
(For paraplegia or quadriplegia, see Section 4.)
For patients who have lost (or lost the use) of one or more extremities, referral
to a driver rehabilitation specialist is highly recommended. These specialists can
prescribe vehicle adaptive devices and/or adaptations to limb prostheses, and train
the patient in their use.
Note that the use of articial limbs on vehicle foot pedals is unsafe because there
is no sensory feedback (i.e., pressure and proprioception). For these patients,
specialized hand controls in place of pedals are required.
Driving should be restricted until the patient demonstrates safe driving ability
(with the use of adaptive devices, as needed).
Section 7: Musculoskeletal disabilities
Arthritis
Foot abnormalities
Limitation of cervical movement
Limitation of thoracic or lumbar spine
Loss of extremities or loss of
use of extremities
Chapter 9—Medical Conditions and Medications That May Affect Driving
169
If the physician is concerned that the patient’s symptoms compromise his/her driv-
ing safety, referral to a driver rehabilitation specialist for driver evaluation (includ-
ing on-road assessment) is recommended. If needed, the specialist may prescribe
vehicle adaptive devices and train the patient in their use.
See Loss of extremities (previous page).
Should not drive for four weeks following right ACL reconstruction. If the patient
drives a vehicle with manual transmission, he/she should not drive for four weeks
following right or left ACL reconstruction.
260
No restrictions if the fracture or splint/cast does not interfere with driving tasks.
If the fracture or splint/cast interferes with driving tasks, the patient may resume
driving after the fracture heals or the splint/cast is removed, upon demonstration
f the necessary strength and range of motion.
Should not drive for four to six weeks following rotator cuff repair. If the patient’s
vehicle does not have power steering, the waiting period may be much longer.
Physicians should counsel patients to wear their seat belts properly (over the
shoulder, rather than under the arm) whenever they are in a vehicle as a driver or
passenger.
Should not drive for four to six weeks following shoulder reconstruction. If the
patient’s vehicle does not have power steering, the waiting period may be much
longer.
Physicians should counsel patients to wear their seat belts properly (over the
shoulder, rather than under the arm) whenever they are in a vehicle as a driver or
passenger.
Should not drive for at least four weeks following right total hip replacement.
If the patient drives a vehicle with manual transmission, he/she should not drive
for at least four weeks following right or left total hip replacement.
Physicians should counsel patients to take special care when transferring into
vehicles and positioning themselves in bucket seats and/or low vehicles, either
of which may result in hip exion greater than 90 degrees. Physicians should also
counsel patients that reaction time may not return to baseline until eight weeks
after the surgery, and that they should exercise extra caution while driving during
this period.
261
260. Gotlin, R. S., et al. (2000). Measurement of brake response time after right anterior cruciate ligament
reconstruction. Arch Physical Med Rehabil. 81(2):201-204.
261. MacDonald, W., & Owen, J. W. (1988). The effect of total hip replacement on driving reactions. J Bone
Joint Surg. 70B(2):202-205
Muscle disorders
Orthopedic procedures/surgeries
Amputation
Anterior cruciate ligament (ACL)
reconstruction
Limb fractures and treatment involving
splints and casts
Rotator cuff repair—open or arthroscopic
Shoulder reconstruction
Total hip replacement
Chapter 9—Medical Conditions and Medications That May Affect Driving
170
Should not drive for three to four weeks following right TKA. If the patient drives
a vehicle with manual transmission, he/she should not drive for three to four weeks
following right or left TKA.
262
The physician should also counsel patients that reaction time may not return to
baseline until eight weeks after the surgery, and that they should exercise extra
caution while driving during this period.
263
262. Pierson, J. L., Ramsey, J., Clayton, R. T., & Stippich, K. T. (February 7, 1999). TKA improves drivers’
brake reaction time. The American Academy of Orthopaedic Surgeons: Academy News.
263. Spalding, T. J., Kiss, J., Kyberd, P., Turner-Smith, A., & Simpson, A. H. (1994). Driver reaction times
after total knee replacement. J Bone Joint Surg Br. 76(5):754–756.
Total knee arthroplasty (TKA)
Chapter 9—Medical Conditions and Medications That May Affect Driving

171
Section 8:
Peripheral vascular diseases
1. Aortic aneurysm
2. Deep vein thrombosis (DVT)
3. Peripheral arterial aneurysm
Section 8: Peripheral vascular diseases
No restrictions to driving unless other disqualifying conditions are present. Indi-
viduals whose aneurysm appears to be at the stage of imminent rupture based on
size, location, and/or recent change should not drive until the aneurysm has been
repaired, if possible.
Patients with acute DVT may resume driving when their international normal-
ized ratio (INR) is therapeutic (or the risk of embolism is otherwise appropriately
treated), and they can demonstrate adequate ankle dorsiexion.
The physician should advise individuals with a history of DVT to take frequent
“mobilization breaks” when driving long distances.
No restrictions unless other disqualifying conditions are present. Patients whose an-
eurysm appears to be at the stage of imminent rupture based on size, location, and/
or recent change should not drive until the aneurysm has been repaired, if possible.
Aortic aneurysm
Deep vein thrombosis (DVT)
Peripheral arterial aneurysm
Chapter 9—Medical Conditions and Medications That May Affect Driving
172
Section 9: Renal disease
1. Chronic renal failure
2. Renal transplant
Section 9: Renal disease
No restrictions unless the patient experiences symptoms that are incompatible with
safe driving (e.g., cognitive impairment, impaired psychomotor function, seizures,
or extreme fatigue from anemia). If the physician is concerned that the patient’s
symptoms compromise his/her driving safety, referral to a driver rehabilitation
specialist for a driver evaluation (including on-road assessment) is recommended.
Many patients with renal failure requiring hemodialysis can drive without restric-
tion. However, management of renal failure requires that the patient be compliant
with substantial nutrition and uid restrictions, frequent medical evaluations, and
regular hemodialysis treatments. Patients with a history of noncompliance should
be advised against driving. Furthermore, certain medications used to treat side
effects of hemodialysis may be substantially impairing (e.g., diphenhydramine for
dialysis-associated pruritis), and dialysis itself may result in hypotension, confusion,
or agitation in many patients. These effects may require that patients avoid driving
in the immediate post-dialysis period.
Patients may resume driving four weeks following successful transplant on the
recommendation of the physician.
.
Chronic renal failure
Renal transplant
Chapter 9—Medical Conditions and Medications That May Affect Driving

173
sleep.
264
Sleep disorder crash risk may be
elevated further by medication use, such
as narcotics or antihistamine.
265
Sleep
apnea patients have been noted to have
as high as a seven-fold increased crash
risk compared to controls depending
on the study.
266
Patients may also be at
increased risk for serious injury.
267
This
264. Garharino, S., Nohili, L., Beelke, M., De Carli,
F., & Ferrillo, F. (2001). The contributing role of
sleepiness in highway vehicle accidents. Sleep.
24:203-206.
265. Howard, M.E., et al. ( 2004). Sleepiness, sleep-
disordered breathing and accident risk factors
in commercial vehicle drivers. Am J Respir Crit
Care Med. 170:1014-1021.
266. Teran-Santos, J., Jimenez-Gomez, A., &
Cordero-Guevara, J. (1999). The association
between sleep apnea and the risk of trafc ac-
cidents. Cooperative Group Burgos-Santander.
N Engl J Med. 340(11):847-851.
267. Medical News Today. (n.a.) Risk of severe
car crashes greatly increased in sleep apnea
patients. http://www.medicalnewstoday.com/
articles/71543.php.
Section 10:
Respiratory diseases
1. Asthma
2. Chronic obstructive pulmonary
disease (COPD)
3. Sleep apnea
“Drowsy driving” or driving with fatigue
or sleepiness is a common cause for a
motor vehicle crash, and some estimate
that more than 100,000 crashes a year
may be attributed to this problem.
Crash risk increases with diminishing
Section 10: Respiratory diseases
topic has been extensively reviewed
elsewhere.
268
Obstructive sleep apnea
is one of the few medical conditions
where treatment has been shown to
reduce crash risk back to baseline lev-
els.
269
In addition, recent studies indi-
cate a high prevalence of sleep disorders
or daytime sleepiness in older adults
270
and in diabetic patients.
271
268. Charlton, J., et al. (2004). Inuence of chronic
illness on crash involvement of motor vehicle
drivers, Monash University Accident Research
Centre, Report No. 213.
269. George, C. F. (2001). Reduction in motor
vehicle collisions following treatment of sleep
apnea with nasal CPAP. Thorax. 56(7):508-512.
270. Vaz Fragoso, Arauio, K. L., Van Ness, P. H., &
Marottoli, R. A. (2008). Prevalence of sleep
disturbances in a cohort of older drivers. J
Gerontol Series A Bio Sci Med Sci. 63:715-723.
271. Hayashino, Y., Yamazaki, S., Nakayama, T.,
et al. (2008). Relationship between diabetes
mellitus and excessive sleepiness during driving.
Exp Clin Endocrinol Diabetes. 116:1-5.
No restrictions.
Patients should be counseled not to drive during acute asthma attacks, or while
suffering transient side effects (if any) from their asthma medications.
No restrictions if symptoms are well controlled, and the patient does not
experience any signicant side effects from the condition or the medication.
The patient should not drive if he/she suffers dyspnea at rest or at the wheel (even
with the use of supplemental oxygen), excessive fatigue, or signicant cognitive
impairment. If the patient requires supplemental oxygen to maintain a hemoglobin
saturation of 90 percent or greater, he/she should be counseled to use the oxygen
at all times while driving. Due to the often tenuous oxygenation status of these
patients, they should also be counseled to avoid driving when they have other re-
spiratory symptoms that may indicate concomitant illness or exacerbation of COPD
(e.g., new cough, increased sputum production, change in sputum color, fever).
Because COPD is often progressive, periodic reevaluation for symptoms and
oxygenation status is recommended.
If the physician is concerned that the patient’s symptoms compromise his/her
driving safety, referral to a driver rehabilitation specialist for a driver evaluation
(including on-road assessment) is recommended. The patient’s oxygen saturation
may be measured during the course of the on-road assessment to provide additional
information for patient management.
Asthma
Chronic obstructive pulmonary
disease (COPD)
Chapter 9—Medical Conditions and Medications That May Affect Driving
174
Patients with excessive daytime sleepiness, loud snoring (particularly if accompa-
nied by witnessed apneic events), large neck circumference (≥ 16 inches in women,
≥ 17 inches in men), elevated body mass index (above 35 kg/m2), and/or hyperten-
sion that requires two or more medications should be considered at risk for obstruc-
tive sleep apnea, and formal sleep study evaluation should be considered, especially
in any patient who reports having fallen asleep while driving a vehicle. A patient
diagnosed with sleep apnea (apnea/hypopnea index of 5 or greater) who has fallen
asleep while driving, or a patient with severe obstructive sleep apnea (apnea/hypo-
pnea index of 30 or greater) should be counseled to refrain from driving until he/
she is receiving effective treatment (via a positive airway pressure device) following
a formal sleep study to conrm the diagnosis. If these patients undergo other treat-
ments (surgery, oral appliances), they should be advised to have a post-treatment
sleep study to conrm effectiveness. Physicians should counsel patients using posi-
tive airway pressure devices that they should not drive if they do not use the device
unless a formal sleep study conrms resolution of their obstructive sleep apnea
(e.g., following substantial weight loss).
Sleep apnea
Chapter 9—Medical Conditions and Medications That May Affect Driving
175
cognitive impairment, and/or analge-
sics. (For specic recommendations
on musculoskeletal restrictions and
narcotic analgesics, please see Sections
7 and 13, respectively.)
In counseling patients about their
return to driving after a surgical
procedure, it is useful to ask whether
the patient’s car has power steering
and automatic transmission. Physicians
can tailor their advice accordingly.
As patients resume driving, they should
be counseled to assess their comfort
level in familiar, trafc-free areas before
driving in heavy trafc. If the patient
feels uncomfortable driving in certain
situations, he/she should avoid these
situations until his/her condence level
has returned. A patient should never
resume driving before he/she feels ready
to do so and has received approval from
the physician.
• Pre-existing cognitive impairment
• Duration of surgery
• Age (over 60)
• Altered mental status post-surgery
• Presence of multiple comorbidities
• Emergency surgery
If the physician is concerned that
residual visual, cognitive or motor
decits following surgery may impair the
patient’s driving performance, referral
to a driver rehabilitation specialist for
a driver evaluation (including on-road
assessment) is highly recommended.
Physicians should counsel patients who
undergo surgery—both inpatient and
outpatient—not to drive themselves
home following the procedure. Although
they may feel capable of driving, their
driving skills may be affected by pain,
physical restrictions, anesthesia,
Section 11:
Effects of anesthesia
and surgery
1. Abdominal, back, and chest surgery
2. Anesthesia
a. General
b. Local
c. Epidural
d. Spinal
3. Neurosurgery
4. Orthopedic surgery
Physicians should be alert to peri- and
post-operative risk factors that may
affect the patient’s cognitive function
post-surgery, or restrictions on limb
movement or joint range of motion that
place the patient at risk for impairments
in driving performance. Risk factors
include:
Section 11: Effects of anesthesia and surgery
The patient may resume driving after demonstrating the necessary strength and
range-of-motion for driving.
See Section 2 for recommendations for surgeries involving median sternotomy.
Because anesthetic agents and adjunctive compounds (such as benzodiazepines)
may be administered in combination, the patient should not resume driving until
the motor and cognitive effects from all anesthetic agents have subsided.
Both the surgeon and anesthesiologist should advise patients against driving for at
least 24 hours after a general anesthetic has been administered. Longer periods of
driving cessation may be recommended depending on the procedure performed and
the presence of complications.
If the anesthetized region is necessary for driving tasks, the patient should not
drive until he/she has recovered full strength and sensation (barring pain).
The patient may resume driving after recovering full strength and sensation
(barring pain) in the affected areas.
The patient may resume driving after recovering full strength and sensation
(barring pain) in the affected areas.
Abdominal, back and chest surgery
Anesthesia
General
Epidural
Spinal
Local
Chapter 9—Medical Conditions and Medications That May Affect Driving
176
See recommendations for post intracranial surgery in Section 3.
See the recommendations for orthopedic procedures/surgeries in Section 7.
Neurosurgery
Orthopedic surgery
Chapter 9—Medical Conditions and Medications That May Affect Driving
177
Section 12:
Miscellaneous conditions
1. Cancer
Section 12: Miscellaneous conditions
Patients who experience signicant motor weakness or cognitive impairments
from the cancer itself, metastases, cachexia, anemia, radiation therapy, and/or
chemotherapy, which can cause cognitive impairment and/or neuropathy,
should cease driving until their condition improves and stabilizes.
Many medications prescribed to relieve the side effects of treatment
(e.g., antiemetics for nausea) may impair driving performance. Physicians
should counsel their patients accordingly. (See Section 13 for
recommendations for specic medications.)
Cancer
Chapter 9—Medical Conditions and Medications That May Affect Driving
178
available on-line.
278
Medication side effects that can affect
driving performance include drowsiness,
dizziness, blurred vision, unsteadiness,
fainting, slowed reaction time, and ex-
trapyramidal side effects. In many cases,
these side effects are dose-dependent
and may attenuate with time.
Whenever possible, the physician
should prescribe non-impairing medica-
tions. If the physician must prescribe
or change the dosage of a medication
that can potentially impair driving
performance, he/she should counsel
the patient about the side effects. The
physician should also recommend that
the patient take the rst few doses in a
safe environment to determine the pres-
ence and extent of any side effects, and
that he/she temporarily cease driving as
needed until the body has adjusted to
the medication.
In addition to being alert to potential
side effects, the patient, caregivers,
and physicians should also understand
that with certain medications, subjec-
tive effects do not always correlate
with impairment.
279
Medications that
cause drowsiness, euphoria, and/or
anterograde amnesia may also diminish
insight, and the patient may experience
impairment without being aware of it.
278. Walgreens Health Services. Continuing
Pharmacy Education Web Site. Medication-
Related Impaired Driving: For Pharmacist.
https://webapp.walgreens.com/cePharmacy/
programsHTML/transportation-tech.pdf. Accessed
November 16, 2007.
279. Mattila, M. (1988). Acute and subacute effects
of diazepam on human performance: comparison
of plain tablet and controlled release capsule.
Pharmacol Toxicol. 63(5):369–374.
Roache, JD., & Grifths, R. R. (1985).
Comparison of triazolam and pentobarbital:
performance
impairment, subjective effects and abuse liability.
J Pharmacol Exp Therapeut. 234(1):120–133.
Aranko, K., Mattila, M. J., & Bordignon, D.
(1985). Psychomotor effects of alprazolam and
diazepam during acute and subacute treatment,
and during the follow-up phase. Acta Pharmaco-
logica Toxicologica. 56(5):364–372.
Weiler, JM., et al. (2000). Effects of fexofena-
dine, diphenhydramine, and alcohol on driving
performance. a randomized placebo-controlled
trial in the Iowa Driving Simulator. Ann Intern
Med. 132(5):354–363.
older adults may be driving while under
the inuence of other medications.
273,
274
Potential driving impairing (PDI) medi-
cations is a relatively new term that
identies medications that have been
associated with increased crash risk.
Crash risk does increase when multiple
PDI drugs are prescribed.
275
Mechanisms
whereby drugs may impair driving are
myriad and include: sleepiness, fatigue,
or sedation; lightheadness, dizziness,
or low blood pressure; blackouts or
syncope; or impaired judgment coordi-
nation. Medications can affect eyesight
in numerous ways, including blurred
vision, impaired visual elds, and
nighttime vision.
276
However, it should
be noted that many medication and
driving studies are usually correlational
in nature, and may suggest increased
crash risk but not necessarily causation.
Whether it is the medication itself, the
condition for which it is prescribed,
the presence of other comorbidities, or
a combination of these issues is often
difcult to sort out.
277
Clinicians should
be aware of the risk and attempt to use
the safest class of medications based on
the most recent evidence. An excellent
review of this subject for pharmacists
may be of interest to physicians and is
273. Higgins, J. P., Wright, S. W., & Wrenn, K. D.
(1996). Alcohol, the elderly, and motor vehicle
crashes. Am J Emerg Med. 14:265–267.
274. Johansson, K., Bryding, G., Dahl, M. L., et
al.(1997). Trafc dangerous drugs are often
found in fatally injured older male drivers. J Am
Geriatr Soc. 45:1029–1031.
275. Leroy, A., & Morse, M. M. (N.A.). Exploratory
Study of the Relationship Between Multiple
Medications and Vehicle Crashes: Analysis
of Databases. NHTSA Contract DTNH22-
02-C-05075. Publication under review.
[Published as Multiple Medications and Vehicle
Crashes: Analysis of Databases. (2008, May).
NHTSA Report No. DOT HS 810 858. Wash-
ington, DC: National Highway Trafc Safety
Administration. Available at www.nhtsa.dot.gov/
staticles/DOT/NHTSA/Trafc%20Injury%20
Control/Articles/Associated%20Files/810858.pdf.]
276. Wang, K.(2007). Adverse Ocular Side-Effects
of Commonly Prescribed Systemic Medications.
Online CE provided by Pacic University
College of Optometry. www.Opt.pacifcu.edu/ce/
catalog/11466-PHWandgDrugs.html. Accessed
October 21, 2007.
277. Bramness, JG., Skurtvelt, S., Neutel, CI., et
al. (2008). Minor increase in trafc accidents
after prescriptions of antidepressants: a study
of population registry data in Norway. J Clin
Psychiatry. 69:1099–1103.
Section 13: Medications
1. Alcohol
2. Anticholinergics
3. Anticonvulsants
4. Antidepressants
a. Bupropion
b. Mirtazapine
c. Monoamine oxidase
(MAO) inhibitors
d. Selective serotonin reuptake
inhibitors (SSRIs)
e. Tricyclic antidepressants (TCAs)
5. Antiemetics
6. Antihistamines
7. Antihypertensives
8. Antiparkinsonians
9. Antipsychotics
10. Benzodiazepines and other
sedatives/anxiolytics
11. Muscle relaxants
12. Nonsteroidal anti-inammatory
drugs (NSAIDs)
13. Narcotic analgesics
14. Stimulants
Many commonly used prescription
and over-the-counter medications can
impair driving performance. In general,
any drug with a prominent central
nervous system (CNS) effect has the
potential to impair an individual’s
ability to operate a motor vehicle. The
level of impairment varies from patient
to patient, between different medica-
tions within the same therapeutic class,
and in combination with other medica-
tions or alcohol.
Many classes of medication have been
associated with increased crash risk or
impaired driving skills when assessed by
simulators or road tests. These include,
but are not limited to hypnotics, alcohol,
antiepileptic agents, anti-emetic agents,
narcotics, barbiturates, benzodiazepines,
antihistamines, antidepressants, antipsy-
chotics, and muscle relaxants. Some of
the highest crash rates have been noted
with long-acting benzodiazepines when
prescribed to older adults.
272
Other stud-
ies suggest that a signicant number of
272. Hemmelgarn, B., Suissa, S., Huang, A., et
al. (1997). Benzodiazepine use and the risk
of motor vehicle crash in the elderly. JAMA.
278:27–31.
Chapter 9—Medical Conditions and Medications That May Affect Driving
179
When prescribing new medications, the
physician should always consider the
patient’s existing regimen of prescription
and nonprescription medications.
Combinations of drugs may affect drug
metabolism and excretion, and produce
additive or synergistic interactions.
In fact, use of multiple psychoactive
medications is a common cause of
hospitalization for delirium among
older adults.
280
Because individuals
react differently to drug combinations,
280. Ray, W. A., Purushottam, B. T., Shorr, R. I.
(1939). Medications and the older driver.
Clin Geriatr Med. 9(2):413–438.
the degree of impairment caused by
polypharmacy may vary from patient
to patient. With polypharmacy’s strong
but unpredictable potential to produce
impairment, physicians should add
new medications at the lowest dosage
possible, counsel the patient to be alert
to any impairing side effects, and adjust
the dosages of individual medications
as needed to achieve therapeutic effects
with a minimum of impairment.
Section 13: Medications
As little as one serving of alcohol (1.25 oz. 80-proof liquor, 12 oz. beer, 5 oz. wine)
has the potential to impair driving performance in many individuals. Due to age-
related changes in body metabolism (e.g., increased body fat and decreases in lean
muscle mass), the same weight-adjusted amount of alcohol (hydrophilic) is likely
to result in higher blood levels of alcohol and functional impairment in advanced
age. In many cases, individuals may be impaired without being aware of it. Further-
more, alcohol can potentiate the CNS effects of medications to produce profound
and dangerous levels of impairment. Physicians should always warn their patients
against drinking and driving, and against combining alcohol and their CNS-
active medications.
For recommendations on substance abuse, see Section 5.
When a patient takes single or multiple medications with anticholinergic activity,
including some antidepressants, antihistamines, antiemetics, antipsychotics,
and antiparkinsonian drugs, the physician should be alert to the possibility of
anticholinergic toxicity and adjust medication dosages accordingly.
Anticholinergic effects that can impair driving performance include blurred vision,
sedation, confusion, ataxia, tremulousness, and myoclonic jerking. Patients should
be counselled about these symptoms and should alert their physicians immediately
if they occur. Patients should also be advised that psychomotor and cognitive
impairment might be present even in the absence of subjective symptoms
(this has been well documented for antihistamines).
Subtle decits in attention, memory, and reasoning may occur with therapeutic
dosages of anticholinergic drugs without signs of frank toxicity. These decits have
often been mistaken for symptoms of early dementia in elderly patients. Physicians
are advised to be aware of this possibility.
Alcohol
Anticholinergics
Chapter 9—Medical Conditions and Medications That May Affect Driving
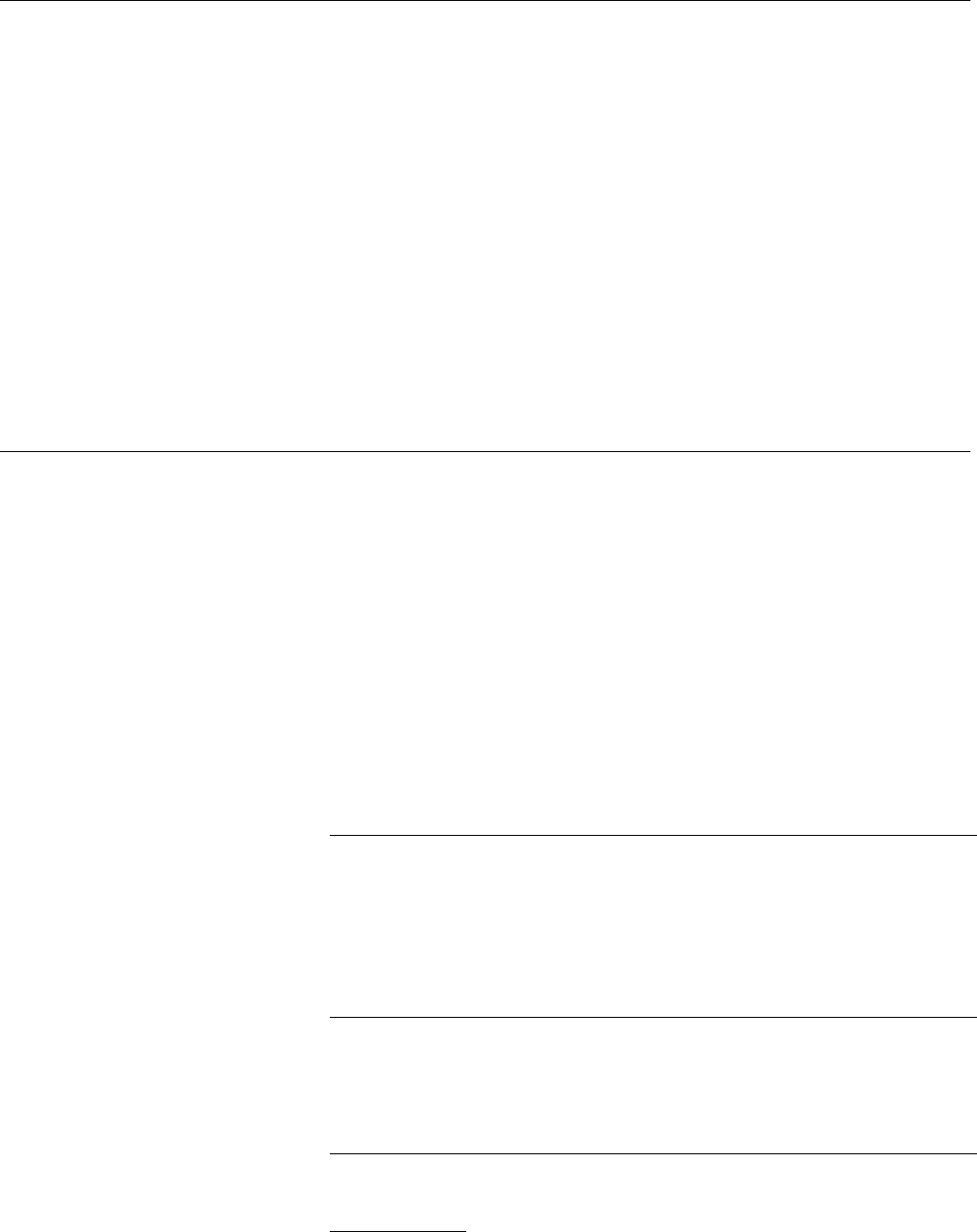
180
The patient should temporarily cease driving during the time of medication
initiation, withdrawal, or dosage change due to the risk of recurrent seizure and/or
potential medication side effects that may impair driving performance.
If there is signicant risk of recurrent seizure during medication withdrawal or
change, the patient should cease driving during this time and for at least three
months thereafter.
Note that many anticonvulsants (e.g., valproic acid, carbamazepine, gabapentine,
lamotrigine and topiramate) are also being used as mood stabilizers for treatment of
bipolar disorder, for agitation in dementia, and as sedating agents for anxiety. These
agents are typically an adjunct to antidepressants, antipsychotics and/or anxiolytics.
By themselves, anticonvulsants may be mildly impairing, but the combined medi-
cation effects on psychomotor performance tend to enhance their effects. When
prescribing anticonvulsants and other psychoactive drugs, it is wise to start with low
doses of each and gradually increase the dosage of each one separately to minimize
signicant side effects. In addition, this would allow for a clear identication of
which drug may be producing a benet or problem.
Impairing side effects vary among the different classes of antidepressants, and even
within certain classes of antidepressants. (In general, antidepressants that possess
antagonistic activity at cholinergic, alpha-1-adrenergic, and histaminergic receptors
are the most impairing.) Recent data have also implicated venlaxine as being asso-
ciated with motor vehicle crashes.
281
Whenever possible, physicians should initiate
antidepressant therapy with the least impairing medication possible. However, the
data indicating increased crash risk with the specic use of certain medications may
reveal associations but not necessarily causation. It is difcult to know whether
increased risk is associated with the drug, a drug-drug interaction, or the disease
itself (e.g., depression, which may independently impair attention, judgment, etc).
Patients should be advised not to drive during the initial phase of antidepressant
dosage adjustment(s) if they experience drowsiness, lightheadedness, or other side
effects that may impair driving performance. Patients should also be advised that
they might experience impairment in the absence of any subjective symptoms.
Side effects of bupropion (also known as Wellbutrin
®
and Zyban
®
) include anxiety,
restlessness, weight loss, and insomnia (leading to daytime drowsiness). Patients
should be counseled about these side effects and their potential to impair driving
performance. Because bupropion may cause seizures at high doses, it should not be
prescribed to patients with epilepsy, brain injuries, eating disorders, or other factors
predisposing to seizure activity.
Mirtazapine (also known as Remeron
®
) is typically taken only at night due to its
sedating effects. It has been shown to cause substantial impairment for many hours
after dosing. If daytime sedation is noted as an adverse side effect, another antide-
pressant should be considered or driving discontinued.
281. Walgreens Health Services. Continuing Pharmacy Education Web Site. Medication-Related Impaired
Driving: For Pharmacist. https://webapp.walgreens.com/cePharmacy/programsHTML/transportation-tech.pdf.
Accessed November 16, 2007.
Anticonvulsants
Antidepressants
Bupropion
Mirtazapine
Chapter 9—Medical Conditions and Medications That May Affect Driving
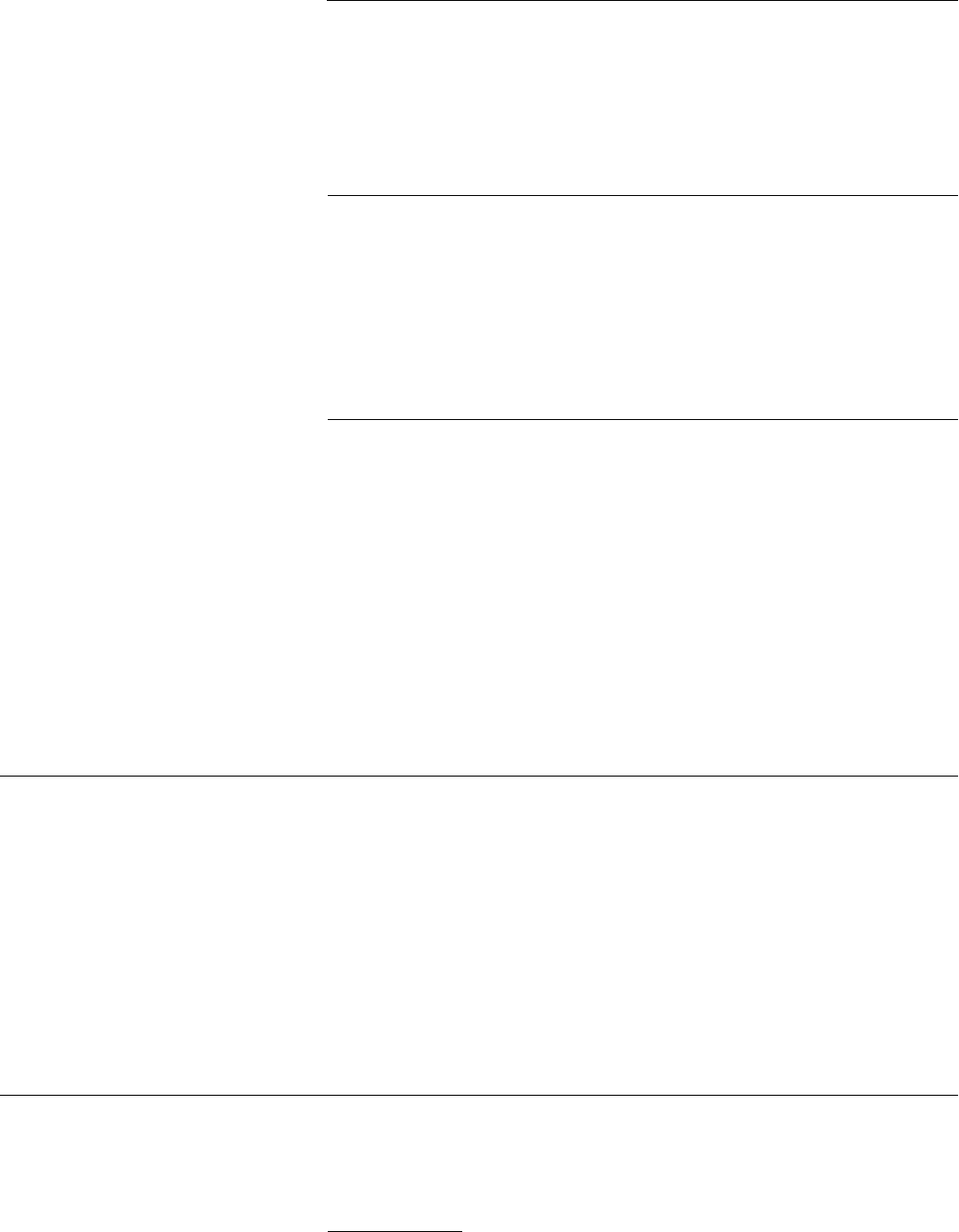
181
Side effects of MAO inhibitors that may impair driving performance include
blurred vision, overstimulation, insomnia (leading to daytime drowsiness),
orthostatic hypotension (with transient cognitive decits), and hypertensive
crisis (presenting with severe headaches and/or mental status changes). The latter
can be caused by failure to adhere to dietary and medication restrictions. Patients
should be counseled about these side effects and their potential to impair driving
performance.
Common side effects of SSRIs that may impair driving performance include sleep
changes (insomnia or sedation), headache, anxiety, and restlessness. While these
side effects tend to be mild and well tolerated, physicians should counsel patients
to be alert to their potential to affect driving performance. Special mention is made
of serotonin syndrome, wherein mental status changes, autonomic hyperactivity,
and neuromuscular side effects are observed due to excessive amounts of the drug or
a drug-drug interaction. Treatment includes discontinuing the offending agent or
hospitalization in severe cases.
Common side effects of TCAs that may impair driving performance include
sedation, blurred vision, orthostatic hypotension, tremor, excitement, and heart
palpitations. In studies involving healthy volunteers, the more sedating TCAs have
been shown to impair psychomotor function, motor coordination, and open-road
driving. Other studies appear to indicate an increased crash risk for drivers who
take TCAs.
282
Whenever possible, other agents like SSRIs or TCA’s with a low propensity for
anticholinergic effects (nortryptiline or desipramine) should be considered for
those who wish to continue driving. If nonimpairing alternatives are not available,
then the physician should advise patients of the potential side effects, and recom-
mend temporary driving cessation during the initial phase of medication initiation/
dosage adjustment. Patients should also be advised that they might experience
impairment even in the absence of subjective symptoms.
Numerous classes of drugs—including anticholinergics, antihistamines, antipsychotics,
cannabinoids, benzodiazepines, 5HT antagonists, and glucocorticoids—are used
for their antiemetic effect. Side effects of antiemetics that may impair driving
performance include sedation, blurred vision, headache, confusion, and dystonias.
Signicant impairment may be present even in the absence of subjective symptoms;
this has been well documented for many benzodiazepines and over-the-counter
antihistamines. Patients should be counseled about side effects and their potential
to impair driving performance, and should be advised that they may experience
impairment even in the absence of subjective symptoms.
For more detailed information, see also Anticholinergics, Antihistamines,
Antipsychotics, and Benzodiazepines in this section.
282. Ray, W. A., Purushottam, B. T., Shorr, R. I. (1993). Medications and the older driver.
Clin Geriatr Med. 9(2):413–438.
Monoamine oxidase (MAO) inhibitors
Selective serotonin reuptake inhibitors
(SSRIs)
Tricyclic antidepressants (TCAs)
Antiemetics
Chapter 9—Medical Conditions and Medications That May Affect Driving
182
In many patients, the rst generation antihistamines (such as diphenhydramine
and chlorpheniramine) have pronounced CNS effects. In studies involving healthy
volunteers, sedating antihistamines have been shown to impair psychomotor
performance, simulated driving, and open-road driving.
283
Furthermore, subjects
may experience impairment even in the absence of subjective symptoms of im-
pairment.
284
In contrast, most nonsedating antihistamines do not produce these
types of impairment after being taken in recommended doses.
285
Even nonsedating
antihistamines may cause impairments if taken in higher-than-recommended doses,
however, and one of them (i.e., cetirizine) may be slightly impairing to certain
patients in normal doses.
Patients who take sedating antihistamines should be advised not to drive while
on the medications. If these patients wish to continue driving, they should be
prescribed a nonsedating antihistamine.
With their hypotensive properties, common side effects of antihypertensives that
may impair driving performance include lightheadedness, dizziness, and fatigue. In
addition, antihypertensives with a prominent CNS effect, including beta-blockers
and the sympatholytic drugs clonidine, guanfacine and methyldopa, may cause
sedation, confusion, insomnia, and nervousness.
Patients should be counseled about these side effects and their potential to
impair driving performance. In addition, patients taking antihypertensives that
may potentially cause electrolyte imbalance (i.e., diuretics) should be counseled
about the symptoms of electrolyte imbalance and their potential to impair driving
performance.
Several medications and classes of medications, including levodopa, antimuscarinics
(anticholinergics), amantadine, and dopamine agonists, may be used in the treatment
of Parkinson’s disease symptoms. Common side effects of antiparkinsonian drugs that
may impair driving performance include excessive daytime sleepiness, lightheaded-
ness, dizziness, blurred vision, dyskinesias, on-off phenomenon, hallucinations, and
confusion. (See also Anticholinergics in this section for more information.)
Patients should be counseled about these side effects and advised not to drive if
they experience side effects. The physician may also consider referring patients for
formal psychomotor testing or for on-road assessment performed by a driver rehabi-
litation specialist.
Most—if not all—antipsychotic medications have a strong potential to impair
driving performance through various CNS effects. Some of the original or
“classic” antipsychotics are heavily sedating, and all produce extrapyramidal
side effects (EPS). Alhough the modern or “atypical” drugs have a lower
tendency to cause EPS, they, too, are sedating.
283. Ibid.
284. Weiler, JM., et al. (2000). Effects of fexofenadine, diphenhydramine, and alcohol on driving performance.
a randomized placebo-controlled trial in the Iowa Driving Simulator. Ann Intern Med. 132(5):354–363.
285. Ray, W. A., Purushottam, B. T., Shorr, R. I. (1993). Medications and the older friver. Clin Geriatr Med.
9(2):413–438.
Antihistamines
Antihypertensives
Antipsychotics
Antiparkinsonians
Chapter 9—Medical Conditions and Medications That May Affect Driving
183
Patients should be counseled about these side effects and advised not to drive if
they experience side effects severe enough to impair driving performance. The
physician should consider referring the patient for formal psychomotor testing or
for on-road assessment performed by a driver rehabilitation specialist. If medication
therapy is initiated while the patient is hospitalized, the impact of side effects on
driving performance should be discussed prior to discharge.
Studies have demonstrated impairments in vision, attention, motor coordination,
and driving performance with benzodiazepine use. Evening doses of long-acting
benzodiazepines have been shown to markedly impair psychomotor function the
following day, while comparable doses of short-acting compounds produce a lesser
impairment.
286
In contrast, benzodiazepine-like hypnotics (such as zolpidem and
zaleplon) have a more rapid rate of elimination. Studies of driving performance
and psychomotor function have shown that ve hours after taking zaleplon and
nine hours after taking zolpidem at recommended doses, it is generally safe to drive
again.41 Recently, reports in the news media and some studies indicate that zolpi-
dem has not uncommonly been found during serum toxicology testing of drivers
involved in fatal accidents or arrested for driving under the inuence of drugs.
287
Patients should be prescribed evening doses of the shortest-acting hypnotics when-
ever possible. Patients who take longer-acting compounds or daytime doses of any
hypnotic should be advised of the potential for impairment, even in the absence
of subjective symptoms. These patients should also be advised to avoid driving,
particularly during the initial phase of dosage adjustment(s).
Most skeletal muscle relaxants (e.g., carisoprodol and cyclobenzaprine) have
signicant CNS effects. Patients should be counseled about these side effects, and
should be advised not to drive during the initial phase of dosage adjustment(s) if
they experience side effects severe enough to affect safe driving performance.
Isolated case reports of confusion following the use of the NSAIDs phenylbutazone
and indomethacin suggest that they may rarely impair driving performance.
288
Recent data reveal an association with motor vehicle crashes, although this could
represent the effects of the disease and not specically treatment.
289
If the patient
reports this side effect, the physician should consider adjusting the dosage or
changing the medication.
286. Ibid.
287. Vermeeren, A., Danlou, P. E., O’Hanlon, J. F. (1999). Residual effects of aaleplon 10 and 20 mg on
memory and actual driving performance following administration 5 and 2 hours before awakening.
Br J Clin Pharmacol. 48:367–374.
Vermeeren, A., Muntjewerff, N. D., van Boxtel, M., et al. (2000). Residual effects of zaleplon and
zopiclone versus the effects of alcohol on actual car driving performance. Eur Neuropsychopharmacol.
10(suppl 3):S394.
Volkerts, E. R., Verster, J. C., Heuckelem, J. H. G., et al. (2000). The impact on car-driving performance
of zaleplon and zolpiden administration during the night. Eur Neuropsychopharmacol. 10(suppl 3):S395.
288. Jones, A. W., Holmgren, A., & Kugelberg, F. C. (2007). Concentrations of scheduled prescription drugs
in blood of impaired drivers: considerations for interpreting the results. Ther Drug Monitor. 29:248–260.
289. Ray, W. A., Gurwitz, J., Decker, M. D., & Kennedy D. L. (1992). Medications and the safety of the older
driver: is there a basis for concern? Hum Factors. 34(1):33–47.
Antipsychotics (continued)
Benzodiazepines and other sedatives /
anxiolytics
Muscle relaxants
Nonsteroidal anti-inammatory drugs
(NSAIDs)
Chapter 9—Medical Conditions and Medications That May Affect Driving
184
Patients should be counseled about the impairing effects of narcotic analgesics
(i.e., opioids) and the potential for impairment even in the absence of subjective
symptoms. They should also be advised not to drive while on these medications.
In addition, many narcotic analgesics have a high potential for abuse. However,
the literature also indicates that physicians often undertreat pain in the general
population and with older adults. Accordingly, physicians should always be alert
to signs of abuse. (For more information, see the recommendations for substance
abuse in Section 5.)
Common side effects of traditional stimulants (such as amphetamines and
methylphenidate) that may impair driving performance include euphoria,
overcondence, nervousness, irritability, anxiety, insomnia, headache, and rebound
effects as the stimulant wears off. Patients should be counseled about these side
effects and advised not to drive during the initial phase of dosage adjustment(s)
if they experience side effects severe enough to impair driving performance.
(The novel stimulant, modanil, is not euphorogenic, nor does it appear to
cause rebound effects. However, its safety for use when driving has not yet
been demonstrated.)
In addition, many stimulants have a high potential for abuse. Accordingly,
physicians should always be alert to signs of abuse. (For more information,
see the recommendations for substance abuse in Section 5.5.)
Narcotic analgesics
Stimulants
Chapter 9—Medical Conditions and Medications That May Affect Driving

CHAPTER 10
Moving Beyond This
Guide: Future Plans to
Meet the Transportation
Needs of Older Adults

187
safety by assessing the functions related
to driving (see the Assessment of Driv-
ing Related Skills [ADReS] in Chapter
3) and reviewing the presence and/or
severity of important medical illnesses
(Chapter 9). The AMA will continue
to promote awareness of the most
recent assessment and rehabilitation
tools, and we encourage physicians to
stay informed on these developments.
2. Increased availability and
affordability of driver rehabilitation
When the results of physician assess-
ment are unclear, or when further
correction of functional decits through
medical management is not possible,
driver rehabilitation specialists (DRSs)
are an excellent resource. DRSs can
perform a focused clinical assessment,
observe the patient in the actual driv-
ing task, and train him/her in the use
of adaptive techniques or devices to
compensate for functional decits. (See
Chapter 5 for more information.)
Unfortunately, access and cost remain
major barriers to the utilization of DRSs
by older drivers and their referring
physicians. DRSs are not available in
all communities, and there are presently
too few to provide services to all older
drivers who are in need of their services
Furthermore, driver assessment and
rehabilitation are expensive, and Medi-
care and private insurance companies
rarely pay for these services.
The previous chapters provide physi-
cians with recommendations and tools
for enhancing the driving safety of their
patients. As in other aspects of patient
care, however, further research can lead
to more effective care. We eagerly await
further evaluation of in-ofce tools
that can predict crash risk or determine
tness-to-drive, as well as improved ac-
cess to driver assessment and rehabilita-
tion. We also look forward to advanced
technology in vehicles to assist drivers
with navigation and safety issues. At
the same time, we wish for safer roads,
better transportation alternatives, in-
creased crashworthiness of vehicles, and
other vehicular improvements that can
help keep our patients safe on the road
as long as possible.
In this chapter, the AMA advocates for
coordinated efforts among the medi-
cal and transportation communities,
policymakers, community planners, the
automobile industry, and government
agencies to achieve the common goal of
safe transportation for the older popula-
tion. As this population continues to
expand and live longer, we all have
the challenge of keeping pace with its
transportation needs.
Listed below is the AMA’s checklist
of research, initiatives, applications,
and system changes that we believe are
crucial for improving and increasing the
safe mobility of the older population.
We encourage readers of this guide to
use this list as a launching pad to boost
your future plans and efforts.
CHAPTER 10
Moving Beyond This Guide:
Future Plans to Meet the
Transportation Needs of
Older Adults
1. Improved physician tools for the
assessment of driving safety
Physicians need an assessment tool that
reliably identies patients who are at
increased risk for a car crash. This test
battery must assess the primary functions
that are related to driving, and must
form a basis for medical interventions to
correct any functional decits that are
identied. In addition, this tool must be
brief, inexpensive, easy to administer,
and validated to predict crash risk and/or
the ability to pass a performance-based,
standardized, reliable and valid road test.
At present, no comprehensive tool is
available. Individual functional tests
(such as the Trail Making Test, Part B;
see Chapters 3 and 4) have been repeat-
edly shown to correlate with crash risk,
yet there is still not a universal cut-off
or score on these tests that can deter-
mine tness-to-drive. Researchers are
currently studying other tests in relation
to driving. The eld has focused on
heterogeneous groups of older adults
with modest correlations in functional
batteries.
290
Further steps will likely
require a focus on different batteries or
tests in a given specic older population
with a specic disease (e.g., glaucoma,
dementia).
While researchers work toward achieving
a comprehensive test battery, physicians
can best evaluate their patients’ driving
290. Ball, K. K., Roenker, D. L., Wadley, V. G., et al.
(2006). Can high-risk older drivers be identied
through performance-based measures in a
Department of Motor Vehicles setting?
J Am Geriatr Soc. 54:77–84.
188 Chapter 10—Moving Beyond This Guide: Future Plans to Meet the Transportation Needs of Older Adults
tor vehicle.
297,
298
We encourage State
licensing authorities and driver rehabili-
tation programs to investigate the use of
technologies to increase the availability
of reliable driver assessment services
to the public. Such technologies, if
integrated into or aligned with current
practices, could help form an intermedi-
ate step between physician assessment
and driver rehabilitation or increase the
licensing authority’s capacity to offer
specialized driver assessment to medi-
cally at-risk drivers.
4. The enhanced role of the driver
licensing agency in promoting the
safety of older drivers
As the agency that ultimately awards,
renews, restricts and revokes the driver’s
license, each State’s driver licensing
agency has the task of distinguishing
unsafe drivers from safe drivers. While
each State has its own procedures,
which are highly variable, potentially
unsafe drivers are usually identied by
one of four means: (1) failure of the
individual to meet licensing or license
renewal criteria; (2) report from the
individual or family; (3) report from
physicians, DRSs, law enforcement of-
cers, and others; and (4) judicial report.
To meet the standards for licensing,
the driver licensing agency initially
requires individuals to pass assessments
of knowledge, vision, and driving
skills. License renewal tends to be less
stringent, with many States permitting
renewal by mail. In recent years, certain
States have increased their efforts to
identify older drivers who are at risk
for unsafe driving by stipulating special
renewal procedures for this population.
These procedures include shortened re-
newal intervals, in-person renewal, and
mandatory reassessment of knowledge,
vision, and driving skills.
297. Walter, H., Vetter, SC., Grothe, J., et al. (2001).
The neural correlates of driving. Neuroreport.
12(8):1763–1767.
298. Ott, B. R., Heindel, W. C., Whelihan, W.
M., et al. (2000). A single-photon emission
computed tomography imaging study of driving
impairment in patients with Alzheimer’s disease.
Dement Geriatr Cogn Disord. 11(3):153–160.
and on-road performance in cognitively
impaired and healthy older drivers.
291
Certainly, limitations exist with the use
of simulators, such as lack of standard-
ization in the eld, use of different crash
scenarios, expense, need for techno-
logical support, and simulator-induced
sickness. However, unlike on-road
assessment, simulators can evaluate
performance in driving situations that
would otherwise be infeasible or danger-
ous.
292
293
In addition, there have been
recent attempts to study their validity
294
and reliability.
295
Yet, a recent study was
not able to correlate simulator ndings
with crash data in a cohort of sleep
apnea patients, who have one of the
highest crash rates associated with any
medical conditions.
296
Further research
and experience may conrm that driv-
ing simulators are safe, effective, and
readily acceptable to the public. It will
also be useful to discover if familiarity
with computers and games by successive
aging cohorts affects the outcome of
simulator performance and/or reduces
crashes.
We applaud recent efforts to further
understand the complex role the central
nervous system plays in operating a mo-
291. Freund, B., Gravenstein, S., Ferris, R. (2002).
Evaluating driving performance of cognitively
impaired and healthy older adults: a pilot study
comparing on-road testing and driving simula-
tion (letter to the editor). J Am Geriatr Soc.
50:1309.
292. Reimer, B., D’Ambrosio, L., Coughlin, J., et al.
(2006). Using self-reported data to assess the
validity of driving simulation data. Behav Res
Method. 38(2):314–324.
293. Uc, E. Y., Rizzo, M. , Anderson, S. W., et al.
(2006). Unsafe rear-end collision avoidance
in Alzheimer’s disease. J Neurol Sci. 251
(1–2):35–43.
294. Reimer, B., D’Ambrosio, L., Coughlin, J., et al.
(2006). Using self-reported data to assess the
validity of driving simulation data. Behav Res
Method. 38(2):314–24.
295. Contardi, S., Pizza, F., Sancisi, E., et al. (2004).
Reliability of a driving simulation task for
evaluation of sleepiness. Brain Res Bull.
63(5):427-431.
296. Turkington, P. M., Sircar, M. , Allgar, V., &
Elliott, M. W. (2001). Relationship between
obstructive sleep apnoea, driving simulator
performance, and risk of road trafc accidents.
Thorax. 56(10):800–805.
The American Occupational Therapy
Association (AOTA) is addressing
these issues through two initiatives.
First, AOTA is devising a framework to
increase the number of DRSs within the
occupational therapy (OT) profession.
This framework will include strategies
to promote older driver practice among
current OT practitioners, curriculum
content for continuing education
programs, and training modules for
entry-level OT educational programs.
Secondly, AOTA is actively lobbying
for consistent Medicare coverage of
OT-performed driver assessment and
rehabilitation, under the assertions that
these services fall under the scope of
OT practice and that driving is an in-
strumental activity of daily living. Indi-
vidual DRS programs have also pursued
insurance coverage from Medicare and
other providers, with varying degrees of
success.
In the effort to keep older drivers on
the road safely as long as is reasonable,
increased access to and affordability of
driver assessment and rehabilitation
are essential. We support the AOTA’s
initiatives, and suggest that physicians
use DRSs as a resource for their patients
whenever possible. We also encourage
research in this eld to create standard-
ized off-road and on-road tests that have
respectable levels of reliability, validity,
and test stability. Correlating results
on road tests with prospective at-fault
crash data remains an important area
of future study. Finally, the added value
of physicians referring their patients to
an OT driving program, in comparison
to “usual care,” would be an important
step in the process of obtaining Medi-
care and insurance company support for
funding these types of evaluations.
3. Increased investigation into the
use of simulators and comprehen-
sive assessment methods techniques
Validated driver assessment technolo-
gies may help make driver assessment
more widely available to older driv-
ers. Preliminary research with a com-
mercially available driving simulator
has demonstrated a strong correlation
between simulated driving performance
189
laws that provide immunity from breach
of condentiality lawsuits for physicians
and others who report impaired drivers
to their State licensing authority.
5. Enhanced role of the Medical
Advisory Board
A Medical Advisory Board (MAB) is
generally composed of State-licensed
physicians who work in conjunction
with the driver licensing agency to
determine whether mental or physical
conditions may impair an individual’s
ability to drive safely. MABs vary
among States in size, role, and level of
involvement. For example, the MAB of
the Maryland Motor Vehicle Adminis-
tration reviews the tness of individu-
als to drive safely, while California’s
MAB provides recommendations to
DMV staff for use in developing policies
that affect medically and functionally
impaired drivers.
304
Many States lack
an MAB altogether or have one that is
ineffective.
We encourage each State driver licens-
ing agency to enhance the role of its
MAB in order to provide a greater
capacity for assessment, rehabilita-
tion and support to older drivers. We
also encourage States that lack MABs
to create a multi-disciplinary team of
medical experts to develop and imple-
ment recommendations on the medical
tness of their State’s licensed drivers.
Such recommendations should be based
on the most current scientic data, and
should be implemented in an efcient
review process.
Recently, the National Highway and
Trafc Safety Administration and
the American Association of Motor
Vehicle Administrators (AAMVA)
completed a study of each State’s
304. Raleigh, R., & Janke, M. (2001). The role of
the medical advisory board in DMVs: protecting
the safety of older adult drivers. Maximizing
Human Potential: Newsletter of the Network
on Environments, Services and Technologies for
Maximizing Independence. American Society on
Aging 9(2):4–5.
tem for older drivers. For example, the
agency can work more closely with the
at-risk drivers’ physicians or the Medi-
cal Advisory Board to correct functional
decits through medical treatment, if
possible. Drivers with a high poten-
tial for rehabilitation can be referred
by the licensing agency to a DRS to
learn adaptive techniques and devices.
Licensing agencies can also consider
the patient’s driving needs by issuing
restricted licenses whenever possible to
help the driver maintain mobility while
protecting his/her safety. For those driv-
ers who must relinquish their license,
the agency can provide guidance in
seeking alternative transportation.
At-risk drivers can also be brought to
the attention of the driver licensing
agency by physician referral. How-
ever, many physicians are not aware of
their State’s referral procedures,
303
and
others fear legal liability for breach of
condentiality. With the advent of the
Health Insurance Portability and Ac-
countability Act (HIPAA), physicians
may have questions about the extent
and detail of patient information they
should provide in a referral. Driver
licensing agencies can encourage physi-
cian referral by establishing clear guide-
lines and simple procedures for referral
(e.g., comprehensive referral forms
that can be accessed over the Internet)
and promoting physician awareness of
these guidelines and referral procedures.
In many States, physicians who refer
patients to their State’s driver licensing
agency are not granted legal protec-
tion against liability for breaching the
patient’s condentiality. Indeed, several
States encourage or require physicians
to report impaired drivers without spe-
cically offering this legal protection.
Physicians should join advocacy groups
in their States to pass fair laws that pro-
tect physicians who report in good faith
and ensure anonymity for reporting.
State legislatures are encouraged to es-
tablish or maintain good-faith reporting
303. Cable, G., Reisner, M. , Gerges, S., & Thiru-
mavalavan, V. (2000). Knowledge, attitudes,
and practices of geriatricians regarding patients
with dementia who are potentially dangerous
automobile drivers: a national survey. J Am
Geriatr Soc. 48(1):14–17.
We encourage all States to maintain
or adopt renewal procedures for the
most effective identication of at-risk
older drivers. (See also Enhanced role
of the Medical Advisory Board below.)
We also encourage States to base their
standards for licensing on current sci-
entic data. For example, visual acuity
standards that are based on outdated
research may be unnecessarily restric-
tive to all drivers and to older drivers in
particular. As noted in Chapter 7, the
only recent licensing renewal procedure
that has been associated with decreased
crash risk is the requirement for in-
person renewal.
In addition to the vision screens that
are currently in use, driver licensing
agencies may also wish to utilize newer
tools (such as contrast sensitivity and
the useful eld-of-view test) that have
been shown to correlate with crash
risk.
299, 300
Some of these tools, along
with other tests of function and driving
skills, are currently being eld-tested
by the California Department of Motor
Vehicles as part of its three-tier assess-
ment system.
301
Future ndings from
this system may be useful to some driver
licensing agencies that are interested in
establishing similar tier systems.
Many individuals are understandably
reluctant to report themselves to the
driver licensing agency as unsafe driv-
ers. Although there are few data on
this issue, recent research on referrals
for tness-to-drive in Missouri suggests
that few if any drivers take this step.
302
Driver licensing agencies can do their
part by creating a more supportive sys-
299. Owsley C., Stalvey BT., Wells J., Sloane M.
E., McGwin G. Visual risk factors for crash
involvement in older drivers with cataract. Arch
Ophthalmol. 119:881–887.
300. Owsley C., Ball K., McGwin G., Sloane M. E.,
Roenker DL., White M. F., Overley ET. Visual
processing impairment and risk of motor vehicle
crash among older adults. JAMA.
279(14):1083–1088.
301. Personal correspondence with Mary Janke,
Ph.D., September 26, 2002; and
Janke M. K., & Eberhard J. W. Assessing
medically impaired older drivers in a licensing
agency setting. Accid Anal Prev. 30(3):347–361.
302. Personal communication, Dr. Tom Meuser,
Director of Aging, University Missouri St.
Louis.
Chapter 10—Moving Beyond This Guide: Future Plans to Meet the Transportation Needs of Older Adults

190
fruitful area that warrants additional
investigation.
307
9. Vehicle designs that optimize
the safety of older drivers and
their passengers
Age-related changes in vision, cogni-
tion, and motor ability may affect an
individual’s ability to enter/egress a
motor vehicle with ease, access critical
driver information, and handle a motor
vehicle safely. Older persons are also
less able to endure and recover from in-
juries sustained in an automobile crash.
We encourage vehicle manufacturers to
explore and implement enhancements
in vehicle design that address and com-
pensate for these physiological changes.
In particular, vehicle designs based on
the anthropometric parameters of older
persons—that is, their physical dimen-
sions, strength, and range of motion—
may be optimal for entry/egress; seating
safety and comfort; seat belt/restraint
systems; and placement and congura-
tion of displays, mirrors and controls.
Improvements in headlamp lighting to
enhance nighttime visibility and reduce
glare, as well as the use of high-contrast
legible fonts and symbols for in-vehicle
displays, may help compensate for age-
related changes in vision.
308
In addition,
prominent analog gauges may be easier
to see and interpret than small digital
devices.
309
Computers have revolution-
ized the motor vehicle industry by man-
aging airbag safety systems, anti-lock
brakes, and global positioning systems.
In-vehicle assessment tools to assess for
high-risk conditions may be developed
in the future.
In the event of a crash, increasingly
crashworthy vehicle designs and
307. Bedard, M. , Porter, M. M., Marshall, S., et
al. (2008). The combination of two training
approaches to improve older driver safety Traff
Inj Prev. 9:70–76.
308. Schieber, F. (1994). High-priority research and
development needs for maintaining the safety
and mobility of older drivers. Exp Aging Res.
20:35–43.
309. Koonce, JM., Gold, M. , & Moroze, M. (1986).
Comparison of novice and experienced pilots
using analog and digital ight displays. Aviat
Space Environ Med. 57(12 pt. 1):1181–1184.
As a result of the meeting, the FDA
and NTSB concluded that steps must
be taken to better educate the public
and prescribing physicians on the ef-
fects on driving of potentially sedating
drugs. Only limited steps have been
taken thus far, but we support efforts to
increase patient and physician educa-
tion and clarify labeling for consumers.
One recent educational effort informs
pharmacists about potentially driving-
impairing drugs, and offers an exten-
sive curriculum that reviews causes of
crashes and the mechanisms whereby
drugs may impair driving.
306
Physicians
are encouraged to review this excel-
lent resource, given the trend toward
polypharmacy and the myriad problems
associated with adverse drug events.
Currently, manufacturers of medications
do not routinely test their products for
effects on driving, nor are they required
to do so. We support the identica-
tion and routine use of effective testing
parameters to identify medications that
may interfere with the ability to safely
operate a motor vehicle. Similarly,
such parameters could be utilized in the
identication of medications that do
not impair drivers when typically used
as directed.
8. Promote self-awareness and
appropriate self-regulation.
Our society relies on self-regulation at
every level, including driving. Most
drivers with adequate cognitive func-
tion and some modest assistance with
compensatory behaviors and alterna-
tives will choose to preserve safety.
Some preliminary data from Califor-
nia indicate that drivers with greater
impairment were actually safer drivers,
perhaps because they had perceived the
need to make adjustments and had suc-
cessfully done so. More research must be
done on appropriate self-regulation, and
productive use must be made of results
as a part of a comprehensive solution.
A recent study suggests this may be a
306. Lococo, K., et al. Pharmacist Curriculum Drugs
and Driving . https://webapp.walgreens.com/
cePharmacy/programsHTML/transportation-tech.
pdf. Accessed November 12, 2007.
MAB practices.
305
This project detailed
the function of each State’s MAB,
its regulatory guidelines, and barriers
to the implementation of screening,
counseling, and referral activities. The
executive summary of this study had
many important recommendations for
States that license medically impaired
drivers, such as: each State should have
an active board to set standards and
guidelines and to be involved in tness-
to-drive evaluations; board members
should be adequately compensated;
immunity for physicians for reporting
should be granted; and national stan-
dards and forms, and referrals for mobil-
ity counseling and/or DRSs, should be
considered.
7. Increased public awareness of
medication side effects that may
impair driving performance
Many prescription and over-the-counter
medications have the potential to
impair driving performance. Despite
warnings on the label and counseling
by physicians and pharmacists, many
patients are unaware of these risks.
To address this problem, the National
Transportation Safety Board (NTSB)
has recommended (in its Safety Recom-
mendation I-00-5) that the U.S. Food
and Drug Administration (FDA) estab-
lish a clear, consistent, and easily recog-
nizable warning label for all prescription
and over-the-counter medications that
may interfere with the individual’s abili-
ty to operate a vehicle. This recommen-
dation was the focus of a FDA/NTSB
joint public meeting held in November
2001. This meeting hosted presenta-
tions of epidemiological and controlled
data on the effects of sedating drugs and
crash risk, as well as presentations from
innovators of devices that are designed
to test the degree to which drugs may
impair driving.
305. Lococo, KH., & Staplin, L. (2005). Strategies
for Medical Advisory Boards and Licensing
Review. DOT HS 809 874. Washington, DC:
National Highway Trafc Safety Administra-
tion. www.nhtsa.dot.gov/people/injury/research/
MedicalAdvisory/pages/Executive.html. Accessed
November 14, 2007.
Chapter 10—Moving Beyond This Guide: Future Plans to Meet the Transportation Needs of Older Adults

191
Existing forms of transportation clearly
need to be optimized for use by older
persons. In a telephone survey of 2,422
people 50 and older, ride-sharing was
the second most common mode of
transportation (after driving); however,
nearly a quarter of the survey partici-
pants cited feelings of dependency and
concerns about imposing as a barrier to
use. Public transportation was the usual
mode of transportation for fewer than
5 percent of survey participants, with
many citing unavailable destinations,
problems with accessibility, and fear of
crime as barriers to use. Fewer than 5
percent used taxis as their usual mode of
transportation due to their high cost.
317
Until these barriers are addressed, these
forms of transportation will remain
inaccessible to many older persons.
Transportation programs created speci-
cally for the older population, such as
senior shuttles and vans, exist in certain
communities. Certain States have
adopted the independent transportation
network (ITN) model developed by Dr.
Katherine Freund initially in Maine.
318
These programs address the Five A’s of
Senior-Friendly Transportation; namely,
availability, accessibility, acceptabil-
ity, affordability, and adaptability (see
Figure).
319
As the older population
continues to grow, we encourage the
creation of new programs or the expan-
sion of existing ones to keep pace with
passengers’ needs. We also encourage
stronger community outreach to in-
crease awareness of such programs.
317. Ritter, AS., Straight, A., & Evans, E. (2002).
Understanding Senior Transportation: Report
and Analysis of a Survey of Consumers Age
50+. American Association for Retired Persons;
Policy and Strategy Group, Public Policy
Institute.
318. ITN America. (2007). www.itnamerica.org.
Accessed November 12, 2007.
319. Supplemental Transportation Programs for Se-
niors. (2001, June). By the Beverly Foundation,
prepared for AAA Foundation for Trafc Safety.
One of the top requests of the nearly
200 Iowans (older drivers, transporta-
tion professionals, and senior-related
professionals) attending the Iowa
Older Drivers Forum was the enhanced
enforcement of speed and aggressive
driving laws.
313
In terms of road and
trafc engineering, the Federal High-
way Administration (FHWA) has
recognized and addressed the needs of
older road users in its Highway De-
sign Handbook for Older Drivers and
Pedestrians, a supplement to existing
standards and guidelines in the areas
of highway geometry, operations, and
trafc control devices.
314
These design
features may be implemented in new
construction, renovation and mainte-
nance of existing structures, and “spot”
treatment at certain locations where
safety problems exist or are anticipat-
ed.
315
Recent positive news is a trend or
reduction in highway deaths for the rst
time since 1992, which in part has been
attributed to installation of median
guard cable on busy highways, building
better roads, and the addition of rumble
strips to the shoulders of roads.
316
The
FHWA handbook will soon be updated
to incorporate the latest research on the
effectiveness of design and engineering
enhancement to accommodate older
road users.
11. Better alternatives to driving
For the older population, alternatives to
driving are often less than ideal or non-
existent. When faced with the choice
of driving unsafely or losing mobility,
many risk their safety by continuing
to drive.
313. Iowa Safety Management System: Safe Mobility
Decisions for Older Drivers Forum. June 19-20,
2002.
314. Staplin, L., Lococo, K., Byington, S., Harkey, D.
(2001, October). Highway Design Handbook
for Older Drivers and Pedestrians. FHWA-
RD-01-103. Washington, DC: Federal Highway
Administration.
315. Ageing and Transport: Mobility Needs and
Safety Issues. (2001). Organisation for Eco-
nomic Co-Operation and Development; p. 60.
316. Tom Warne Report. (2007). Missouri Highway
Deaths Decline. http://tomwarnereport.com/twr/
twr_v4n28.html. Accessed November 15, 2007.
restraint systems designed for fragile
occupants may enhance the safety of
older drivers and passengers. Further-
more, certain add-on features may make
current vehicle designs safer and more
accessible for older drivers. For example,
handholds and supports on door frames
may facilitate entry/egress for drivers
and their passengers. Padded steering
wheels and seat adjuster handles (rather
than knobs) may benet drivers with
decreased hand grip, while adjustable
steering wheels and foot pedals may aid
drivers with limited range of motion.
310
Other adjustable controls and displays
may allow older drivers to tailor their
vehicle to their changing abilities and
needs. New safety features with the
potential to prevent injury in older
adults include: tire pressure monitor-
ing systems, adaptive cruise control/
collision mitigation systems, blind
spot detection/collision warning, lane
departure warnings, rollover prevention,
occupant-sensitive airbags, emergency
brake assist, rearview cameras, and
on-demand emergency response systems
(e.g., OnStar).
311
10. Optimal environments for older
drivers and pedestrians
Many older road users are at a disad-
vantage on roads and highways that are
most heavily used by and traditionally
designed for a younger population. In
a telephone survey of 2,422 people 50
and older, nearly one of ve participants
considered inconsiderate drivers to be
a signicant problem. Other commonly
identied problems included trafc con-
gestion, crime, and fast trafc.
312
These problems may be ameliorated
through trafc law enforcement and
better road and trafc control designs.
310. Ageing and Transport: Mobility Needs
and Safety Issues. (2001). Organisation for
Economic Co-Operation and Development;
p. 69–71.
311. Edmunds.Com. Top 10 High-Tech Car Safety
Technologies; 2007. www.edmunds.com/reviews/
list/top10/114984/article.html. Accessed Novem-
ber 15, 2007.
312. Ritter, AS., Straight, A., & Evans, E. (2002).
Understanding Senior Transportation: Report
and Analysis of a Survey of Consumers Age
50+. American Association for Retired Persons.
Chapter 10—Moving Beyond This Guide: Future Plans to Meet the Transportation Needs of Older Adults

192
and programs for the safe mobility of
the aging population.
Supplemental Transportation Programs
for Seniors. By the Beverly Founda-
tion, prepared for AAA Foundation for
Trafc Safety, June 2001. This report
contains the ndings of the Supplemen-
tal Transportation Program for Seniors
project, which was initiated in 2000 by
the AAA Foundation for Trafc Safety,
a philanthropic foundation in Wash-
ington, DC, and the Beverly Founda-
tion, a private foundation in Pasadena,
California. This project was designed as
a nine-month effort to gather informa-
tion about community-based transporta-
tion programs for seniors in the United
States. In describing and evaluating
these programs in order to provide their
ndings to interested organizations, the
project staff recognized the importance
of ve criteria for senior-friendly trans-
portation, which are listed.
Lococo , K., Tyree, R. Medication-Re-
lated Impaired Driving. By NHTSA and
co-sponsored by Walgreens, 2007.
By NHTSA and co-sponsored by
Walgreens, this excellent review of
potential driving-impairing drugs
provides credits or CEUs for pharmacy
technicians. However, this curriculum
is useful reading for any clinician who
prescribes drugs to older adults. The
manual covers causes of motor vehicle
crashes, reviews functional abilities that
are key for operating a motor vehicle,
and lists reasons why medications may
impair driving. There is a discussion
of the term “potentially impairing
medications” and an updated review of
the literature that identies high risk
drugs. Ethical and legal issues in drug
prescribing are addressed. Although the
curriculum was created for pharmacists,
much of the information is helpful to
physicians.
Lococo, K., Staplin, L. Strategies for
Medical Advisory Boards and Licensing
Review. DOT HS 809 874 , July 2005.
This NHTSA-funded project, written
by Lococo and Staplin, reviews the cur-
rent operations and practices of MABs.
A summary of what each State is cur-
rently doing in this area is provided.
Figure 10.1
The Five A’s of Senior-Friendly
Transportation
(Reproduced from Supplemental
Transportation Programs for Seniors,
The Beverly Foundation)
Availability: Transportation exists and
is available when needed (e.g., eve-
nings, weekdays, weekends)
Accessibility: Transportation can be
reached and used (e.g., bus stairs are
negotiable, seats are high enough,
vehicle comes to the door, transit
stops are reachable)
Acceptability: Deals with standards
including cleanliness and safety
(e.g., the transporting vehicle is
clean, transit stops are in safe areas,
drivers are courteous and helpful)
Affordability: Deals with costs
(e.g., fees are affordable, vouchers
or coupons are available to defray
out-of-pocket expenses)
Adaptability: Transportation can be
modified or adjusted to meet special
needs (e.g., the vehicle can accom-
modate a wheelchair, trip chaining is
possible, escorts can be provided)
12. Education and training tools
Additional resources
The following resources contain ad-
ditional information on meeting the
mobility needs of the older population:
Ritter, A. S., Straight, A., and Evans,
E. Understanding Senior Transporta-
tion: Report and Analysis of a Survey of
Consumers Age 50+. AARP, Policy and
Strategy Group, Public Policy Institute,
2002. This paper was created to explore
the problems of people 50 and older, in
particular, those 75and older with rela-
tion to transportation. May be used in
the development of policies that expand
and improve transportation options for
older persons.
Staplin, L., Lococo, K., Byington, S.,
and Harkey, D. Highway Design Hand-
book for Older Drivers and Pedestrians.
FHWA-RD-01-103, October 2001. This
applications-oriented handbook pro-
vides detailed design recommendations
for ve types of sites: (1) intersections
(at grade); (2) interchanges (grade sepa-
ration); (3) roadway curvature and pass-
ing zones; (4) construction/work zones;
and (5) highway-rail grade crossings.
This handbook is primarily intended
for highway designers, trafc engineers,
and highway safety specialists involved
in the design and operation of highway
facilities. It may also be of interest to re-
searchers concerned with issues of older
road user safety and mobility.
Ageing and Transport: Mobility Needs
and Safety Issues. Organisation for
Economic Co-Operation and Develop-
ment (OECD), 2001. The OECD, an
international organization dedicated to
addressing the economic, social, and
governance challenges of a globalized
economy, produced this investigation
of the travel patterns, transport and
safety needs, and mobility implications
of tomorrow’s elderly. It is intended to
inform strategists, policy-makers, regula-
tors, and the general public of the aging
population’s safety and mobility needs;
dispel myths and misconceptions about
older road users; and present the latest
research ndings to assist decision-
makers in formulating sound policies
Chapter 10—Moving Beyond This Guide: Future Plans to Meet the Transportation Needs of Older Adults
193
An executive summary is especially
useful in outlining the direction States
and MABs should pursue in order to
enhance their usefulness and viability,
and have an impact on public safety.
Maintaining Safe Mobility in an Aging
Society. The overarching objective
of this book is to provide a concise,
comprehensive, and up-to-date resource
on aging and transportation. Speci-
cally, it has the following goals: Enable
readers to understand the issues related
to aging and mobility and to respond
to the often heard comment “Just take
their driver license away”; describe the
skills related to safe driving and how
they can be affected by aging; critically
examine the current evidence on how
medical conditions and medications
affect driving skills; provide a compre-
hensive description of screening and
assessment practices, issues, and tools;
provide information to help older adults
transition from full driving to driving
cessation; and explore various means by
which an aging individual can maintain
safe mobility. (Eby, D.W., Molnar, L.J.,
& Kartje, P.S.. Maintaining Safe Mobil-
ity in an Aging Society. New York, NY:
CRC Press. ISBN: 9781420064537.
In press.)
Chapter 10—Moving Beyond This Guide: Future Plans to Meet the Transportation Needs of Older Adults
194

APPENDIX A
CPT
®
Codes
197Appendix A—CPT
®
Codes
The following Current Procedural Terminology (CPT
®
) codes
can be used for driver assessment and counseling, when
applicable. These codes were taken from Current Procedural
Terminology (CPT
®
). 4th ed., Professional ed. Chicago, IL:
American Medical Association; 2009.
When selecting the appropriate CPT
®
codes for driver
assessment and counseling, rst determine the primary reason
for your patient’s ofce visit, as you would normally. The
services described in this Guide will most often fall under
Evaluation and Management (E/M) services. Next, select
the appropriate E/M category/subcategory. If you choose to
apply codes from the Preventive Medicine Services category,
consult Table 1 for the appropriate codes. If any additional
services are provided over and above the E/M services, codes
from Table 2 may be additionally reported.
APPENDIX A
CPT
®
codes
New Patient, Initial Comprehensive Preventive Medicine
Evaluation and management of an individual including an age and gender
appropriate history, examination, counseling/anticipatory guidance/risk factor
reduction interventions, and the ordering of appropriate immunizations(s),
laboratory/diagnostic procedures.
These codes can be used for a complete Preventive Medicine history and physical exam for
a new patient (or one who has not been seen in three or more years), which may include
assessment and counseling on driver safety. If signicant driver assessment and counseling
take place during the ofce visit, Modier-25 may be added to the codes above.
Established Patient, Periodic Comprehensive Preventive Medicine
Reevaluation and management of an individual including an age and gender
appropriate history, examination, counseling/anticipatory guidance/risk factor
reduction interventions, and the ordering of appropriate immunization(s),
laboratory/diagnostic procedures.
Codes from the Preventative Medicine Services 99386-99387 and 99396-99397 can only be
reported once per year. If driver assessment and counseling take place during the ofce visit,
Modier-25 may be added to the codes above.
99386 40-64 years
99387 65 years and older
99396 40-64 years
99397 65 years and older
99401 Approximately 15 minutes
99402 Approximately 30 minutes
99403 Approximately 45 minutes
99404 Approximately 60 minutes
Modier-25 is appended to the ofce/outpatient service code to indicate that a signicant, separately identiable E/M service
was provided by the same physician on the same day as the preventive medicine service.
Counseling and/or Risk Factor Reduction Intervention
Preventive medicine counseling and risk factor reduction interventions provided
as a separate encounter will vary with age and should address such issues as family
problems, diet and exercise, substance abuse, sexual practices, injury prevention,
dental health, and diagnostic and laboratory test results available at the time of
the encounter. (These codes are not to be used to report counseling and risk factor
reduction interventions provided to patients with symptoms or established illness.)
These are time-based codes, to be reported based upon the amount of time spent counseling
the patient. Driver safety or driving retirement counseling fall under the category of injury
prevention. Please note that for driving retirement counseling, a copy of the follow-up letter
to your patient can be included in the patient’s chart as additional documentation. A sample
letter can be found in Chapter 6.
Table 1: Evaluation and Management—Preventive Medicine Services
If the primary reason for your patient’s visit falls under the E/M category of Preventive Medicine Services,
choose one of the following codes:
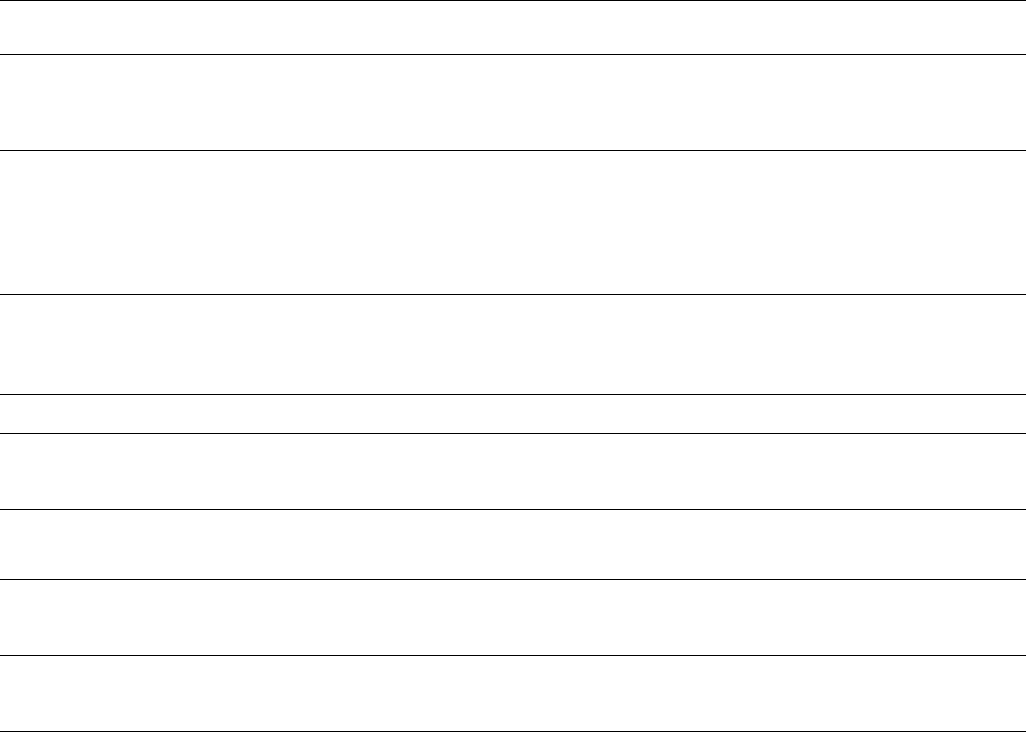
198 Appendix A—CPT
®
Codes
Table 2: Additional codes
The codes below can be used for administration of ADReS (see Chapter 3). If you complete the entire assessment, you can
include codes 99420, 95831 and either 99172 or 99173. The ADReS Score Sheet can serve as the report.
Administration and Interpretation of Health Risk Assessment Instrument
Muscle and Range of Motion Testing
Muscle testing, manual (separate procedure)with report; extremity
(excluding hand)or trunk.
Visual Function Screening
Automated or semi-automated bilateral quantitative determination of visual
acuity, ocular alignment, color vision by pseudoisochromatic plates, and eld of
vision (may include all or some screening of the determination(s) for contrast
sensitivity, vision under glare).
Screening Test of Visual Acuity, quantitative, bilateral
The screening used must employ graduated visual acuity stimuli that allow a
quantitative estimate of visual acuity (e.g., Snellen chart).
99420
95831
99172
99173
99406
99407
99408
99409
New CPT
®
codes for the Revised Physician’s Guide:
Smoking and tobacco use cessation counseling visit; intermediate, greater than
3 minutes up to 10 minutes
Smoking and tobacco use cessation counseling visit; intensive, greater than
10 minutes
Alcohol and/or substance (other than tobacco) abuse structured screening
(eg, AUDIT, DAST), and brief intervention (SBI) services; 15 to 30 minutes
Alcohol and/or substance (other than tobacco) abuse structured screening
(eg, AUDIT, DAST), and brief intervention (SBI) services;greater than30 minutes

APPENDIX B
Patient and Caregiver
Educational Materials

201Appendix B—Patient and Caregiver Educational Materials
APPENDIX B
Patient and Caregiver
Educational Materials
These handouts were designed to be user-friendly and simple to read. All patient education materials were written at or below
a 6th grade reading level, and all family and caregiver material was written at a 7th grade reading level.
We encourage physicians to make copies of these handouts for their patients, have them available in the ofce setting, educate
ofce staff to distribute them when appropriate, and use them as talking points when discussing driving issues with patients.
203Appendix B—Patient and Caregiver Educational Materials
Am I a Safe Driver?
Check the box if the statement applies to you.
I get lost while driving.
My friends or family members say they are worried about my driving.
Other cars seem to appear from nowhere.
I have trouble nding and reading signs in time to respond to them.
Other drivers drive too fast.
Other drivers often honk at me.
Driving stresses me out.
After driving, I feel tired.
I feel sleepy when I drive.
I have had more “near-misses” lately.
Busy intersections bother me.
Left-hand turns make me nervous.
The glare from oncoming headlights bothers me.
My medication makes me dizzy or drowsy.
I have trouble turning the steering wheel.
I have trouble pushing down the foot pedal.
I have trouble looking over my shoulder when I back up.
I have been stopped by the police for my driving.
People no longer will accept rides from me.
I have difculty backing up.
I have had accidents that were my fault in the past year.
I am too cautious when driving.
I sometimes forget to use my mirrors or signals.
I sometimes forget to check for oncoming trafc.
I have more trouble parking lately.
If you have checked any
of the boxes, your safety
may be at risk when you
drive.
Talk to your doctor about
ways to improve your
safety when you drive.
205Appendix B—Patient and Caregiver Educational Materials
Successful Aging Tips
Tip #1: Take care of your health.
Visit your doctor regularly.
Ask about tests and immunizations that are right
for your age group.
Consider testing for cancer that is right for your
age group.
Treat any risk factors for atherosclerosis or
“hardening of the arteries.”
Eat a healthy diet. Your diet should be low in fat
and high in ber.
• Eat plenty of vegetables, fruits, beans and whole
grains.
• Eat low fat proteins in the form of lean red meat,
poultry and sh.
• Get enough calcium by drinking low fat milk
and eating low fat yogurt and cheese.
• Eat a variety of foods to get enough vitamins
and minerals in your diet.
• Drink lots of water.
Exercise to stay t. Be active every day at your
own level of comfort.
• Walk, dance, or swim to improve your
endurance.
• Work out with weights to increase your strength.
• Stretch to maintain your exibility or consider
joining group classes that will help you stay t
(e.g., yoga, tai chi).
Don’t drink too much alcohol. It is recommended
that people over the age of 65, not have more than
one drink per day. (A drink is one glass of wine,
one bottle of beer, or one shot of hard liquor.)
Never drink alcohol with your medicines!
Don’t use tobacco in any form. This means
cigarettes, cigars, pipes, chew or snuff. If you
need help quitting, talk to your doctor.
Tip #2: Keep yourself safe.
Make your home a safe place.
• Keep your home, walkways and stairways well
lit and uncluttered.
• Keep working smoke detectors and a re
extinguisher in your home.
• Adjust the thermostat on your hot water tank
so that you don’t burn yourself.
• Remove rearms from the house.
Prevent falls.
• Make sure all throw rugs have non-slip backs
so they don’t throw you!
• Slip-proof your bathtub with a rubber mat.
• Consider grab bars and a shower chair for
the bathtub.
• Consider a raised toilet seat.
• Consider an occupational therapy home
safety evaluation.
Stay safe in the car.
• Wear your seat belt—and wear it correctly!
(It should go over your shoulder and across
your lap.)
• Never drink and drive!
• Don’t drive when you are angry, upset,
sleepy or ill.
• If you have concerns about your driving safety,
talk to your doctor.
• Do not use a cell phone while driving.
• Do not do other activities such as eating,
reading, and shaving when driving.
(over)
206 Appendix B—Patient and Caregiver Educational Materials
Tip #3: Take care of your
emotional health.
Keep in touch with family and friends.
It’s important to maintain your social life!
Exercise your mind. Keep your mind active
by reading books, doing crossword puzzles,
and learning about computers.
Stay active by joining groups and keeping your
mind alert.
• Consider doing crosswords, puzzles, computer
games, card games, etc.
• Join a club, organization, or religious group and
participate in volunteer activities.
• Consider volunteering to drive an older adult
who no longer has a license!
Keep a positive attitude!
Remember to smile and laugh.
• Focus on the good things in your life, and don’t
dwell on the bad.
• Stay active with the activities that make you
happy.
• If you’ve been feeling sad lately or no longer
enjoy the things you used to, ask your doctor
for assistance.
Tip #4: Plan for your future.
Keep track of your money. Even if someone else
is helping you manage your bank accounts and
investments, stay informed.
Know your own health. This is important for
receiving good medical care.
• Know what medical conditions you have.
• Know the names of your medicines and how
often you take them.
• If you are having trouble remembering taking
your medication, use a pillbox, calendar, or
family member to help you stay on track.
• Make a list of your medical conditions, medi-
cines, drug allergies (if any), and the names
of your doctors. Keep this list in your wallet.
Make your health care wishes known to your
family and doctors.
• Consider lling out an advance directives form.
This form lets you state your health care choices
or name someone to make these choices for you
in case you are unable to do so.
• Give your family and doctors a copy of the
advanced directives form. This way, they have
a written record of your choices in case you are
unable to tell them at the time.
• If you need help with your advance directives,
talk to your doctor or your lawyer.
Create a transportation plan. If you don’t drive,
know how to get around.
• Ask family and friends if they would be willing
to give you a ride.
• Find out about buses, trains, and shuttles in your
area.
• If you need help nding a ride, contact your
local Area Agency on Aging.
207Appendix B—Patient and Caregiver Educational Materials
Tips for Safe Driving
Tip #1: Drive with care.
Always—
• Plan your trips ahead of time. Decide what time
to leave and which roads to take. Try to avoid
heavy trafc, poor weather and high-speed
areas.
• Wear your seat belt—and wear it correctly.
(It should go over your shoulder and across
your lap.)
• Be sure you “t” well in your car. Take advantage
of a CarFit class (see resources) if one is available
in your community.
• Drive at the speed limit. It’s unsafe to drive too
fast or too slow.
• Be alert—pay attention to trafc at all times.
• Keep enough distance between you and the car
in front of you.
• Be extra careful at intersections. Use your turn
signals and remember to look around you for
people and other cars.
• Check your blind spot when changing lanes or
backing up.
• Be extremely careful with left hand turns,
allowing enough time to pass through the
intersection in case of on-coming trafc.
• Be extra careful at train tracks. Remember to
look both ways for trains.
• When you take a new medicine, ask your
doctor or pharmacist about side effects.
Many medicines may affect your driving even
when you feel ne. If your medicine makes you
dizzy or drowsy, talk to your doctor to nd out
ways to take your medicine so it doesn’t affect
your driving.
Never—
• Never drink and drive.
• Never drive when you feel angry or tired. If you
start to feel tired, stop your car somewhere safe.
Take a break until you feel more alert.
• Never drive if your medication is making you
sleepy.
• Never use a cell phone when driving.
• Never eat, drink or do other activities while
driving.
• Never drive in icy or snowy weather.
If—
• If you don’t see well in the dark, try not to drive
at night or during storms.
• If you have trouble making left turns at an
intersection, make three right turns instead
of one left turn.
• If you can, avoid driving in bad weather such
as rain, sleet or snow.
• If a certain route always causes you stress,
try to nd an alternate route.
• If someone in the car is bothering you
(e.g., noisy grandchildren) tell him or her to stop.
(over)
208 Appendix B—Patient and Caregiver Educational Materials
Tip #2: Take care of your car.
• Make sure you have enough gas in your car.
• Make sure your tires have the right amount of
air and check them each month for any wear
or damage.
• Get your car tuned up regularly.
• Keep your windshields and mirrors clean.
• Keep a cloth in your car for cleaning windows.
• Replace your windshield wiper blades when they
get worn out.
• Consider using Rain-X or a similar product to
keep your windows clear.
• If you are shopping for a new car, look for a car
with power steering and automatic transmission.
• If you own a computer you can check to see
how well a car will do if it is involved in a crash.
This information is on the following Web site
of the National Highway Trafc Safety Admin-
istration: www.safercar.gov. You might want to
consider buying a car that has the highest rating
when struck by another vehicle from the front
or side.
Tip # 3: Know where you can find a ride.
How do you get around when your car is in
the shop? If you don’t know the answer to this
question, it’s time for you to put together a
“transportation plan.”
A transportation plan is a list of all the ways that
you can get around. Use this list when your car is
in the shop or when you don’t feel safe driving.
Your transportation plan might include:
• Rides from friends and family
• Taxi
• Bus or train
• Senior shuttle
• Volunteer drivers from your local community
or government center.
If you need help creating a transportation plan,
your doctor can get you started.
Tip #4: Take a driver safety class.
To learn how to drive more safely, try taking a
class. In a driver safety class, the instructor teaches
you skills that you can use when you are driving.
To nd a class near you, call one of the following
programs:
AAA Foundation for Trafc Safety
Safe Driving for Mature Operators (course)
www.seniordrivers.org/driving/driving.cfm?button=
publication&selection=MO
AARP Driving Safety Program
The classic course with information on how to
locate an educational venue in your community.
www.aarp.org/families/driver_safety/
wrapper_driver.py
Driving School Association of the
Americas, Inc.
1-800-270-3722
These classes usually last several hours. These
classes do not cost much money—some are even
free. As an added bonus, you might receive a
discount on your car insurance after taking one
of these classes. Talk to your insurance agent and
company to determine if they offer a discount.
209Appendix B—Patient and Caregiver Educational Materials
How to Assist the
Older Driver
As experienced drivers age, changes in vision,
reaction time, and /or medical conditions may
cause them to drive less safely. Sometimes these
changes happen so slowly that drivers may not
even be aware that their skills have declined.
If you have concerns about someone’s driving
safety, here’s what you can do to keep your older
driver safe AND mobile.
Is your loved one a safe driver?
If you have the chance, go for a ride with this
driver. Look for the following warning signs in
his/her driving:
• Forgets to buckle up (use seat belts)
• Does not obey stop signs or red trafc lights
• Fails to yield right of way
• Drives too slowly or quickly
• Often gets lost, even on familiar routes
• Stops at a green light or at the wrong time
• Doesn’t seem to notice other cars, walkers,
or bike riders on the road
• Doesn’t stay in the lane
• Gets honked at or passed often
• Reacts slowly to driving situations
• Makes poor driving decisions
• Fails to use mirrors, check for blind spots, use
turn signals
• Mixes up gas and brake pedal or no longer can
use them smoothly
• Too cautious or too aggressive when driving
Other signs of unsafe driving:
• Recent near misses or fender benders
• Recent tickets for moving violations
• Repeated comments from those riding with your
driver or watching them in trafc about close
calls, near misses, or the driver not seeing other
vehicles.
• Accidents, especially those that were the driver’s
fault.
• Recent increase in the car insurance premium
Riding with or following your driver, every once in
a while, is one way to keep track of your loved one’s
driving. Another way is by talking to the spouse or
friends of the driver you are concerned about.
If you are concerned about your loved
one’s driving, what can you do?
Talk to your loved one. Say that you are concerned
about his/her driving safety. Ask if he or she shares
your concern.
• Don’t bring up your concerns while driving.
It’s dangerous to distract the driver! Wait until
he or she is calm and you have the driver’s full
attention.
• Explain why you are concerned. Give specic
reasons—for example, a medical condition like
poor vision, recent fender benders, getting lost,
or running stop signs.
• Realize that your loved one may become
negative or defensive. After all, driving is
important for independence and self-esteem.
(over)

210 Appendix B—Patient and Caregiver Educational Materials
• If the person you are concerned about does not
want to talk about driving at that time, bring
it up again later. Your continued concern and
support may help your loved one feel more
comfortable with this topic.
• Be a good listener. Take your loved one’s
concerns seriously.
• Consider using a handout like the Hartford’s
“We Need to Talk” which can be accessed at the
following website; www.thehartford.com/
talkwitholderdrivers/brochure/brochure.htm or
writing the Hartford and requesting brochures at;
The Hartford
We Need to Talk
200 Executive Boulevard
Southington, CT 06489
Help make plans for transportation. When your
loved one is ready to talk about his/her driving
safety, you can work together to create plans for
future safety.
• Make a formal agreement about driving. In this
agreement, your loved one chooses a person to
tell him/her when it is no longer safe to drive.
This individual then agrees to help your loved
one make the transition to driving retirement.
(You can nd a sample agreement in At the
Crossroads: A Guide to Alzheimer’s Disease, De-
mentia & Driving. Order a free copy by writing
to At the Crossroads booklet, The Hartford, 200
Executive Boulevard, Southington, CT, 06489.)
• Help create a transportation plan. Your loved
one may rely less on driving if he/she has other
ways to get around. Starting to use other ways to
travel even before the person stops driving may
make the change easier in the future.
Encourage a visit to the doctor. The doctor can
examine a person’s medical history, medication
regimen, and current health to see if any of these
may be affecting his/her driving safety. If so, the
doctor can provide treatment to help improve
medical conditions and possibly driving safety.
Encourage your loved one to take a driving test.
A driver rehabilitation specialist (DRS) can assess
a person’s driving safety through an ofce exam
and driving test. The DRS can also teach special
techniques or provide special equipment to help
a person drive more safely. (To nd a DRS in your
area, ask your doctor for a referral or contact the
Association for Driver Rehabilitation Specialists
(ADED
*
):
The Association for Driver Rehabilitation
Specialists (ADED
*
)
Information on the Association.
www.aded.net/i4a/pages/index.cfm?pageid=1
Also provides a locating tool for nding a
DRS near you.
www.aded.net/custom/directory/
?pageid=209&showTitle=1
If a DRS is not available in your area, contact a
local driving school or your State’s Department of
Motor Vehicles to see if they can do a driving test.
* The acronym ADED was retained when the association
changed its name from the Association of Driver Educators
for the Disabled to its current name.
211Appendix B—Patient and Caregiver Educational Materials
How to help when your loved one
needs to stop driving.
At some point, your loved one may need to stop
driving for his/her own safety and the safety of oth-
ers. You and your family members may come to this
decision yourselves, or at the recommendation of
the doctor, a driver rehabilitation specialist, driving
instructor, or the Department of Motor Vehicles.
When someone close to you retires from driving,
there are several things you can do to make this
easier for him/her:
• Help create a transportation plan. It may be
easier for someone to give up driving if they are
aware of other ways to get around. Help them
create a list of “tried-and-true” ride options.
This list can include:
• The names and phone numbers of friends and
relatives who are willing to give rides, with the
days and times they are available. You should
even consider writing in specic duties, dates,
and times, with the places your loved one needs
to go and the name of the driver on a calendar
to make this a reality.
• The phone number of a local cab company.
• Which bus or train to take to get to a specic
destination. Try riding with your loved one the
rst time to make him/her feel comfortable.
(This may not be possible for many people with
physical weakness or arthritis and certainly
could not be done for those with memory or
thinking problems.)
• The phone number for a shuttle service.
Call your community center and regional
transit authority to see if they offer a door-to-
door shuttle service for older passengers.
• The names and phone numbers of volunteer
drivers. Call your community center, church, or
synagogue to see if they have a volunteer driver
program.
• If you need help nding other ride options,
contact your local Area Agency on Aging.
Local Agency on Aging
Assists in nding resources for the aging
in your community.
www.eldercare.gov
If your loved one can’t go shopping, help him/
her shop from home. Arrange for medicines and
groceries to be delivered. Explore online ordering
or subscribe to catalogs and “go shopping” at home.
Locate which services make house calls—local
hairdressers or barbers may be able to stop by for
a home visit.
Encourage social activities. Visits with friends,
time spent at the senior center, and volunteer work
are important for health and well-being. When cre-
ating a transportation plan, don’t forget to include
rides to social activities. It’s especially important to
maintain social contacts and keep spirits up during
this time of adjustment.
Be there for your loved one. Let the person you
care for know that he or she has your support.
Offer assistance willingly and be a good listener.
This may be an emotionally difcult time, and it’s
important to show that you care. You may need to
nd additional family members or friends to help
with this discussion.
213Appendix B—Patient and Caregiver Educational Materials
Getting By Without Driving
Who doesn’t drive?
If you live long enough, you will eventually have
to stop driving. The average male will have seven
years without the ability to drive, and the average
female ten years! Many people choose to stop
driving because of the hassle and expense of auto
insurance, car maintenance, and gasoline. Other
people stop driving because they feel unsafe on the
road. And some people have never learned
to drive!
If you don’t drive, you’re in good company.
Although most Americans use their cars to get
around, many people get by just ne without one.
In this sheet, we suggest ways to get by without
driving.
Where can you find a ride?
Here are some ways to get a ride. See which ones
work best for you.
• Ask for a friend or relative for a ride. Offer to
pay for the gasoline.
• Take public transportation. Can a train, subway
or bus take you where you need to go? Call your
regional transit authority and ask for directions.
• Take a taxi cab. To cut down costs, try sharing
a cab with friends or nd out if your community
offers discounted fares for seniors.
• Ride a senior transit shuttle. Call your com-
munity center or local Area Agency on Aging to
see if your neighborhood has a shuttle service.
• Ask about volunteer drivers. Call your commu-
nity center, church or synagogue to see if they
have a volunteer driver program.
• Ride a Medi-car. If you need a ride to your
doctor’s ofce, call your local Area Agency on
Aging to see if a Medi-car can get you there.
If you can’t go out to get something,
have it come to you.
Many stores can deliver their products straight to
your door.
• Have your groceries delivered. Many stores
deliver for free or for a low fee. You can even call
your family and friends, or volunteers from your
local community center, church or synagogue to
see if someone can pick up your groceries
• Order your medicines by mail. Not only is this
more convenient—it’s often less expensive, too.
Order only from pharmacies that you know and
trust. Some pharmacists will also deliver medica-
tions to the home.
• Have your meals delivered to you. Many
restaurants will deliver meals for free or for a
low fee. Also, you may be eligible for Meals-on-
Wheels, a program that delivers hot meals at low
cost. Call your local Area Agency on Aging for
more information about Meals-on-Wheels.
• Shop from catalogs. You can buy almost any-
thing you need from catalogs: clothing, pet food,
toiletries, gifts, and more! Many catalogs are
now on-line, with the most recent selections
available from Internet Web sites.
(over)
214 Appendix B—Patient and Caregiver Educational Materials
Who can tell me more about services
in my area?
The following agencies can provide you with
information to get you started:
Area Agency on Aging (AAA) Eldercare Locator
www.eldercare.gov
800-677-1116 weekdays
Call this toll-free number and ask for the phone
number of your local Area Agency on Aging
(AAA). Your local AAA can tell you more
about ride options, Meals-on-Wheels, and senior
recreation centers in your area.
Administration on Aging Resource Directory
for Older People
www.aoa.gov/eldfam/How_to_Find/
ResourceDirectory/ ResourceDirectory.pdf
800-222-2225
Call this toll-free number and ask the National
Institute on Aging to send you their Resource
Directory for Older People. This 120-page
directory lists organizations that provide
services for older people.
215Appendix B—Patient and Caregiver Educational Materials
Where Can I Find More
Information?
We’ve listed additional resources on the
following pages to help you assess and
enhance driving safety for the retired
driver. Some resources can help you
create a transportation plan for your
loved one.
National Association of Private
Geriatric Care Managers (NAPGCM)
520-881-8008
www.caremanager.org
A geriatric care manager can help
older people and their families arrange
long-term care, including transportation
services. Call the phone number or visit
the Web site above to nd a geriatric
care manager in your loved one’s area.
National Association of Social
Workers (NASW)
www.socialworkers.org/register/
default.asp
A social worker can provide counsel-
ing to your loved one, assess his/her
social and emotional needs, and assist
in locating and coordinating transporta-
tion and community services. To nd a
qualied clinical social worker in your
loved one’s area, search the NASW
Register of Clinical Social Workers on the
Internet.
Additional clinician, patient,
and caregiver resources
Clinician resources
American Occupational Therapy
Association (AOTA)
Information on occupational therapists
and their role in driving assessment and
rehabilitation.
www1.aota.org/olderdriver/
The Association for Driver
Rehabilitation Specialists (ADED*)
Information on the Association.
www.aded.net/i4a/pages/
index.cfm?pageid=1
Also provides a locating tool for nding
a DRS near you.
www.aded.net/custom/directory/
?pageid=209&showTitle=1
National Highway Trafc Safety
Administration
Many links to resources for
older drivers.
www.nhtsa.dot.gov
and
Adapting Motor Vehicles for People
with Disabilities
www.nhtsa.dot.gov/cars/rules/
adaptive/brochure/brochure.html
American Medical Association (AMA)
Physician’s Guide to Assessing and
Counseling Older Drivers
www.ama-assn.org/ama/pub/
category/10791.html
General older driver information
provided by the AMA.
www.ama-assn.org/ama/pub/
category/8925.html
CanDrive
Dementia and Driving Toolkit:
The Dementia Network of Ottawa
www.candrive.ca/En/
Physician_Resources/toolkit.asp
Canadian Medical Association (CMA)
Determining Medical Fitness to Oper-
ate a Motor Vehicle
CMA Driver’s Guide, 7th edition
www.cma.ca/index.cfm/ci_id/18223/
la_id/1.htm
Administration on Aging (AOA)
Information and resources for older
drivers.
www.aoa.gov
Summary of Internet resources
for the older driver.
www.aoa.gov/prof/notes/Docs/
Older_Drivers.doc
Insurance Institute for
Highway Safety (IIHS)
A frequently-updated site on older
driver laws for driver licensing.
www.iihs.org/laws/olderdrivers.aspx
Older Drivers: Fact Sheets
General information on the older driver
from the Centers for Disease Control
and Prevention, AARP and the Na-
tional Highway Trafc Safety Adminis-
tration.
www.cdc.gov/ncipc/factsheets/older.
htm
www.aarp.org/families/driver_safety/
www-nrd.nhtsa.dot.gov/Pubs/
809475.PDF
AAA Foundation for Trafc Safety
Older driver brochures.
Safe Driving For Mature Operators
(course).
www.seniordrivers.org/driving/
driving.cfm?button=publication&
selection=MO
Caregiver and patient resources
GrandDriver Program
Resources and information on other
older driver sites.
www.granddriver.info/
American Society on Aging
Information on DriveWell, an older
driver educational program that may be
offered in your community.
www.asaging.org/asav2/drivewell/
index.cfm
* The acronym ‘ADED’ was retained when the
association changed its name from the Associa-
tion of Driver Educators for the Disabled to its
current name.
216
The Association for Driver
Rehabilitation Specialists (ADED)
Information on the Association.
www.aded.net
Also provides a locating tool for nding
a DRS in your community.
www.aded.net/custom/directory/?pagei
d=209&showTitle=1
University of Michigan Transportation
Institute
Driving Decisions Workbook
A self-awareness guide to identify areas
of concern for older driver safety.
http://deepblue.lib.umich.edu/
handle/2027.42/1321
Alternative Transportation Options
American Administration on Aging
(AOA)
Eldercare locator
Assists in nding older adult resources
in your community.
www.eldercare.gov
Community Transportation
Association (CTAA)
Information on transportation in the
United States.
www.ctaa.org/ntrc/
American Public Transportation
Association (APTA)
Locate a local transportation provider
in your community.
www.publictransportation.org/systems/
Easter Seals
Transportation solutions for caregivers
www.easterseals.com/site/
PageServer?pagename=ntl_trans_care
National Center for Senior
Transportation
www.seniortransportation.net/
Local Agency on Aging
Assists in nding resources for the aging
in your community.
www.n4a.org/
Seniors on the MOVE
Assists with relocating to another
community.
www.seniorsonthemoveinc.com
New York Department for the Aging
When You Are Concerned—
A Handbook for Families, Friends,
and Caregivers
A handbook for those worried about the
safety of an aging driver.
http://aging.state.ny.us/caring/
concerned
AARP Driving Safety Program
The classic course with information on
how to locate an educational venue in
your community.
www.aarp.org/families/driver_safety/
wrapper_driver.py
Australia
Handbooks on older adults from the
provinces of Victoria and Tasmania in
Australia and the Australian Capital
Territory.
www.transport.tas.gov.au/licence_in-
formation_folder/the_tasmanian_old-
er_drivers_handbook?SQ_DESIGN_
NAME=printer_friendly
www.vicroads.vic.gov.au/NR/
rdonlyres/B15A81F1-2047-45B0-
821C-7AB3317029B6/0/victorianol-
derdrivershandbook5.pdf.
www.act.gov.au/living/roads/older/con-
tents.html
www.cota-act.org.au/Download_Docu-
ments/PDFS/Older_Drivers_Hbook_
web_0703.pdf
Drivers.com
General information on older drivers.
www.drivers.com/
Top_Older_Drivers.html
Mobilise
Disabled Drivers Information Website
(United Kingdom)
www.mobilise.info/Information.asp
American Occupational Therapy
Association (AOTA)
Information on occupational therapists
and their role in driving assessment and
rehabilitation.
www1.aota.org/olderdriver/
Road map to driving wellness.
Information on staying t.
www.asaging.org/CDC/module4/
home.cfm
Caregiver and patient resources
(continued)
AAA Foundation for Trafc Safety
Older driver brochures and the
Safe Driving For Mature
Operators course.
www.seniordrivers.org/driving/
driving.cfm?button=publication&
selection=MO
CarFit and General Information
www.seniordrivers.org/home/
toppage.cfm
RoadWise Review
www.roadwisereview.com/
University of Massachusetts Boston
Center for Gerontology
Keep moving longer: features for safe
driving. A video program that offers
advice on staying mobile.
www.geront.umb.edu/inst/projects/
promoting.jsp
National Highway Trafc Safety
Administration
Older Road Users; other older driver
information and materials.
www.nhtsa.dot.gov/people/injury/
olddrive
Driving Safely while Aging Gracefully
Reviews the skills and problems that
may face older drivers.
www.nhtsa.dot.gov/people/injury/
olddrive/Driving Safely Aging Web/
index.html
The Hartford
We Need to Talk
At the Crossroads: A Guide to
Alzheimer’s Disease, Dementia,
and Driving
State-of-the-art educational materials
for older drivers.
www.thehartford.com/
talkwitholderdrivers
www.thehartford.com/alzheimers/
brochure.html
217
Alternative Transportation Options
(continued)
National Association of Social
Workers (NASW)
Locate a social worker near you.
www.socialworkers.org/register/
default.asp
United We Ride
Coordination of transportation services.
www.unitedweride.gov
Research and Statistics
Federal Highway Administration
Information on older drivers
http://safety.fhwa.dot.gov/older_driver/
older_quiz.htm
Guidelines and recommendations to ac-
commodate older drivers and pedestrians.
Information on environmental design.
www.tfhrc.gov/humanfac/01105/
cover.htm
Older Road Users
General information on older drivers.
www.nhtsa.dot.gov/people/injury/old-
drive/
Research Agenda for Older Drivers
www.nhtsa.dot.gov/people/injury/
olddrive/pub/Chapter3.html
Safe Mobility for Older People: Model
Driver Screening and Evaluation
Program
www.nhtsa.dot.gov/people/injury/
olddrive/safe/
Further Analysis of Drivers Licensed
with Medical Conditions in Utah
www.nhtsa.dot.gov/people/injury/
olddrive/utah/utah_index.htm
The Road Information Program
(TRIP)
A research community on transportation.
www.tripnet.org
www.tripnet.org/
OlderDriversStudyOct2000.PDF
Older Driver Involvements in Police
Reported Crashes and Fatal Crashes:
Trends and Projections
Duke University Science News
http://unisci.com/stories/
20022/0624023.htm
Transportation Safety
Center for Injury Prevention Policy and
Practice
San Diego State University
www.injuryprevention.org/links/
links-trans.htm
AAA Foundation for Trafc Safety
Research on older driver safety
www.seniordrivers.org
Appendix B—Patient and Caregiver Educational Materials
Putting it all together.
Fill out the table below with names and numbers of services in your area. Keep this information at your ngertips by placing it
next to your phone or posting it on your refrigerator.
Service Phone number Cost

APPENDIX C
Continuing Medical
Education Questionnaire
and Evaluation

221
CME Questionnaire:
Instructions: The Physician’s Guide for Assessing and Counseling
Older Drivers contains the correct answers to the following
questions. Circle your answer to each question.
1. Compared to drivers age 25 to 69,
older drivers experience—
a. A higher fatality rate in motor vehicle crashes
b. A higher fatality rate per vehicle mile driven
c. A higher crash rate per vehicle mile driven
d. All of the above
2. The majority of older Americans do not rely on
driving as their primary form of transportation.
a. True
b. False
3. Compared to younger drivers, older drivers are more
likely to wear seatbelts and are less likely to drive at
night, speed, tailgate, and consume alcohol prior to
driving.
a. True
b. False
4. Medications that have the potential to impair driving
ability include—
a. Anticonvulsants
b. Antidepressants
c. Muscle Relaxants
d. a and b only
e. All of the above
5. Aspects of vision that are most important for safe
driving include—
a. Visual acuity
b. Visual elds
c. Contrast sensitivity
d. b and c only
e. All of the above
6. Match the cognitive skill to the appropriate
driving situation:
7. Research has demonstrated that drivers with 20/70 vi-
sual acuity have a signicantly greater crash risk than
drivers with 20/40 visual acuity.
a. True
b. False
8. All of the following are important for viewing the driv-
ing environment EXCEPT—
a. Visual acuity
b. Visual elds
c. Memory
d. Neck rotation
9. A Driver Rehabilitation Specialist (DRS) can—
a. Revoke a client’s drivers license for poor perfor-
mance on a clinical exam
b. Evaluate a client’s driving skills through an on-road
assessment
c. Assess the client’s vehicle and recommend adaptive
equipment to enhance the client’s comfort and driv-
ing safety
d. b and c only
e. All of the above
APPENDIX C
Physicians Guide to
Assessing and Counseling
Older Drivers
1. Applying the brake at a green
light because a child runs into
the path of your vehicle.
2. Listening to the trafc report
on the radio while keeping an
eye on the road.
3. Recalling that a particular
street is a one-way street.
4. Determining the distance
from your car to the stop sign.
___ Memory
___ Visuospatial skills
___ Divided attention
___ Executive skills
Appendix C—Physicians Guide to Assessing and Counseling Older Drivers
222 Appendix C—Physicians Guide to Assessing and Counseling Older Drivers
10. Driving cessation has been associated with an increase
in depressive symptoms in the elderly.
a. True
b. False
11. Which of the following is NOT recommended as
an initial technique to help your patients retire
from driving?
a. With the patient’s permission, involve family
members and caregivers.
b. Explain to the patient why you have recommended
that they retire from driving.
c. Provide your patient with information on
alternatives to driving.
d. Tell the patient’s relatives to hide the car keys.
12. ‘Physicians are required to report patients with
dementia to their state Department of Motor Vehicles’
is an example of—
a. Mandatory Medical Reporting Laws
b. Physician Reporting Laws
c. Physician Liability
d. None of the above
13. Physician-patient privilege can be used to prevent
physicians from abiding by their state’s Physician
Reporting Laws.
a. True
b. False
14. All states protect the identity of the individual who
reports an unsafe driver to the DMV.
a. True
b. False
15. Key functions that are important for safe driving
include—
a. Vision
b. Cognition
c. Motor function
d. a and b only
e. All of the above
16. What conditions are in part responsible for the increase
vulnerability to injury in a motor vehicle crash?
a. osteoporosis
b. atherosclerosis of
c. left-hand turn crashes
d. cars with no air bags
e. All of the above
17. What eye disease when treated has been shown to
lower crash risk in older adults?
a. glaucoma
b cataract
c. macular degeneration
d. diabetic retinopathy
e. All of the above
18. What neurological illness in late life carries the highest
crash risk for those that continue to drive?
a. Alzheimer’s Disease
b. Seizure disorder
c. Stroke
d. Brain Injury
19. Which of the following medications has been shown to
be associated with impaired driving?
a. Valium
b. Anti-depressants
c. Narcotics
d. Benadryl
e. All of the above.
20. Which of the following conditions carries the highest
crash risk?
a. a driver with a spinal cord affecting his arms and legs
that uses a joystick to drive
b. a stroke patient that has to use hand controls on the
steering wheel to drive
c. an amputee that uses hand controls on the steering
wheel to drive
d. an older adult with restricted neck range of motion
21. What are the most common road conditions when
older adults have crashes?
a. wet pavement, morning rush hour, and going
up a hill
b. dry pavement, mid-morning, on a at roadway
c. snowy weather, at night, going around a curve
d. icy conditions, at night, trying to pass another
vehicle
22. What vehicle modications have been shown to reduce
crashes or injuries?
a. infrared brakes
b. side air bags
c. enlarged side view mirrors
d. On-STAR
e. All of the Above
223Appendix C—Physicians Guide to Assessing and Counseling Older Drivers
23. What is true about laws for reporting unsafe drivers?
a. Physicians prefer to have civil immunity for protec-
tion and anonymity when reporting
b. States with mandatory reporting laws appear to have
higher number of reports
c. Physicians have been sued for not reporting unsafe
drivers and they have been sued for reporting.
d. Almost all states require a physician evaluation for
medical tness-to-drive if a driver is reported to the
state authorities as being unsafe
e. All of the above
24. What types of crash scenarios are common for
older adults?
a. high speed crashes
b. low speed and/or left hand turn crashes
c. head-on collisions
d. failure to yield
e. Answer B, D
25. What common medical condition is often undiag-
nosed and likely carries the highest crash rate if
left untreated?
a. Sleep apnea
b. Alzheimer’s Disease
c. Diabetes Mellitus
d. Parkinson’s Disease
Please print and include all information requested.
Name and title _________________________________________________________________________________________
Address _______________________________________________________________________________________________
City _______________________________________________________ State _____ Zip _____________________________
Phone ( ) ________________________________Fax ( ) ________________________________________
E-mail ________________________________________________________________________________________________
Medical specialty _______________________________________________________________________________________
Please mail the completed form to:
Lela Manning, MPH, MBA
Project Coordinator, Older drivers Project
American Medical Association
515 N. State Street
Chicago, IL 60654
(312) 464-4111 (Fax)
224
Please complete this evaluation by circling your response or writing your
comments in the spaces provided.
Overall Impression
1. I feel I can dene the safety risks of older drivers as a public health issue.
Strongly agree Agree Undecided Disagree Strongly disagree
2. This guide is a useful and effective physician education tool.
Strongly agree Agree Undecided Disagree Strongly disagree
3. This guide has raised my awareness of driving as a public safety issue.
Strongly agree Agree Undecided Disagree Strongly disagree
4. I have a better understanding of the medical conditions and medications that may impair my patient’s ability to
drive safely.
Strongly agree Agree Undecided Disagree Strongly disagree
5. I feel comfortable identifying patients who may be at risk for unsafe driving.
Strongly agree Agree Undecided Disagree Strongly disagree
6. I feel comfortable using the various clinical screens to assess patients’ level of function for driving tness.
Strongly agree Agree Undecided Disagree Strongly disagree
7. I feel comfortable using counseling techniques for patients who are no longer t to drive.
Strongly agree Agree Undecided Disagree Strongly disagree
8. I have a better understanding of driver rehabilitation options and alternatives to driving.
Strongly agree Agree Undecided Disagree Strongly disagree
9. I feel comfortable utilizing referral and treatment options for patients who are no longer t to drive.
Strongly agree Agree Undecided Disagree Strongly disagree
10. I have a better understanding of my state’s reporting laws and legal/ethical issues surrounding patients who may not
be safe on the road.
Strongly agree Agree Undecided Disagree Strongly disagree
As a result of participating in this educational activity:
❏ I will change my practice How? ____________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
Continuing Medical Education
Evaluation Form
Appendix C—Physicians Guide to Assessing and Counseling Older Drivers
225
❏ I will not change my practice ______________________________________________________________________ Why?
❏ This activity reinforced my current practice __________________________________________ ❏ Other (please explain)
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
I perceived commercial bias in this activity. (“Commercial bias” is dened as a personal judgment in favor of a specic proprietary
business interest of an entity that produces, markets, sells or distributes healthcare goods or services consumed by, or used on, patients.)
❏ Yes ❏ No If yes, please comment: ______________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
Please the usefulness of the following guide materials on a scale of 1 to 5.
1. Physicians’ Plan for Older Drivers’ Safety (PPODS) Very useful 1 2 3 4 5 Not useful at all
2. Red Flags for Further Assessment Very useful 1 2 3 4 5 Not useful at all
3. Assessment of Driving-Related Skills (ADReS) Very useful 1 2 3 4 5 Not useful at all
4. State Licensing and Reporting Laws (Chapter 8) Very useful 1 2 3 4 5 Not useful at all
5. Medical Conditions that May Affect Driving (Chapter 9) Very useful 1 2 3 4 5 Not useful at all
6. Patient Education Materials (Appendix) Very useful 1 2 3 4 5 Not useful at all
Please include any additional comments you feel would be helpful.
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
Only physician participants (MD, DO, or equivalent international medical degree) are eligible to receive AMA PRA Category
1 Credit™. Physicians will receive a certicate of credit, indicating one credit for each hour of participation, rounded to the
nearest quarter credit (or hour). Physicians must complete this form to receive AMA PRA Category 1 Credit.
Non-physician participants may complete this form to obtain a certicate of participation indicating that this activity was
approved for AMA PRA Category 1 Credit.
Check one: ❏ Physician: Certicate of Credit ❏ Non-physician: Certicate of Participation
FOR PHYSICIANS ONLY. Please check one below:
❏ U.S. Licensed Physician Medical Education Number*: __________________________________________
❏ Non-U.S. Licensed Physician Date of Birth (mm/dd/yyyy)**: _________________________________________
Specialty: _____________________________________________________________________________________________
Please Send Completed Questionnaires and Evaluation Forms to: Lela Manning, MPH, MBA
Project Coordinator
Older Drivers Project
American Medical Association
515 N. State Street
Chicago, IL 60654
(312) 464-4111 (Fax)
Appendix C—Physicians Guide to Assessing and Counseling Older Drivers

Index

229Index
A
AAA Foundation for Trafc Safety,
Safe Driving for Mature Operators course ........................ 208
AARP Driving Safety Program ........................................ 208
Accommodation and adaptation of lens of eye .................. 22
Acute events of older drivers
conditions requiring counseling associated with, ........... 15
counseling following ....................................................... 13
red ags for further assessment after .................... 11, 14–15
Adaptive devices, vehicle ............................... 36, 37, 42, 155
Additional resources for driving safety ..................... 215–217
Administration on Aging Resource Directory for Older
People ................................................................................ 214
Adult protective services (APS) ........................................ 55
Affective disorders ............................................................ 163
Alabama, licensing and reporting procedures in ................ 71
Alaska, licensing and reporting procedures in ................... 72
Alcohol ............................................................. 164, 178, 179
Alzheimer’s Association ...................................................... 43
Policy Statement on Driving and Dementia by ............... 158
Alzheimer’s disease. See also Dementia
evaluation by another health professional
for patient with ................................................................ 45
mandatory reporting of drivers with ............................... 62
repeat driving tests for patients with ............................. 157
AMA Ethical Opinion E-2.24,
“Impaired Drivers and Their Physicians” ........................... 62
Am I a Safe Driver? ..................................................... 20, 203
American Academy of Neurology recommendations ...... 157
American Association of Motor Vehicle Administrators
(AAMVA), study by NHTSA and ........................... 189–190
American Occupational Therapy Association (AOTA) . 188
Amputation ....................................................................... 169
Anesthesia and surgery ............................................. 175–176
Angular movement vision test ........................................... 22
Anterior cruciate ligament (ACL) reconstruction .......... 169
Anterograde amnesia ........................................................ 178
Anticholinergics ............................................................... 179
Anticonvulsants ................................................................ 180
Antidepressants ................................................. 178, 180–181
Antiemetics ............................................................... 178, 181
Anti-epileptic drug therapy ...................................... 161, 178
Antihistamines ......................................................... 178, 182
Antihypertensives ............................................................. 182
Antiparkinsonians ............................................................ 182
Antipsychotics .................................................. 178, 182–183
Anxiety disorders ...................................................... 162, 163
Aortic aneurysm ................................................................ 171
Area Agency on Aging ............................................. 211, 214
Arizona, licensing and reporting procedures in ............ 69, 73
Arkansas, licensing and reporting procedures in ................ 74
Arthritis ............................................................................ 168
Assessment of driving-related skills (ADReS)
case study of scores on ..................................................... 33
cognitive skill ................................................ 23–25, 34–36
CPT codes for ....................................................... 21, 27, 198
discussion of results of ..................................................... 50
import of impairment in functions tested by .................. 21
motor and sensory function ................................. 26, 36–37
repeat administration of .................................................. 38
score sheet for ............................................................ 27–30
sequence of test administration in .................................. 27
use of ................................................................................ 61
vision ....................................................... 21–22, 27, 33–34
Association for Driver Rehabilitation Specialists (ADED)
certication of DRSs by .................................................. 41
online directory of ........................................................... 43
referrals to DRS by ........................................................ 210
Asthma .............................................................................. 173
Atrial utter/brillation .................................................... 152
Atrio-ventricular (AV) block, high grade ........................ 153
Attentional functioning ..................................................... 24
Attention decit disorder/
attention decit hyperactivity disorder .................... 162, 164
Automatic transmission, encouraging
use of vehicle having .................................................. 37, 167
B
Barbiturates ............................................................... 167, 178
Benzodiazepines and other sedatives/anxiolytics...... 178, 183
Bipolar disorder ................................................................. 163
Blepharospasm .................................................................. 149
Blurred vision. See Visual acuity
Brain tumor ....................................................................... 158
Bupropion ......................................................................... 180
C
California
licensing and reporting procedures in ....................... 75–76
mandatory reporting requirements
of medical impairments in ............................................... 62
Canadian Consensus Conference on Dementia ............... 158
Cancer ............................................................................... 177
Cardiac arrest .................................................................... 153
Cardiac surgery involving median sternotomy ................. 154
Cardiovascular diseases ............................................. 151–154
Index
230 Index
Cardioverter debrillator, internal ................................... 154
CarFit program .................................................................... 44
Caregiver burnout ............................................................... 51
Case study of dementia patient (Allen)
diagnosis of Alzheimer’s disease for ................................. 59
report of driving issues by daughter of............................. 49
state notication requirements for .................................. 59
Case study of older driver (Clayton Phillips)
assessment of functional capabilities of........................... 19
follow-up counseling in ................................. 41, 49, 50, 52
observation of driving risk and existing conditions of .... 11
performance on ADReS of .............................................. 33
physician letter for driving cessation in .......................... 56
referral to DRS in ...................................................... 41, 44
Cataracts ........................................................................... 147
Central nervous system (CNS) ........................................ 178
Cerebrovascular disorders ......................................... 155–156
Certied driver rehabilitation specialists (CDRSs) ........... 41
Cervical movement limitations ........................................ 168
Chronic conditions, driving safety for patients having
formal assessment of ........................................................ 13
red ags for further assessment in .................................... 11
Chronic obstructive pulmonary disease (COPD) ............ 173
Chronic renal failure ......................................................... 172
Civil damages, protection against ....................................... 62
Clock Drawing Test (CDT) .......................................... 24, 27
correlation with impaired driving performance of .......... 35
score sheet for .................................................................. 29
Cognitive domains .............................................................. 25
Cognitive skills
identifying cause of decline in......................................... 35
tested for driving ............................................... 23–25, 153
tested to diagnose dementia .......................................... 157
Colorado, licensing and reporting procedures in ......... 69, 77
Color detection in vision test ............................................. 22
Color vision, defective ...................................................... 150
Compliance with driving cessation .................................... 63
Condentiality issues. See Patient condentiality
Congestive heart failure (CHF) ........................................ 154
Connecticut, licensing and reporting procedures in .... 78–79
Contrast sensitivity ............................................................. 21
correlation with crash risk of......................................... 189
denition of ................................................................... 150
red ags for further assessment with ................................ 14
Copiloting ........................................................................... 36
Counseling for patient not safe to drive ....................... 49–56
key points addressed in .................................................... 49
by physicians, fullling duty in ................................. 62, 63
to prepare for driving cessation ..................................... 157
situations requiring additional .......................... 53–55, 146
by social worker ............................................................... 54
CPT codes for driver assessment and counseling ..... 197–198
in functional abilities testing of ADReS ........... 21, 27, 198
new ................................................................................ 198
for preventive medicine services ................................... 197
Crash risk
cardiac disease and ........................................................ 151
contrast sensitivity correlated with ............................... 189
detection of impairment correlated with ........................ 24
increases in, physical frailty and...................................... 26
medications associated with .................................. 167, 178
musculoskeletal disorders correlated with ..................... 167
visual testing and ....................................................... 33, 69
D
Deep vein thrombosis (DVT) ........................................... 171
Delaware
licensing and reporting procedures in ............................. 80
mandatory reporting requirements of
medical impairments in ................................................... 62
Dementia. See also Alzheimer’s disease
cessation of driving by patient having .................... 36, 159
cognition affected by ....................................................... 26
correlation with impaired driving performance
of degenerative ................................................................ 35
detection of...................................................................... 35
incidence of ..................................................................... 36
family involvement in deciding risk level from ............ 158
lack of decision-making capacity in ........................ 54, 157
test results of patients with ...................................... 35, 157
Department of Motor Vehicles (DMV)
driving assessment by ...................................................... 45
form for reporting medical condition(s) to ..................... 63
physician reporting requirements for ................ 52, 59, 189
self-reporting of impairment to ....................................... 52
state laws for driving safety of ......................................... 20
Depression ......................................................................... 163
discussing symptoms of .................................................... 54
questions to assess ............................................................ 54
signs of ............................................................................. 52
Depth perception vision test .............................................. 22
Diabetes mellitus ............................................................... 165
Diplopia ............................................................................. 150
District of Columbia, licensing and
reporting procedures in ................................................. 81–82
Doctor-patient relationship. See Patient-physician
relationship
Driver rehabilitation, increased availability of ......... 187–188
Driver rehabilitation specialist (DRS) ......................... 41–45
barriers to using ............................................................. 187
certication of ................................................................. 41
clients of .......................................................................... 42
clinical assessment by ...................................... 42, 155, 187
consulting ............................................................ 19, 20, 65
costs of services by ........................................................... 43
denition of ..................................................................... 41
on-road assessment by ..................... 34, 35, 37, 38, 42, 167
physician use of ............................................................. 188
prescription of adaptive devices by ......................... 37, 145
referral to ....................................... 33, 36, 38, 44, 155, 167
refusal of assessment by ................................................... 44
report by, physician documentation of ............................ 63
231Index
selecting, questions to ask in ..................................... 43–44
services provided by................................................. 42, 145
sources for nding ...................................................... 43–44
Driver retraining ................................................................. 42
Driving assessment. See also Driver rehabilitation specialist
(DRS)
age-based ......................................................................... 69
discussion of results of ............................................... 50–53
by non-DRS individual ............................................. 44–45
patient refusal to take ...................................................... 20
purpose in driving as inuencing .................................. 146
ways to suggest ................................................................. 19
Driving cessation
counseling to prepare for ....................................... 157, 159
losses from........................................................................ 49
view as step in health promotion of ................................ 54
Driving cessation recommendation .............................. 38, 42
basis of ................................................................. 45, 62–63
documenting .............................................................. 63, 64
economic arguments supporting ..................................... 52
medication use prompting ............................................. 145
for patients having dementia .......................................... 36
reasons physicians avoid making ..................................... 49
reinforcement of ........................................................ 51–52
Driving Decisions Workbook ............................................. 20
Driving educational specialists ........................................... 45
Driving Health Inventory (DHI) ................................. 24–25
Driving safety addressed in diagnosis/treatment plan ........ 15
Driving School Association of the Americas, Inc. ........... 208
Drowsiness, medications causing ...................................... 178
Duty to protect as physician responsibility ................... 59–60
E
Early Treatment Diabetic Retinopathy Study (ETDRS) ... 22
Educational materials for
patient and caregiver .................... 20, 44, 192–193, 201–217
Eldercare Locator .......................................... 51, 55, 211, 214
Epilepsy ............................................................... 61, 160–161
Ethical and legal responsibilities for reporting ............. 59–66
situations involving ................................................... 63–65
Ethical opinion E-2.24,
“Impaired Drivers and Their Physicians” (AMA) ............. 62
Euphoria, medications causing ......................................... 178
Executive skills, uses in driving of ...................................... 26
Extremities, loss of or loss of use of ................................... 168
Eyesight. See Visual acuity
F
Family member or caregiver
assistance with physician’s evaluation by ................ 35, 158
counseling, patient permission for .................................. 62
transportation plan developed with involvement of ...... 51
Family member’s concerns about patient’s driving safety
further assessment addressing .......................................... 14
How to Assist the Older Driver addressing ........................ 20
Federal Highway Administration (FHWA) ..................... 191
Five A’s of Senior-Friendly Transportation ............... 191, 192
Florida, licensing and reporting procedures in ....... 61, 83–84
Follow-up appointment following
driving cessation recommendation ............................... 52–53
Food and Drug Administration (FDA),
meeting by NTSB and ...................................................... 190
Foot abnormalities ............................................................ 168
Freund Clock Scoring Criteria ........................................... 35
Functional ability
assessing older driver’s ............................................... 17–30
detailed history and examination of ............................... 35
G
Geographic orientation ...................................................... 25
Georgia, licensing and reporting procedures in .................. 85
Getting By Without Driving .................................... 213–214
Glaucoma .......................................................................... 149
Glossary of terms for state licensing
and reporting laws ......................................................... 65–66
H
Hawaii, licensing and reporting procedures in ................... 86
Head injury, closed ............................................................ 158
Health Insurance Portability and Accountability
Act of 1996 (HIPAA)
patient rights and condentiality issues under.......... 60–61
reporting protected health information under ................ 62
Health risk assessment of older driver
conditions requiring ........................................................ 14
denition of ..................................................................... 12
inquiries about driving in .......................................... 12–13
Hearing loss ....................................................................... 151
Hemianopia/quadrantanopia ............................................ 149
Highway Design Handbook for
Older Drivers and Pedestrians .......................................... 191
Hip replacement, total ...................................................... 169
How to Assist the Older Driver .................... 20, 51, 209–211
Hypertension ..................................................................... 151
Hyperthyroidism ............................................................... 166
Hypertrophic obstructive cardiomyopathy ....................... 154
Hypnotics .......................................................................... 178
Hypothyroidism ................................................................ 166
I
Idaho, licensing and reporting procedures in ..................... 87
Illinois, licensing and reporting procedures in ............. 88–89
Independent transportation network (ITN) model ......... 191
Indiana, licensing and reporting procedures in ............ 90–91
Inpatient setting, counseling driver in ............................... 12
Insulin dependent diabetes mellitus (IDDM) .................. 165
232 Index
Insurance Information Institute ......................................... 70
Insurance Institute for Highway Safety .............................. 70
Iowa, licensing and reporting procedures in ....................... 92
K
Kansas, licensing and reporting procedures in ................... 93
Kentucky, licensing and reporting procedures in ............... 94
Keratoconus ...................................................................... 148
Knee arthroplasty, total (TKA) ........................................ 170
L
Language skills for driving .................................................. 25
Lawsuit by patient ................................................... 59, 63–64
Liability protection for physician,
state legislation for ...................................................... 64, 189
License renewal practices
international .................................................................... 70
for older drivers ............................................................... 69
state ........................................................................... 69–70
Licensing agencies, role in driving safety of.
See also Department of Motor Vehicles (DMV).......189-190
Licensing and unsafe driver reporting laws,
state-by-state descriptions of ................................. 45, 69–141
Limb fractures ................................................................... 169
Listening to patient’s concerns ........................................... 53
Local Agency on Aging .................................................... 211
Loss of consciousness, cardiac conditions causing .... 152–153
Louisiana, licensing and reporting procedures in ............... 95
M
Macular degeneration ....................................................... 148
Maine, licensing and reporting procedures in .................... 96
Mandatory tness-to-drive reporting requirements
for physicians
compliance with ........................................................ 63, 64
states requiring ................................................................ 62
Manual Test of Motor Strength .................................... 25, 27
results of ..................................................................... 36–37
Manual Test of Range of Motion test ........................... 25, 27
scoring of ......................................................................... 37
Maryland, licensing and reporting procedures in ............... 97
Massachusetts, licensing and reporting procedures in .. 98–99
Medical Advisory Board ........................................... 189–190
Alabama .............................................................................. 71
Arizona ................................................................................ 73
California ............................................................................ 76
Connecticut ........................................................................ 79
Delaware ............................................................................. 80
Florida ................................................................................. 84
Georgia ................................................................................ 85
Hawaii ................................................................................. 86
Idaho ................................................................................... 87
Illinois ................................................................................. 89
Indiana ................................................................................ 91
Iowa ..................................................................................... 92
Kansas ................................................................................. 93
Kentucky ............................................................................. 94
Louisiana ............................................................................. 95
Maine .................................................................................. 96
Maryland ............................................................................. 97
Massachusetts ...................................................................... 99
Michigan ........................................................................... 101
Minnesota ......................................................................... 102
Mississippi ......................................................................... 103
Missouri ............................................................................. 105
Nebraska ........................................................................... 108
Nevada .............................................................................. 109
New Jersey ......................................................................... 111
New Mexico ...................................................................... 112
New York........................................................................... 114
North Carolina ................................................................. 115
North Dakota .................................................................... 116
Oklahoma ......................................................................... 119
Oregon .............................................................................. 121
Pennsylvania ..................................................................... 123
Rhode Island ..................................................................... 124
South Carolina .................................................................. 125
South Dakota .................................................................... 126
Tennessee .......................................................................... 127
Texas ................................................................................. 129
Utah .................................................................................. 131
Virginia ............................................................................. 134
West Virginia .................................................................... 137
Wisconsin .......................................................................... 139
Medical conditions that may affect driving .............. 146–177
Medication dose, reducing ................................................ 145
Medications interfering with
driving performance ............................................ 37, 178–184
Medications review for patient ............................... 11–12, 35
Medications, side effects of ......................................... 26, 178
public awareness of, increasing ..................................... 190
review of .......................................................................... 35
Medications with strong potential to affect
driving safety ............................................................. 145–184
types of ............................................................................. 15
Memory tests ................................................................. 23, 24
Metabolic disorders ................................................... 165–166
Michigan, licensing and reporting
procedures in ....................................................... 69, 100–101
Migraine headaches .......................................................... 159
Minnesota, licensing and reporting procedures in ........... 102
Mirtazapine ....................................................................... 180
Mississippi, licensing and reporting procedures in ........... 103
Missouri
license retention following evaluations in ...................... 61
licensing and reporting procedures in ................... 104–105
Mobility needs of patient .................................................... 13
Model Driving Impairment Law ......................................... 62
Monoamine oxidase (MAO) inhibitors ........................... 181
233Index
Monocular vision .............................................................. 149
Montana, licensing and reporting procedures in .............. 106
Motor abilities for operating vehicle .................................. 26
results of tests of .............................................................. 36
Motor Strength, manual test of .................................... 25, 27
score sheet for .................................................................. 28
Movement disorders .......................................................... 159
Multiple sclerosis .............................................................. 159
Muscle disorders ................................................................ 169
Muscle relaxants ............................................... 167, 178, 183
Musculoskeletal disabilities ................................ 26, 167–170
N
Narcolepsy ......................................................................... 161
Narcotic analgesics ........................................................... 184
Narcotics ........................................................................... 167
National Association of Social Workers Register of Clinical
Social Workers .................................................................... 54
National Family Caregivers Association (NCFA) ............. 51
National Highway Trafc Safety Administration (NHTSA)
data on medically impaired drivers ................................. 61
meeting by FDA and ..................................................... 190
study by AAMVA and .......................................... 189–190
Nebraska, licensing and reporting procedures in ..... 107–108
Neglect or self-neglect
adult protective services to address ................................. 55
signs of ............................................................................. 54
Neurologic diseases ................................................... 157–162
Nevada
licensing and reporting procedures in ........................... 109
mandatory reporting requirements of
medical impairments in ................................................... 62
New Hampshire, licensing and reporting
procedures in ..................................................................... 110
New Jersey
licensing and reporting procedures in ........................... 111
mandatory reporting requirements of
medical impairments in ................................................... 62
New Mexico, licensing and reporting procedures in ........ 112
New York, licensing and reporting procedures in..... 113–114
Night vision
medications affecting .................................................... 178
poor ................................................................................ 150
N-methyl d-aspartate (NMDA) receptor blockers ........... 157
Non-insulin dependent diabetes mellitus (NIDDM) ....... 165
Nonsteroidal anti-inammatory agents (NSAIDs) .......... 167
possible effects on driving of ......................................... 183
North Carolina, licensing and reporting procedures in ... 115
North Dakota, licensing and reporting procedures in ...... 116
Nystagmus ......................................................................... 148
O
Observations of patient throughout ofce visit .................. 11
Occupational therapists off-road tests
and/or mobility counseling by ............................................ 44
Occupational therapy (OT) profession ............................ 188
Ohio, licensing and reporting procedures in ...... 69, 117–118
Oklahoma, licensing and reporting procedures in ........... 119
Older drivers
educational materials for ................................. 20, 201–217
increasing number of ......................................................... 1
optimal environments for .............................................. 191
plans for alternate transportation of ..................... 187–193
vehicle designs to improve safety of ...................... 190–191
Oregon
licensing and reporting procedures in ................... 120–121
mandatory reporting requirements of
medical impairments in ................................................... 62
reports of medically impaired drivers in .......................... 61
Orthopedic procedures/surgeries ............................... 169–170
Osteoarthritis .................................................................... 167
P
Pacemaker insertion or revision ....................................... 154
Paraplegia, adapted vehicle for driving with .................... 159
Parkinson’s disease .................................................... 159–160
Paroxysmal supraventricular tachycardia (PSVT) ........... 152
Patient concerns about driving safety ................................. 14
Patient condentiality
exceptions to maintaining............................................... 62
in impaired driver situations ....................... 60–61, 64, 189
reducing impact of breaching .......................................... 62
Patient-physician relationship
condentiality of health information in ................... 60, 61
effects of reporting tness to drive reports on ........... 61–62
reducing impact of breach of condentiality on ............. 63
Pedestrians, optimal environments for ............................. 191
Pennsylvania
licensing and reporting procedures in ................... 122–123
mandatory reporting requirements of
medical impairments in ................................................... 62
provider compliance in ....................................... 59–60, 61
Percutaneous transluminal coronary
angioplasty (PTCA) ......................................................... 154
Peripheral arterial aneurysm ............................................. 171
Peripheral neuropathy ...................................................... 160
Peripheral vascular diseases .............................................. 171
Personality disorders ......................................................... 164
Physical activity regimen ............................................ 37, 167
Physician assessment tools for effects on driving ............. 1–2
future improved ............................................................. 187
Physician documentation of patient’s driving ability ... 20, 63
Physician intervention .................................................. 33–38
cognitive abnormal results prompting ...................... 34–35
course of action for .................................................... 37–38
234 Index
documenting .................................................................... 63
motor ability results prompting ....................................... 36
summary of ...................................................................... 63
visual acuity results prompting .................................. 33–34
visual eld loss prompting ............................................... 34
Physician-patient privilege
denition of ..................................................................... 64
as not preventing report to DMV ................................... 64
Physician responsibilities for reporting unsafe driver
DMV requirements as ............................................. 52, 59, 63
ethical and legal ........................................................ 59–66
when state has no reporting laws .................................... 64
Physician’s Plan for Older Drivers’ Safety (PPODS)
algorithm of ................................................................. 6, 19
documenting steps of ....................................................... 63
formal assessment in ............................................ 19–29, 63
observation in ...................................................... 11–15, 63
Physician, threat by unsafe-driving patient
to nd another .............................................................. 64–65
Polypharmacy .................................................................... 179
Post intracranial surgery ................................................... 155
Potential driving impairing (PDI) medications ............... 178
Power steering, recommending use of
vehicle providing ........................................................ 37, 167
Prescription reinforcement stating “Do Not Drive” ..... 51, 52
Pre-syncope or syncope, risk of ................................. 153–154
Psychiatric disorders .................................................. 163–164
Psychotic illness ................................................................ 164
Ptosis or lid redundancy .................................................... 149
Public safety ........................................................................ 60
Public transportation statistics ......................................... 191
Q
Quadriplegia, adapted vehicle for driving with ................ 159
R
Range of motion ................................................................. 26
manual test of ............................................................ 25, 27
score sheet for .................................................................. 28
Rapid Pace Walk test .................................................... 24, 27
correlation between future at-fault crash and performance
on ..................................................................................... 36
functions assessed by ....................................................... 36
score sheet for .................................................................. 28
Referral of patient for tness-to-drive evaluation
to DRS ................................................... 33, 36, 38, 44, 167
physicians’ condentiality concerns in ..................... 61–62
physicians’ problems with ............................................... 61
retention of license following ......................................... 61
Referral of patient to DMV for testing ......................... 20, 45
Release of information, patient consent for ....................... 62
Renal disease ..................................................................... 172
Renal transplant ................................................................ 172
Renewal rates for licenses ............................................. 69–70
Resources, driving safety ..................................... 20, 215–217
CarFit .................................................................................. 44
DRS ............................................................................... 43–33
handout ................................................................. 201–217
Resources, mobility needs ......................................... 192–193
Respiratory diseases ................................................... 173–174
Restricted driving .................................................... 34, 38, 42
for cardiac conditions .................................................... 154
medication use prompting ..................................... 145, 178
recommendation basis for ............................................... 45
Retinitis pigmentosa ......................................................... 149
Review of systems (ROS)
comprehensive................................................................. 12
symptoms affecting driving safety revealed by ................ 15
Rhode Island, licensing and reporting procedures in ....... 124
Ride-sharing statistics ....................................................... 191
Roadwise Review CD of AAA ........................................... 20
Rotator cuff repair ............................................................. 169
S
Safe Driving Tips ................................................................ 45
SAFER Driving survey ........................................................ 20
Safety features, new vehicular .......................................... 191
Safety of older driver having functional
or medical impairments
examples of issues for ............................................. 1, 11, 19
overview of .................................................................... 1–7
Seizure disorder ......................................................... 160–161
Selective serotonin reuptake inhibitors (SSRIs) .............. 181
Self-awareness and self-regulation of driving safety ......... 190
Self-screening tool, Am I a Safe Driver? .................... 20, 203
Sensory deprivation conditions ................................ 147–151
Shopping from home ........................................................ 211
Shoulder reconstruction ................................................... 169
Sick sinus syndrome .......................................................... 153
Simulators, driving ............................................................ 188
Sinus brachycardia/sinus exit block/sinus arrest ............... 153
Sleep apnea ....................................................................... 174
Sleep disorders .......................................................... 161, 174
Snellen E chart test of visual acuity ............................. 22, 27
Social history/health risk assessment, driving on ............... 12
South Carolina, licensing and reporting procedures in 69, 125
South Dakota, licensing and reporting procedures in ...... 126
Spine limitations, thoracic or lumbar ............................... 168
State laws for referrals to DMV .............................. 20, 45, 52
compliance with .............................................................. 63
State licensing and physician reporting laws ........ 45, 69–141
Stimulants ......................................................................... 184
Stroke .................................................................. 61, 155–156
Subarachnoid hemorrhage ................................................ 156
Substance abuse ........................................................ 164, 179
Successful Aging Tips ................................... 20, 45, 205–206
Support systems ................................................................... 53
Surgery, abdominal, back, and chest................................. 175
Suspension of driver’s license, driving subsequent to ......... 64
Syncope ..................................................................... 153–154
effects on driving of ....................................................... 156
235Index
T
Taxi use statistics ............................................................... 191
Telescopic lens .................................................................. 148
Tennessee, licensing and reporting procedures in ............ 127
Texas, licensing and reporting procedures in ........... 128–129
Tips for Safe Driving ........................................... 20, 207–208
Tourette’s syndrome .......................................................... 162
Trafc Safety Course (AARP) ............................................ 20
Trail-marking test, Part B ............................................. 23, 27
driving performance on ............................................. 34–35
score sheet for ............................................................ 29, 30
Transient ischemic attacks (TIA) .................................... 156
Transportation alternatives
discussed with patient ....................................... 50–51, 146
follow-up of patient’s success using ................................. 63
future plans for....................................................... 187–193
list of ................................................................................ 50
Transportation needs of older adults ......................... 187–193
Tricyclic antidepressants (TCAs) ..................................... 181
U
Unsafe drivers
identifying ..................................................................... 188
patient’s recognition of .................................................... 53
referral requirements of providers for .............................. 20
reporting. See Physician responsibilities for reporting
unsafe driver
Unstable coronary syndrome ............................................ 152
Useful Field of View (UFOV) ............................................. 24
U.S. Public Health Service guidelines on musculoskeletal
ability and driving ............................................................... 37
Utah, licensing and reporting procedures in ............ 130–131
V
Valvular disease ................................................................. 154
Vascular malformation ...................................................... 156
Vehicle designs to optimize safety ............................ 190–191
Vehicle modication ....................................... 36, 37, 42, 155
Ventricular tachycardia (VT)
prolonged, nonsustained ............................................... 152
sustained ................................................................ 152–153
Vermont, licensing and reporting procedures in, 132
Vertigo ............................................................................... 162
Vigilance (sustained attention) .......................................... 25
Virginia, licensing and reporting procedures in ....... 133–134
Visual acuity
correlation with crash risk of........................................... 33
frequency of assessing ...................................................... 34
greater than 20/40 ..................................................... 33–34
lessening impact on driving of decreased ...................... 147
less than 20/70 ................................................................. 34
less than 20/100 ............................................................... 34
medical conditions decreasing .............................. 147–148
medications affecting .................................................... 178
state requirements for drivers’ ................................... 33, 69
in vision assessment................................................... 21–23
Vision assessment, visual acuity and visual elds in ..... 21–23
Visual Fields by Confrontation test .............................. 23, 27
Visual elds deterioration ................................................... 34
medical conditions causing ................................... 148–149
Visual perception, visual processing, and
visuospatial skills ........................................................... 23–24
Voluntary reporting laws, liability of
physicians in states having .................................................. 62
W
Walking ......................................................................... 26, 36
Washington, licensing and reporting
procedures in ............................................................. 135–136
“We Need to Talk” (Harford) ........................................... 210
West Virginia, licensing and reporting procedures in ...... 137
Wisconsin, licensing and reporting procedures in .... 138–139
Wolf-Parkinson-White (WPW) syndrome ...................... 152
Wyoming, licensing and reporting procedures in ............. 140
PD102:10-0193:PDF:4/10:DF
